EXHIBIT 10.1
Published on January 20, 2017
Exhibit 10.1

|
 |
Centers for Medicare & Medicaid Services
Center for Medicare and Medicaid Innovation
Seamless Care Models Group
7205 Windsor Blvd
Baltimore, MD 21244
Next Generation ACO Model
Participation Agreement
Last Modified: December 15, 2016
Contents
| I. | Agreement Term and Renewal | 6 | |
| II. | Definitions | 7 | |
| III. | ACO Composition | 12 | |
| A. | ACO Legal Entity | 12 | |
| B. | ACO Governance | 12 | |
| 1. | General | 12 | |
| 2. | Composition and Control of the Governing Body | 13 | |
| 3. | Conflict of Interest | 14 | |
| C. | ACO Leadership and Management | 14 | |
| D. | ACO Financial Arrangements | 14 | |
| IV. | Next Generation Participants and Preferred Providers | 17 | |
| A. | General | 17 | |
| B. | Initial Next Generation Participant List | 17 | |
| C. | Initial Preferred Provider List | 18 | |
| D. | Updating Lists During the Performance Year | 19 | |
| 1. | Additions to a List | 19 | |
| 2. | Removals from a List | 20 | |
| 3. | Updating Enrollment Information | 20 | |
| E. | Annual Updates to Participant List and Preferred Provider List | 20 | |
| 1. | Proposed Participant and Preferred Provider Lists | 20 | |
| 2. | ACO Notice to Proposed Participants | 21 | |
| 3. | ACO Notice to TINs | 21 | |
| 4. | Review, Certification, and Finalization of the Participant List and Preferred Provider List | 21 | |
| F. | Non-Duplication and Exclusivity of Participation | 22 | |
| V. | Beneficiary Alignment, Engagement, and Protections | 23 | |
| A. | Beneficiary Alignment | 23 | |
| B. | Alignment Minimum | 23 | |
| C. | Voluntary Alignment | 23 | |
| 1. | General | 23 | |
| 1 |
| 2. | Influencing or Attempting to Influence the Beneficiary | 23 | |
| 3. | Enforcement | 24 | |
| 4. | Modification or Elimination of Voluntary Alignment | 24 | |
| D. | Beneficiary Notifications | 24 | |
| E. | Descriptive ACO Materials and Activities | 24 | |
| F. | Availability of Services | 25 | |
| G. | Beneficiary Freedom of Choice | 25 | |
| H. | Prohibition on Beneficiary Inducements | 26 | |
| 1. | General Prohibition | 26 | |
| 2. | Exception | 26 | |
| I. | HIPAA Requirements | 26 | |
| VI. | Data Sharing and Reports | 27 | |
| A. | General | 27 | |
| B. | Provision of Certain Claims Data | 27 | |
| C. | De-Identified Reports | 30 | |
| 1. | Monthly Financial Reports | 30 | |
| 2. | Quarterly Benchmark Reports | 30 | |
| D. | Beneficiary Rights to Opt Out of Data Sharing | 31 | |
| E. | Beneficiary Substance Abuse Data Opt-In | 32 | |
| F. | Certification of Data and Information | 32 | |
| VII. | Care Improvement Objectives | 33 | |
| A. | General | 33 | |
| B. | Outcomes-Based Contracts with Other Purchasers | 33 | |
| VIII. | ACO Quality Performance | 34 | |
| A. | Quality Scores | 34 | |
| B. | Quality Measures | 34 | |
| C. | Quality Measure Reporting | 34 | |
| D. | Quality Performance Scoring | 35 | |
| IX. | Use of Certified EHR Technology | 35 | |
| X. | ACO Selections and Approval | 35 | |
| A. | ACO Selections | 35 | |
| 2 |
| B. | Risk Arrangement and Savings/Loss Cap Approval | 36 | |
| C. | Alternative Payment Mechanism Approval | 36 | |
| XI. | Benefit Enhancements | 36 | |
| A. | General | 36 | |
| B. | 3-Day SNF Rule Waiver Benefit Enhancement | 36 | |
| C. | Telehealth Expansion | 37 | |
| D. | Post-Discharge Home Visits | 37 | |
| E. | Requirements for Termination of Benefit Enhancements | 38 | |
| F. | Termination of Benefit Enhancements upon Termination | 38 | |
| XII. | Coordinated Care Reward | 39 | |
| A. | Reward Payment | 39 | |
| B. | ACO Obligations and Limitations Regarding the Coordinated Care Reward | 39 | |
| XIII. | ACO Benchmark | 40 | |
| A. | Prospective Benchmark | 40 | |
| B. | Trend Adjustments | 40 | |
| XIV. | Payment | 40 | |
| A. | General | 40 | |
| B. | Alternative Payment Mechanisms | 41 | |
| 1. | General | 41 | |
| 2. | Infrastructure Payments | 41 | |
| 3. | Population-Based Payments (PBP) | 41 | |
| 4. | All-Inclusive Population-Based Payments (AIPBP) | 41 | |
| C. | Settlement | 42 | |
| 1. | General | 42 | |
| 2. | Error Notice | 42 | |
| 3. | Deferred Settlement | 43 | |
| 4. | Settlement Reopening | 43 | |
| 5. | Payment of Amounts Owed | 43 | |
| 6. | Transition from the ACO Investment Model (AIM) | 44 | |
| D. | Financial Guarantee | 44 | |
| E. | Delinquent Debt | 44 | |
| 3 |
| XV. | Participation in Evaluation, Shared Learning Activities, and Site Visits | 44 | |
| A. | Evaluation Requirement | 45 | |
| 1. | General | 45 | |
| 2. | Primary Data | 45 | |
| 3. | Secondary Data | 45 | |
| B. | Shared Learning Activities | 46 | |
| C. | Site Visits | 46 | |
| D. | Rights in Data and Intellectual Property | 46 | |
| XVI. | Public Reporting and Release of Information | 47 | |
| A. | ACO Public Reporting and Transparency | 47 | |
| B. | ACO Release of Information | 47 | |
| XVII. | Compliance and Oversight | 48 | |
| A. | ACO Compliance Plan | 48 | |
| B. | CMS Monitoring and Oversight Activities | 48 | |
| C. | ACO Compliance with Monitoring and Oversight Activities | 49 | |
| D. | Compliance with Laws | 49 | |
| 1. | Agreement to Comply | 49 | |
| 2. | State Recognition | 49 | |
| 3. | Reservation of Rights | 50 | |
| 4. | Office of Inspector General of the Department of Health and Human Services (OIG) Authority | 50 | |
| 5. | Other Government Authority | 50 | |
| E. | Certification of Data and Information | 50 | |
| XVIII. | Audits and Record Retention | 51 | |
| A. | Right to Audit and Correction | 51 | |
| B. | Maintenance of Records | 51 | |
| XIX. | Remedial Action and Termination | 52 | |
| A. | Remedial Action | 52 | |
| B. | Termination of Agreement by CMS | 54 | |
| C. | Termination of Agreement by ACO | 55 | |
| D. | Financial Settlement upon Termination | 55 | |
| 4 |
| E. | Notifications to Participants, Preferred Providers, and Beneficiaries upon Termination. | 55 | |
| XX. | Limitation on Review and Dispute Resolution | 56 | |
| A. | Limitations on Review | 56 | |
| B. | Dispute Resolution | 56 | |
| 1. | Right to Reconsideration | 56 | |
| 2. | Standards for reconsideration. | 57 | |
| 3. | Reconsideration determination. | 57 | |
| XXI. | Miscellaneous | 58 | |
| A. | Agency Notifications and Submission of Reports | 58 | |
| B. | Notice of Bankruptcy | 58 | |
| C. | Severability | 59 | |
| D. | Entire Agreement; Amendment | 59 | |
| E. | Survival | 59 | |
| F. | Precedence | 60 | |
| G. | Change of ACO Name | 60 | |
| H. | Prohibition on Assignment | 60 | |
| I. | Change in Control | 60 | |
| J. | Certification | 61 | |
| K. | Execution in Counterpart | 61 | |
| 5 |
PARTICIPATION AGREEMENT
This participation agreement (“Agreement”) is between the CENTERS FOR MEDICARE & MEDICAID SERVICES (“CMS”) and ____________________________, an accountable care organization (“ACO”).
CMS is the agency within the U.S. Department of Health and Human Services (“HHS”) that is charged with administering the Medicare and Medicaid programs.
The ACO is an entity that has been approved by CMS to operate a Medicare accountable care organization (“Medicare ACO”). A Medicare ACO is an entity formed by certain health care providers that accepts financial accountability for the overall quality and cost of medical care furnished to Medicare fee-for-service beneficiaries assigned to the entity.
Typically, the health care providers participating in a Medicare ACO continue to bill Medicare under the traditional fee-for-service system for services rendered to Beneficiaries. However, the Medicare ACO may share in any Medicare savings achieved with respect to the aligned beneficiary population if the Medicare ACO satisfies minimum quality performance standards. The Medicare ACO may also share in any Medicare losses recognized with respect to the aligned beneficiary population. Medicare ACOs participating in a two-sided risk model are liable to CMS for a portion of the Medicare expenditures that exceed a benchmark.
CMS is implementing the Next Generation ACO Model (“Model”) under section 1115A of the Social Security Act (“Act”), which authorizes CMS, through its Center for Medicare and Medicaid Innovation, to test innovative payment and service delivery models that have the potential to reduce Medicare, Medicaid, or Children’s Health Insurance Program expenditures while maintaining or improving the quality of beneficiaries’ care.
The purpose of the Next Generation ACO Model is to test an alternative Medicare ACO payment model. Specifically, this model will test whether health outcomes improve and Medicare Parts A and B expenditures for Medicare fee-for-service beneficiaries decrease if Medicare ACOs (1) accept a higher level of financial risk compared to existing Medicare ACO payment models, and (2) are permitted to select certain innovative Medicare payment arrangements and to offer certain additional benefit enhancements to their assigned Medicare fee-for-service beneficiaries.
The ACO submitted an application to participate in the Next Generation ACO Model, and CMS has approved the ACO for participation in the model.
The parties therefore agree as follows:
| I. | Agreement Term and Renewal |
| A. | This Agreement will become effective when it is signed by both parties. The effective date of this Agreement (the “Effective Date”) will be the date this Agreement is signed by the last party to sign it (as indicated by the date associated with that party’s signature). This Agreement will conclude at the end of two Performance Years (the “Initial Term”) or at the end of a renewal period, unless sooner terminated by either party in accordance with Section XIX. |
| 6 |
| B. | The first Performance Year of this Agreement shall begin on January 1, 2017 (the “Start Date”) and end on December 31, 2017. The second Performance Year shall begin on January 1, 2018 and end on December 31, 2018. |
| C. | CMS may offer to renew this Agreement for a renewal period of an additional two Performance Years. In deciding whether to offer to renew this Agreement, CMS may consider the ACO’s actual spending in relation to the Performance Year Benchmark; the ACO’s quality score performance; the ACO’s history of compliance with the terms of this Agreement and Medicare program requirements; the results of a program integrity screening of the ACO, its Next Generation Participants, and its Next Generation Professionals; the ACO’s ability to repay in full any Shared Losses and Other Monies Owed; and such other criteria CMS deems relevant. If CMS offers to renew this Agreement, CMS shall make a written offer to renew this Agreement at least 60 days before the expiration of the Initial Term. The ACO shall accept or reject such offer in writing by a date and in a manner specified by CMS. |
| II. | Definitions |
“ACO Activities” means activities related to promoting accountability for the quality, cost, and overall care for a patient population of aligned Medicare fee-for-service Beneficiaries, including managing and coordinating care for Next Generation Beneficiaries; encouraging investment in infrastructure and redesigned care processes for high quality and efficient service delivery; or carrying out any other obligation or duty of the ACO under this Agreement. Examples of these activities include, but are not limited to, providing direct patient care to Next Generation Beneficiaries in a manner that reduces costs and improves quality; promoting evidence-based medicine and patient engagement; reporting on quality and cost measures under this Agreement; coordinating care for Next Generation Beneficiaries, such as through the use of telehealth, remote patient monitoring, and other enabling technologies; establishing and improving clinical and administrative systems for the ACO; meeting the quality performance standards of this Agreement; evaluating health needs of Next Generation Beneficiaries; communicating clinical knowledge and evidence-based medicine to Next Generation Beneficiaries; and developing standards for Beneficiary access and communication, including Beneficiary access to medical records.
“AIPBP” means the all-inclusive population-based payment Alternative Payment Mechanism in which CMS makes a monthly payment to the ACO reflecting an estimate, based on historical expenditures, of the percentage of total expected Medicare Part A and/or Part B FFS payments for Covered Services furnished to Next Generation Beneficiaries by Next Generation Participants and Preferred Providers who have agreed to receive AIPBP Fee Reduction.
“AIPBP Fee Reduction” means the 100% reduction in Medicare FFS payments to selected Next Generation Participants and Preferred Providers, who have agreed to receive no payment from Medicare for Covered Services furnished to Next Generation Beneficiaries to account for the Monthly AIPBP Payments made by CMS to the ACO under AIPBP.
“Alternative Payment Mechanism” means an optional payment mechanism that may be selected by the ACO for a given Performance Year, under which CMS will make interim payments to the ACO during a Performance Year. The three Alternative Payment Mechanisms available for selection are Infrastructure Payments, PBP, and AIPBP.
| 7 |
“At-Risk Beneficiary” means a Beneficiary who—
| A. | Has a high risk score on the CMS-Hierarchical Condition Category (HCC) risk adjustment model; |
| B. | Is considered high cost due to having two or more hospitalizations or emergency room visits each year; |
| C. | Is dually eligible for Medicare and Medicaid; |
| D. | Has a high utilization pattern; |
| E. | Has one or more chronic conditions; |
| F. | Has had a recent diagnosis that is expected to result in increased cost |
| G. | Is entitled to Medicaid because of disability; |
| H. | Is diagnosed with a mental health or substance abuse disorder; or |
| I. | Meets such other criteria as specified in writing by CMS. |
“Beneficiary” means an individual who is enrolled in Medicare.
“Benefit Enhancements” means the following additional benefits the ACO chooses to make available to Next Generation Beneficiaries through Next Generation Participants and Preferred Providers in order to support high-value services and allow the ACO to more effectively manage the care of Next Generation Beneficiaries: (1) 3-Day SNF Rule Waiver (as described in Section
XI.B and Appendix I; (2) Telehealth Expansion (as described in Section XI.C and Appendix J); and (3) Post-Discharge Home Visits (as described in Section XI.D and Appendix K).
“CCN” means a CMS Certification Number.
“Coordinated Care Reward” means payment from CMS to a Beneficiary to reward the Beneficiary for receiving qualifying services from Next Generation Participants and Preferred Providers in an ACO when the Beneficiary was a Next Generation Beneficiary aligned to that ACO.
“Covered Services” means the scope of health care benefits described in sections 1812 and 1832 of the Act for which payment is available under Part A or Part B of Title XVIII of the Act.
“Days” means calendar days unless otherwise specified.
“Descriptive ACO Materials and Activities” include, but are not limited to, general audience materials such as brochures, advertisements, outreach events, letters to Beneficiaries, web pages, mailings, social media, or other activities conducted by or on behalf of the ACO or its Next Generation Participants or Preferred Providers, when used to educate, notify, or contact Beneficiaries regarding the Next Generation ACO Model. The following communications are not Descriptive ACO Materials and Activities: communications that do not directly or indirectly reference the Next Generation ACO Model (for example, information about care coordination generally would not be considered Descriptive ACO Materials and Activities); materials that cover Beneficiary-specific billing and claims issues; educational information on specific medical conditions; referrals for health care items and services; and any other materials that are excepted from the definition of “marketing” under the HIPAA Privacy Rule (45 CFR Part 160 & Part 164, subparts A & E).
| 8 |
“FFS” means fee-for-service.
“Infrastructure Payments” means the Alternative Payment Mechanism under which CMS makes monthly per-Next Generation Beneficiary payments to the ACO to support ACO Activities.
“Legacy TIN” means a TIN that a Next Generation Participant or Preferred Provider previously used for billing Medicare Parts A and B services but no longer uses to bill for those services, and includes a “sunsetted” Legacy TIN (a TIN that is no longer used for billing for Medicare Parts A and B services by any Medicare-enrolled provider or supplier) or an “active” Legacy TIN (a TIN that may be in use by a Medicare-enrolled provider or supplier that is not a Next Generation Participant or Preferred Provider).
“Medically Necessary” means reasonable and necessary as determined in accordance with section 1862(a) of the Act.
“Monthly AIPBP Payment” means the monthly payment made by CMS to an ACO under AIPBP.
“Monthly PBP Payment” means the monthly payment made by CMS to an ACO under PBP.
“Next Generation Beneficiary” means a Beneficiary who is aligned to the ACO for a given Performance Year using the methodology set forth in Appendix B and has not subsequently been excluded from the aligned population of the ACO.
“Next Generation Participant” means an individual or entity that:
| A. | Is a Medicare-enrolled provider (as defined at 42 CFR § 400.202) or supplier (as defined at 42 CFR § 400.202); |
| B. | Is identified on the Participant List in accordance with Section IV; |
| C. | Bills for items and services it furnishes to Beneficiaries under a Medicare billing number assigned to a TIN in accordance with applicable Medicare regulations; |
| D. | Is not a Preferred Provider; |
| E. | Is not a Prohibited Participant; and |
| F. | Pursuant to a written agreement with the ACO, has agreed to participate in the Model, to report quality data through the ACO, and to comply with care improvement objectives and Model quality performance standards. |
“Next Generation Professional” means a Next Generation Participant who is either:
| A. | A physician (as defined in section 1861(r) of the Act); or |
| B. | One of the following non-physician practitioners: |
| 1. | Physician assistant who satisfies the qualifications set forth at 42 CFR § 410.74(a)(2)(i)-(ii); |
| 2. | Nurse practitioner who satisfies the qualifications set forth at 42 CFR § 410.75(b); |
| 3. | Clinical nurse specialist who satisfies the qualifications set forth at 42 CFR § 410.76(b); |
| 4. | Certified registered nurse anesthetist (as defined at 42 CFR § 410.69(b)); |
| 9 |
| 5. | Certified nurse midwife who satisfies the qualifications set forth at 42 CFR § 410.77(a); |
| 6. | Clinical psychologist (as defined at 42 CFR § 410.71(d)); |
| 7. | Clinical social worker (as defined at 42 CFR § 410.73(a)); or |
| 8. | Registered dietician or nutrition professional (as defined at 42 CFR § 410.134). |
“NPI” means a national provider identifier.
“Other Monies Owed” means a monetary amount owed by either party to this Agreement that represents a reconciliation of monthly payments made by CMS during a Performance Year, including payments made through Alternative Payment Mechanisms, and is neither Shared Savings nor Shared Losses. Such calculations shall be made in accordance with Appendix B and reconciliation shall be performed pursuant to Section XIV.B.
“Participant List” means the list that identifies each Next Generation Participant that is approved by CMS for participation in the Next Generation Model, specifies which Next Generation Participants, if any, have agreed to receive an AIPBP Fee Reduction or PBP Fee Reduction, and designates the Benefit Enhancements, if any, in which each Next Generation Participant participates, as updated from time to time in accordance with Sections IV.D and IV.E of this Agreement.
“PBP” means the population-based payment Alternative Payment Mechanism in which CMS makes a Monthly PBP Payment to the ACO reflecting an estimate, based on historical expenditures, of the percentage of total expected Medicare Part A and/or Part B FFS payments for Covered Services furnished to Next Generation Beneficiaries by Next Generation Participants and Preferred Providers who have agreed to receive a PBP Fee Reduction.
“PBP Fee Reduction” means a partial reduction in Medicare FFS payments to selected Next Generation Participants and Preferred Providers who have agreed to receive such reduced payments for Covered Services furnished to Next Generation Beneficiaries are reduced to account for the Monthly PBP Payments made by CMS to the ACO under PBP.
“Performance Year” means the 12-month period beginning on January 1 of each year during the term of this Agreement.
“Performance Year Benchmark” means the target expenditure amount to which actual Medicare Part A and Part B expenditures for Next Generation Beneficiaries during a Performance Year will be compared in order to calculate Shared Losses and Shared Savings as determined by CMS in accordance with Appendix B.
“Preferred Provider” means an individual or entity that:
| A. | Is a Medicare-enrolled provider (as defined at 42 CFR § 400.202) or supplier (as defined at 42 CFR § 400.202); |
| B. | Is identified on the Preferred Provider List in accordance with Section IV; |
| C. | Bills for items and services it furnishes to Beneficiaries under a Medicare billing number assigned to a TIN in accordance with applicable Medicare regulations; |
| D. | Is not a Next Generation Participant; |
| 10 |
| E. | Is not a Prohibited Participant; and |
| F. | Has agreed to participate in the Model pursuant to a written agreement with the ACO. |
“Preferred Provider List” means the list that identifies each Preferred Provider that that is approved by CMS for participation in the Next Generation Model, specifies which Preferred Providers, if any, have agreed to receive an AIPBP Fee Reduction or PBP Fee Reduction, and designates the Benefit Enhancements, if any, in which each Preferred Provider participates, as updated from time to time in accordance with Section IV of this Agreement.
“Prohibited Participant” means an individual or entity that is: (1) a Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) supplier, (2) an ambulance supplier, (3) a drug or device manufacturer, or (4) excluded or otherwise prohibited from participation in Medicare or Medicaid.
“Reduced FFS Payment” means the applicable Medicare FFS payment for Covered Services furnished by Next Generation Participants or Preferred Providers to Next Generation Beneficiaries, less the applicable AIPBP Fee Reduction or PBP Fee Reduction.
“Risk Arrangement” means the arrangement selected by the ACO that determines the portion of the savings or losses in relation to the Performance Year Benchmark that accrue to the ACO as Shared Savings or Shared Losses.
“Rural ACO” means an ACO in this Model for which at least 40 percent of the Federal Information Processing Standard (FIPS) codes in its service area are determined to be rural according to the definition used by the Health Resources and Services Administration (HRSA) Office of Rural Health Policy. Such definition includes all non-Metropolitan counties, census tracts inside Metropolitan counties with Rural-Urban Commuting Area (RUCA) codes 4-10, and census tracts with RUCA codes 2 or 3 that are at least 400 square miles in area with a population density of no more than 35 people per square mile.
“Savings/Losses Cap” means the maximum percentage of Shared Savings or Shared Losses that will be paid to or owed by the ACO, as selected by the ACO in accordance with Section X.A.2. and based upon the ACO’s Performance Year Benchmark (i.e., if the ACO elects a 5% Savings/Losses Cap, the ACO would only share in savings up to 5% of its Performance Year Benchmark, even if it achieved savings equal to 6% of that Performance Year Benchmark and elected a 100% savings risk arrangement).
“Shared Losses” means the monetary amount owed to CMS by the ACO in accordance with the applicable Risk Arrangement and Appendix B due to expenditures for Medicare Part A and B items and services furnished to Next Generation Beneficiaries in excess of the Performance Year Benchmark.
“Shared Savings” means the monetary amount owed to the ACO by CMS in accordance with the applicable Risk Arrangement and Appendix B due to expenditures for Medicare Part A and B items and services furnished to Next Generation Beneficiaries lower than the Performance Year Benchmark.
“TIN” means a federal taxpayer identification number.
“Voluntary Alignment” means the process by which Beneficiaries may voluntary align to the ACO as described in Section V.C and Appendix C.
| 11 |
“Voluntary Alignment Form” has the meaning set forth in Appendix C.
| III. | ACO Composition |
| A. | ACO Legal Entity |
| 1. | The ACO shall be a legal entity identified by a TIN formed under applicable state, federal, or tribal law, and authorized to conduct business in each state in which it operates for purposes of the following: |
| (a) | Receiving and distributing Shared Savings; |
| (b) | Repaying Shared Losses or Other Monies Owed to CMS; |
| (c) | Establishing, reporting, and ensuring Next Generation Participant compliance with health care quality criteria, including quality performance standards; and |
| (d) | Fulfilling ACO Activities identified in this Agreement. |
| 2. | If the ACO was formed by two or more Next Generation Participants, the ACO shall be a legal entity separate from the legal entity of any of its Next Generation Participants or Preferred Providers. |
| 3. | If the ACO was formed by a single Next Generation Participant, the ACO’s legal entity and governing body may be the same as that of the Next Generation Participant if the ACO satisfies the requirements of Section III.B. |
| 4. | The ACO is deemed to satisfy the requirements of Sections III.A.1 and III.A.2 if, as of the Effective Date, it was a Pioneer ACO pursuant to a Pioneer ACO Model Innovation Agreement or a Medicare Shared Savings Program (“MSSP”) ACO pursuant to a participation agreement (as defined at 42 C.F.R. § 425.20). |
| 5. | During the term of this Agreement, the ACO shall not participate in the MSSP, the independence at home medical practice pilot program under section 1866E of the Act, another model tested or expanded under section 1115A of the Act that involves shared savings, or any other Medicare initiative that involves shared savings. |
| B. | ACO Governance |
| 1. | General |
| (a) | The ACO shall maintain an identifiable governing body with sole and exclusive authority to execute the functions of the ACO and make final decisions on behalf of the ACO. The ACO shall have a governing body that satisfies the following criteria: |
| i. | The governing body has responsibility for oversight and strategic direction of the ACO and is responsible for holding ACO management accountable for the ACO's activities; |
| ii. | The governing body is separate and unique to the ACO, except as permitted under section III.A.3; |
| 12 |
| iii. | The governing body has a transparent governing process; |
| iv. | When acting as a member of the governing body of the ACO, each governing body member has a fiduciary duty to the ACO, including the duty of loyalty, and shall act consistent with that fiduciary duty; and |
| v. | The governing body shall receive regular reports from the designated compliance official of the ACO that satisfies the requirements of XVII.A.1. |
| (b) | The ACO shall provide each member of the governing body with a copy of this Agreement. |
| 2. | Composition and Control of the Governing Body |
| (a) | The ACO governing body shall include at least one Beneficiary served by the ACO who: |
| i. | Does not have a conflict of interest with the ACO; |
| ii. | Has no immediate family member with a conflict of interest with the ACO; |
| iii. | Is not a Next Generation Participant or Preferred Provider; and |
| iv. | Does not have a direct or indirect financial relationship with the ACO, a Next Generation Participant, or a Preferred Provider, except that such person may be reasonably compensated by the ACO for his or her duties as a member of the governing body of the ACO. |
| (b) | The ACO governing body shall include at least one person with training or professional experience in advocating for the rights of consumers (“Consumer Advocate”), who may be the same person as the Beneficiary and who: |
| i. | Does not have a conflict of interest with the ACO; |
| ii. | Has no immediate family member with a conflict of interest with the ACO; |
| iii. | Is not a Next Generation Participant or Preferred Provider; and |
| iv. | Does not have a direct or indirect financial relationship with the ACO, a Next Generation Participant, or a Preferred Provider, except that such person may be reasonably compensated by the ACO for his or her duties as a member of the governing body of the ACO. |
| (c) | The ACO Governing body shall not include a Prohibited Participant, or an owner, employee or agent of a Prohibited Participant. |
| (d) | If Beneficiary and/or consumer advocate representation on the ACO governing body is prohibited by state law, the ACO shall notify CMS and request CMS approval of an alternative mechanism to ensure that its policies and procedures reflect consumer and patient perspectives. CMS shall use reasonable efforts to approve or deny the request within 30 days. |
| 13 |
| (e) | The governing body members may serve in similar or complementary roles or positions for Next Generation Participants or Preferred Providers. |
| (f) | At least 75 percent control of the ACO's governing body shall be held by Next Generation Participants or their designated representatives. The Beneficiary and consumer advocate required under this Section shall not be included in either the numerator or the denominator when calculating the percent control. |
| 3. | Conflict of Interest |
The ACO shall have a conflict of interest policy that applies to members of the governing body and satisfies the following criteria:
| (a) | Requires each member of the governing body to disclose relevant financial interests; |
| (b) | Provides a procedure to determine whether a conflict of interest exists and set forth a process to address any conflicts that arise; and |
| (c) | Addresses remedial actions for members of the governing body that fail to comply with the policy. |
| C. | ACO Leadership and Management |
| 1. | The ACO’s operations shall be managed by an executive, officer, manager, general partner, or similar party whose appointment and removal are under the control of the ACO’s governing body and whose leadership team has demonstrated the ability to influence or direct clinical practice to improve the efficiency of processes and outcomes. |
| 2. | Clinical management and oversight shall be managed by a senior-level medical director who is: |
| (a) | A Next Generation Participant; |
| (b) | Physically present on a regular basis at any clinic, office, or other location participating in the ACO; and |
| (c) | A board-certified physician and licensed in a state in which the ACO operates. |
| D. | ACO Financial Arrangements |
| 1. | The ACO shall not condition a Next Generation Participant’s or Preferred Provider’s participation in the Model, directly or indirectly, on referrals of items or services provided to Beneficiaries who are not aligned to the ACO. |
| 2. | The ACO shall not require that Next Generation Beneficiaries be referred only to Next Generation Participants or Preferred Providers or to any other provider or supplier. This prohibition shall not apply to referrals made by employees or contractors who are operating within the scope of their employment or contractual arrangement with the employer or contracting entity, provided that the employees and contractors remain free to make referrals without restriction or limitation if a Next Generation Beneficiary expresses a preference for a different provider or supplier, or the referral is not in the Next Generation Beneficiary's best medical interests in the judgment of the referring party. |
| 14 |
| 3. | The ACO shall not condition the eligibility of an individual or entity to be a Next Generation Participant or Preferred Provider on the individual’s or entity’s offer or payment of cash or other remuneration to the ACO or any other individual or entity. |
| 4. | The ACO, its Next Generation Participants, and/or Preferred Providers shall not take any action to limit the ability of a Next Generation Participant or Preferred Provider to make decisions in the best interests of the Beneficiary, including the selection of devices, supplies and treatments used in the care of the Beneficiary. |
| 5. | The ACO shall notify CMS within 15 days after becoming aware that any Next Generation Participant or Preferred Provider is under investigation or has been sanctioned by the Government or any licensing authority (including, without limitation, the imposition of program exclusion, debarment, civil monetary penalties, corrective action plans, and revocation of Medicare billing privileges). If a Next Generation Participant or Preferred Provider is under investigation or has been sanctioned but not excluded from Medicare program participation, CMS may take any of the actions set forth in Section XIX. |
| 6. | By the date specified in Section III.D.7, below, the ACO shall have a written agreement with each of the individuals and entities that are approved by CMS to be Next Generation Participants or Preferred Providers that complies with the following criteria: |
| (a) | The only parties to the agreement are the ACO and the Next Generation Participant or Preferred Provider. |
| (b) | The agreement requires the Next Generation Participant or Preferred Provider to agree to participate in the Model, to engage in ACO Activities, to comply with the applicable terms of the Model as set forth in this Agreement, and to comply with all applicable laws and regulations (including, but not limited to, those specified at Section XVII.D). The ACO shall provide each Next Generation Participant and Preferred Provider with a copy of this Agreement. |
| (c) | The agreement expressly sets forth the Next Generation Participant’s or Preferred Provider’s obligation to comply with the applicable terms of this Agreement, including provisions regarding the following: participant exclusivity, quality measure reporting, and continuous care improvement objectives for Next Generation Participants; Voluntary Alignment; Beneficiary freedom of choice; Benefit Enhancements; the Coordinated Care Reward; participation in evaluation, shared learning, monitoring, and oversight activities; the ACO compliance plan; and audit and record retention requirements. |
| (d) | The agreement requires the Next Generation Participant or Preferred Provider to update its Medicare enrollment information (including the addition and deletion of Next Generation Professionals that have reassigned to the Next Generation Participant or Preferred Provider their right to Medicare payment) on a timely basis in accordance with Medicare program requirements. |
| 15 |
| (e) | The agreement requires the Next Generation Participant or Preferred Provider to notify the ACO of any changes to its Medicare enrollment information within 30 days after the change. |
| (f) | The agreement requires the Next Generation Participant or Preferred Provider to notify the ACO within seven days of becoming aware that it is under investigation or has been sanctioned by the Government or any licensing authority (including, without limitation, the imposition of program exclusion, debarment, civil monetary penalties, corrective action plans, and revocation of Medicare billing privileges). |
| (g) | The agreement permits the ACO to take remedial action against the Next Generation Participant or Preferred Provider (including the imposition of a corrective action plan, denial of incentive payments such as Shared Savings distributions, and termination of the ACO’s agreement with the Next Generation Participant or Preferred Provider) to address noncompliance with the terms of the Model or program integrity issues identified by CMS. |
| (h) | The agreement is for a term of at least one year, but permits early termination if CMS requires the ACO to remove the Next Generation Participant or Preferred Provider pursuant to Section XIX.A.1. |
| (i) | The agreement requires the Next Generation Participant to complete a close- out process upon termination or expiration of the agreement that requires the Next Generation Participant to furnish all quality measure reporting data. |
| 7. | The ACO shall have fully executed written agreements in place that meet the requirements set forth in Section III.D.6 by the following dates: |
| (a) | By the Start Date in the case of agreements with individuals and entities that are approved by CMS before the Start Date to be Next Generation Participants and Preferred Providers; |
| (b) | By the date the ACO certifies its Participant List and Preferred Provider Lists in accordance with Section IV.E in the case of agreements with individuals and entities approved by CMS to be Next Generation Participants and Preferred Providers effective on the first day of the second or any subsequent Performance Year. |
| (c) | For agreements with individuals or entities approved by CMS to be Next Generation Participants or Preferred Providers effective on a day other than the first day of a Performance Year, by the date the ACO requests the addition of the individual or entity to the Participant List or Preferred Provider List. |
| 8. | The ACO shall not distribute Shared Savings to any Next Generation Participant or Preferred Provider that has been terminated pursuant to Section XIX.A.1. |
| 16 |
| 9. | CMS provides no opinion on the legality of any contractual or financial arrangement that the ACO, a Next Generation Participant, or a Preferred Provider has proposed, implemented, or documented. The receipt by CMS of any such documents in the course of the application process or otherwise shall not be construed as a waiver or modification of any applicable laws, rules or regulations, and will not preclude CMS, HHS or its Office of Inspector General, a law enforcement agency, or any other federal or state agency from enforcing any and all applicable laws, rules and regulations. |
| IV. | Next Generation Participants and Preferred Providers |
| A. | General |
| 1. | Next Generation Participants and Preferred Providers will be included on the Participant List or Preferred Provider List only upon the prior written approval of CMS. |
| 2. | CMS shall maintain the Participant List and Preferred Provider List in a manner that permits the ACO to review the list. |
| 3. | The ACO shall maintain current and historical Participant Lists and Preferred Provider Lists in accordance with Section XVIII. |
| 4. | CMS may periodically monitor the program integrity history of an ACO’s Next Generation Participants or Preferred Providers. CMS may remove an individual or entity from the Participant List or Preferred Provider List, or subject the ACO to additional monitoring on the basis of the results of a periodic program integrity screening or information obtained regarding an individual’s or entity’s history of program integrity issues. CMS shall notify the ACO if it chooses to remove an individual or entity from the Participant List or Preferred Provider List, and such notice shall specify the effective date of removal. |
| B. | Initial Next Generation Participant List |
| 1. | The parties acknowledge that the ACO submitted to CMS a proposed list of Next Generation Participants, identified by name, NPI, TIN, Legacy TIN (if applicable), and CCN (if applicable). |
| 2. | CMS states that it has reviewed the proposed list of Next Generation Participants and conducted a program integrity screening on the proposed Next Generation Participants. |
| 3. | CMS states that it has submitted to the ACO a list of individuals and entities that it approved to be Next Generation Participants. The ACO states that it reviewed the list and made any necessary corrections to it, including the removal of any individuals or entities that have not agreed to participate in the Model as of the Start Date pursuant to a written agreement. No additions to the list are permitted. |
| 17 |
| 4. | The ACO states that it has submitted to CMS an initial Participant List that the ACO has certified is a true, accurate and complete list identifying all of the ACO’s Next Generation Participants approved by CMS to participate in the Model as of the Start Date and with whom the ACO will have a fully executed written agreement meeting the requirements in Section III.D.6. The ACO further states that, by a date set by CMS, this initial Participant List identified which individuals and entities, if any, had agreed to receive a PBP Fee Reduction or AIPBP Fee Reduction and specified the Benefit Enhancements, if any, in which each individual or entity had agreed to participate. |
| 5. | The ACO states that at least 30 days after the Start Date it will furnish a written notice to the executive of each entity through whose TIN a Next Generation Participant bills Medicare. The notice must – |
| (a) | Include a list identifying by name and NPI each Next Generation Participant who is identified on the initial Participant List as billing through the entity’s TIN; and |
| (b) | Inform the executive that participation in the Model may preclude a Next Generation Participant from participating in the MSSP, another Medicare ACO or other payment model tested or expanded under section 1115A of the Act, or any other Medicare initiative that involves shared savings. |
| 6. | The ACO shall update the initial Participant List in accordance with Sections IV.D and IV.E. |
| C. | Initial Preferred Provider List |
| 1. | The parties acknowledge that the ACO submitted to CMS a proposed list of Preferred Providers identified by name, NPI, TIN, Legacy TIN (if applicable), and CCN (if applicable). The proposed list also identified which individuals and entities, if any, had agreed to receive a PBP Fee Reduction, and specified the Benefit Enhancements, if any, in which each individual or entity had agreed to participate. |
| 2. | CMS states that it will review the proposed list of Preferred Providers and conduct a program integrity screening on the proposed Preferred Providers. |
| 3. | Before the Start Date, CMS shall submit to the ACO a list of individuals and entities that it has approved to be Preferred Providers. The ACO shall review the list and made any necessary corrections to it, including the removal of any individuals or entities that have not agreed to participate in the Model. No additions to this list are permitted at this time. |
| 4. | Before the Start Date or at such other time as may be specified by CMS, the ACO shall submit to CMS an initial Preferred Provider List that the ACO has certified is a true, accurate and complete list identifying the following: (i) all of the ACO’s Preferred Providers approved by CMS to participate in the Model as of the Start Date, and with whom the ACO will have, by the date specified in Section III.D.7.a, a fully executed written agreement meeting the requirements in Section III.D.6; (ii) each Preferred Provider that has agreed to receive a PBP Fee Reduction, or AIPBP Fee Reduction, if applicable, and (iii) the specific Benefit Enhancements, if any, in which each Preferred Provider has agreed to participate. |
| 18 |
| 5. | The ACO shall update the initial Preferred Provider List in accordance with Sections IV.D and IV.E. |
| D. | Updating Lists During the Performance Year |
| 1. | Additions to a List |
| (a) | Participant List Additions. The ACO shall not add a Next Generation Participant without prior written approval from CMS. If the ACO wishes to add an individual or entity to the Participant List effective on a date other than the first day of a Performance Year (“during a Performance Year”), it shall submit a request to CMS in a form and manner specified by CMS. CMS may accept requests for additions only under the following circumstances: |
| i. | The request for addition is submitted to CMS between January 1 of the Performance Year for addition and July 31 of the Performance Year for addition; |
| ii. | In the case of a request to add an individual to a Participant List, the ACO certifies that the individual (1) currently bills for items and services he or she furnishes to Beneficiaries under a Medicare billing number assigned to the TIN of an entity that is a Next Generation Participant, and (2) did not bill for such services under the TIN of the same Next Generation Participant at the time the ACO submitted its most recent Proposed Participant List pursuant to Section IV.E.1; |
| iii. | The ACO certifies that it has a fully executed written agreement with the individual or entity it wishes to add to the Participant List and that the agreement meets the requirements of Section III.D.6; and |
| iv. | The ACO certifies that is has given notice to each Next Generation Participant that is a physician or non-physician practitioner and the TIN through which such individual bills Medicare that the individual has been added to the ACO’s Participant List. |
CMS may reject the request on the basis that the individual or entity fails to satisfy the definition of “Next Generation Participant,” or on the basis of information obtained from a program integrity screening. If CMS approves the request, the individual or entity will be added to the Participant List effective on the date the addition is approved by CMS.
| (b) | Preferred Provider List Additions. The ACO shall not add an individual or entity to the Preferred Provider List during a Performance Year without prior written approval from CMS. If the ACO wishes to add an individual or entity to the Preferred Provider List during a Performance Year, it shall submit a request to CMS in the form and manner and by a deadline specified by CMS, under the following requirements: |
| i. | The ACO certifies that is has a fully executed written agreement with the individual or entity it wishes to add to the Preferred Provider List and that the agreement meets the requirements of Section III.D.6; and |
| 19 |
| ii. | The ACO certifies that it has furnished a written notice to the executive of each entity identified in the request for addition through whose TIN a Preferred Provider bills Medicare. The notice must identify by name and NPI each individual who is identified on the request for addition as billing through the entity’s TIN. |
CMS may reject the request on the basis that the individual or entity fails to satisfy the definition of “Preferred Provider,” or on the basis of information obtained from a program integrity screening. If CMS approves the request, the individual or entity will be added to the Preferred Provider List effective on the date the addition is approved by CMS.
| 2. | Removals from a List |
In a form and manner specified by CMS, the ACO shall notify CMS no later than 30 days after an individual or entity has ceased to be a Next Generation Participant or Preferred Provider and shall include in the notice the date on which the individual or entity ceased to be a Next Generation Participant or Preferred Provider. The removal of the individual or entity from the Participant List or Preferred Provider List will be effective on the date the individual or entity ceased to be a Participant or Preferred Provider. An individual or entity ceases to be a Next Generation Participant or Preferred Provider when it is no longer a Medicare-enrolled provider or supplier, when its agreement with the ACO to participate in the Model terminates, or when it ceases to bill for items and services to Beneficiaries under a Medicare billing number assigned to a TIN in accordance with applicable Medicare regulations.
| 3. | Updating Enrollment Information |
The ACO shall ensure that all changes to enrollment information for Next Generation Participants and Preferred Providers, including changes to reassignment of the right to receive Medicare payment, are reported to CMS consistent with 42 C.F.R. § 424.516.
| E. | Annual Updates to Participant List and Preferred Provider List |
| 1. | Proposed Participant and Preferred Provider Lists |
Prior to its second and subsequent Performance Years, the ACO shall submit to CMS by a date and in a manner specified by CMS proposed lists identifying each individual or entity that the ACO expects to participate in the Model as a Next Generation Participant or Preferred Provider effective at the start of the next Performance Year (“Proposed Participant List” and “Proposed Preferred Provider List,” respectively). CMS shall specify a submission deadline for the Proposed Participant List that is no later than 165 days before the start of the next Performance Year. CMS shall specify a submission deadline for the Proposed Preferred Provider List that is not later than 45 days before the start of the next Performance Year. The Proposed Participant List must identify each individual or entity by name, NPI, TIN, Legacy TIN (if applicable), and CCN (if applicable).
| 20 |
The Proposed Preferred Provider List must identify each individual or entity by name, NPI, TIN, Legacy TIN (if applicable), and CCN (if applicable), and any PBP Fee Reduction, AIPBP Fee Reduction (if applicable) and participation in any benefit enhancements (if applicable). The ACO shall certify that the Proposed Preferred Provider list is a true, accurate, and complete list of individuals and entities that have agreed to be Preferred Providers, subject to CMS approval, effective January 1 of the relevant Performance Year.
| 2. | ACO Notice to Proposed Participants |
At least 14 days prior to submitting its Proposed Participant List to CMS, the ACO shall furnish written notification to each individual or entity it wishes to include on the Proposed Participant List. Such notice shall –
| (a) | State that the individual or entity and any relevant TINs through which it bills Medicare will be identified on the Proposed Participant List; and |
| (b) | State that participation in the Model may preclude the individual or entity from participating in the MSSP, another Medicare ACO or other payment model tested or expanded under section 1115A of the Act, or any other Medicare initiative that involves shared savings. |
| 3. | ACO Notice to TINs |
At least 30 days prior to submitting its Proposed Participant List and Proposed Preferred Provider List to CMS, the ACO shall furnish written notification to the executive of any TIN through which an individual on the Proposed Participant List or Proposed Preferred Provider List bills Medicare. Such notification must:
| (a) | Identify by name and NPI any individual associated with the TIN that will be identified on the ACO’s Proposed Participant List or Proposed Preferred Provider List; and |
| (b) | Inform the entity that a Next Generation Participant’s participation in the ACO may preclude the entire TIN from receiving payment adjustments through the value-based payment modifier under section 1848(p) of the Act and from participating in the MSSP. |
| 4. | Review, Certification, and Finalization of the Participant List and Preferred Provider List |
| (a) | With respect to each individual and entity identified on the Proposed Participant List and Proposed Preferred Provider List, CMS shall conduct a program integrity screening, including a review of the individual’s or entity’s history of Medicare program exclusions, current or prior law enforcement investigations, or other sanctions and affiliations with individuals or entities that have a history of program integrity issues. |
| (b) | CMS may reject any individual or entity on a Proposed Participant List or a Proposed Preferred Provider List on the basis of the results of a program integrity screening, history of program integrity issues, or if it determines that the individual or entity does not satisfy the definition of Next Generation Participant or Preferred Provider. |
| 21 |
| (c) | No later than 115 days before the start of the next Performance Year, CMS shall send the ACO a preliminary list of individuals and entities that CMS has tentatively approved to be Next Generation Participants effective at the start of the next Performance Year. |
| (d) | No later than 90 days before the start of the next Performance Year, the ACO shall, after a review of the list of tentatively approved Next Generation Participants, submit a revised Participant List with any necessary corrections, including the removal of any individuals or entities that have not agreed to participate in the Model pursuant to a written agreement with the ACO or otherwise ineligible to participate. No additions to the list are permitted at this time. The ACO shall certify that the submitted list is a true, accurate, and complete list of the individuals and entities that have agreed to be Next Generation Participants effective January 1 of the relevant Performance Year. |
| (e) | No later than 60 days before the start of the next Performance Year, CMS shall send the ACO a list of individuals and entities that CMS has approved to be Next Generation Participants effective at the start of the next Performance Year. The ACO shall not request the addition of any individual or entity to this list until after the start of the next Performance Year. |
| (f) | No later than 45 days before the start of the next Performance Year, the ACO shall submit to CMS completed AIPBP Fee Reduction, PBP Fee Reduction, and Benefit Enhancement information, as applicable, for each individual and entity identified on the Participant List it received from CMS. |
| (g) | No later than 15 days before the start of the next Performance Year, CMS shall send the ACO a final Participant List identifying all individuals and entities that CMS has approved to be Next Generation Participants effective at the start of the next Performance Year (now including PBP Fee Reduction or AIPBP Fee Reduction and Benefit Enhancement information, as applicable) and a final Preferred Provider List identifying all individuals and entities that it has approved to be Preferred Providers (including PBP Fee Reduction or AIPBP Fee Reduction and Benefit Enhancement information, as applicable) effective at the start of the next Performance Year. The ACO shall update such lists in accordance with this Agreement. |
| F. | Non-Duplication and Exclusivity of Participation |
| 1. | The ACO and its Next Generation Participants may not participate in any other Medicare shared savings initiatives, as described in Appendix A. |
| 2. | CMS waives the non-duplication requirements under section 1899(b)(4)(A) of the Act and in the implementing regulations at 42 C.F.R. § 425.114(a) regarding participation in a model tested under section 1115A of the Act that involves shared savings as they apply to Preferred Providers, subject to the conditions and requirements set forth in Appendix A. |
| 22 |
| 3. | The ACO and its Next Generation Participants and Preferred Providers are bound by the participation overlap provisions set forth in Appendix A. |
| V. | Beneficiary Alignment, Engagement, and Protections |
| A. | Beneficiary Alignment |
| 1. | CMS shall, according to the methodology set forth in Appendix B, use an analysis of evaluation and management services furnished by Next Generation Professionals to Beneficiaries to align Beneficiaries to the ACO for the purposes of the Next Generation ACO Model. |
| 2. | The addition or removal of a Next Generation Participant or Preferred Provider from the Next Generation Participant List or Preferred Provider List, pursuant to Section IV.D, will not affect the alignment of Next Generation Beneficiaries to the ACO for the Performance Year during which the removal becomes effective. |
| B. | Alignment Minimum |
| 1. | The ACO shall maintain an aligned population of at least 10,000 Next Generation Beneficiaries during each Performance Year. |
| 2. | A Rural ACO shall maintain an aligned population of at least 7,500 Next Generation Beneficiaries during each Performance Year. |
| 3. | If at any time during a Performance Year, the ACO’s aligned population falls below the minimum, CMS shall notify the ACO, request a corrective action plan (CAP) pursuant to Section XIX, and require the ACO to satisfy the applicable minimum aligned population requirement by a date specified by CMS. If the ACO’s aligned population remains below the applicable minimum required under this section by the specified date, CMS may take further remedial action and/or terminate this Agreement pursuant to Section XIX. |
| C. | Voluntary Alignment |
| 1. | General |
If the ACO elects to participate in Voluntary Alignment for a Performance Year according to Section X.A, CMS shall conduct Voluntary Alignment in accordance with Appendix C, subject to the provisions in this Section V.C.
| 2. | Influencing or Attempting to Influence the Beneficiary |
| (a) | The ACO, Next Generation Participants, Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities are prohibited from providing gifts or other remuneration to Beneficiaries as inducements for influencing a Beneficiary’s decision to complete or not complete a Voluntary Alignment Form. |
| 23 |
| (b) | The ACO, Next Generation Participants, Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities shall not, directly or indirectly, commit any act or omission, nor adopt any policy, that coerces or otherwise influences a Beneficiary’s decision to complete or not complete a Voluntary Alignment Form, including but not limited to the following: |
| i. | Offering of anything of value to the Beneficiary; |
| ii. | Including the Voluntary Alignment Form and instructions with any other materials or forms, including but not limited to materials requiring the signature of the Beneficiary; and |
| iii. | Withholding or threatening to withhold medical services or limiting or threatening to limit access to care. |
| (c) | For purposes of Section V.H.2, any items or services provided in violation of this Section V.C.2 will not be considered to have a reasonable connection to the medical care of the Beneficiary. |
| 3. | Enforcement |
In addition to the actions available under Section XIX, failure to comply with the provisions of this Section may result in retroactive reversal of any alignment of Next Generation Beneficiaries to the ACO that occurred solely pursuant to this section.
| 4. | Modification or Elimination of Voluntary Alignment |
Notwithstanding Section XXI.D, CMS may amend this Agreement without ACO consent to revise or remove the provisions of Appendix C.
| D. | Beneficiary Notifications |
| 1. | In a form and manner and by a date specified by CMS, the ACO shall provide Next Generation Beneficiaries notice in writing that they have been aligned to the ACO for the Performance Year. |
| 2. | CMS shall provide the ACO with a template letter indicating letter content that the ACO shall not change and places in which the ACO may insert its own original content. |
| 3. | Pursuant to Section V.E, the ACO shall obtain CMS approval of the final notification letter content, which includes the ACO’s own original content, prior to sending letters to Next Generation Beneficiaries. |
| E. | Descriptive ACO Materials and Activities |
| 1. | The ACO shall not use, and shall prohibit its Next Generation Participants and Preferred Providers from using Descriptive ACO Materials or Activities until reviewed and approved in their entirety by CMS. |
| 2. | Descriptive ACO Materials or Activities are deemed approved 10 business days following their submission to CMS if: |
| 24 |
| (a) | The ACO certifies in writing its compliance with all the marketing requirements under this section; and |
| (b) | CMS does not disapprove the Descriptive ACO Materials or Activities. |
| 3. | CMS may issue written notice of disapproval of Descriptive ACO Materials or Activities at any time, including after the expiration of the 10 day review period. |
| 4. | The ACO, Next Generation Participants, Preferred Providers, or any other individuals or entities performing functions or services related to ACO activities, as applicable, must immediately discontinue use of any Descriptive ACO Materials or Activities disapproved by CMS. |
| 5. | Any material changes to CMS-approved Descriptive ACO Materials and Activities must be reviewed and approved by CMS before use. |
| 6. | The ACO shall retain copies of all written and electronic Descriptive ACO Materials and Activities and appropriate records for all other Descriptive ACO Materials and Activities provided to Next Generation Beneficiaries in a manner consistent with Section XVIII. |
| F. | Availability of Services |
| 1. | The ACO shall require its Next Generation Participants and Preferred Providers to make Medically Necessary Covered Services available to Next Generation Beneficiaries in accordance with applicable laws, regulations and guidance. Next Generation Beneficiaries and their assignees retain their right to appeal claims determinations in accordance with 42 CFR § 405, Subpart I. |
| 2. | The ACO and its Next Generation Participants and Preferred Providers shall not take any action to avoid treating At-Risk Beneficiaries or to target certain Beneficiaries for services with the purpose of trying to ensure alignment in a future period. |
| G. | Beneficiary Freedom of Choice |
| 1. | Consistent with section 1802(a) of the Act, neither the ACO nor any Next Generation Participant, Preferred Provider, or other individuals or entities performing functions or services related to ACO Activities shall commit any act or omission, nor adopt any policy, that inhibits Next Generation Beneficiaries from exercising their freedom to obtain health services from providers and suppliers who are not Next Generation Participants or Preferred Providers. This prohibition shall not apply to referrals made by employees or contractors who are operating within the scope of their employment or contractual arrangement with the employer or contracting entity, provided that the employees and contractors remain free to make referrals without restriction or limitation if a Next Generation Beneficiary expresses a preference for a different provider or supplier, or the referral is not in the Next Generation Beneficiary's best medical interests in the judgment of the referring party. |
| 25 |
| 2. | Notwithstanding the foregoing, the ACO may communicate to Next Generation Beneficiaries the benefits of receiving care with the ACO. All such communications shall be deemed Descriptive ACO Materials and Activities. CMS may provide the ACO with scripts, talking points or other materials explaining these benefits. |
| H. | Prohibition on Beneficiary Inducements |
| 1. | General Prohibition |
Except as set forth in Section V.H.2, the ACO, Next Generation Participants, Preferred Providers, and other individuals or entities performing functions and services related to ACO Activities are prohibited from providing gifts or other remuneration to Beneficiaries to induce them to receive items or services from the ACO, Next Generation Participants, or Preferred Providers, or to induce them to continue to receive items or services from the ACO, Next Generation Participants or Preferred Providers.
| 2. | Exception |
| (a) | Consistent with the provisions of Section V.H.1, and subject to compliance with all other applicable laws and regulations, Next Generation Participants, Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities may provide in-kind items or services to Beneficiaries if the following conditions are satisfied: |
| i. | There is a reasonable connection between the items and services and the medical care of the Beneficiary; and |
| ii. | The items and services are preventive care items and services or advance a clinical goal for the Beneficiary, including adherence to a treatment regime, adherence to a drug regime, adherence to a follow-up care plan, or management of a chronic disease or condition. |
| (b) | For each in-kind item or service provided by a Next Generation Participant or Preferred Provider under V.H.2.a, above, the ACO shall maintain records of the following: |
| i. | The nature of the in-kind item or service; |
| ii. | The identity of each Beneficiary that received the in-kind item or service; |
| iii. | The identity of the individual or entity that furnished the in-kind item or service; and |
| iv. | The date the in-kind item or service was furnished. |
| I. | HIPAA Requirements |
| 1. | The ACO acknowledges that it is a covered entity or a business associate, as those terms are defined in 45 CFR § 160.103, of Next Generation Participants who are covered entities. |
| 26 |
| 2. | The ACO shall have all appropriate administrative, technical, and physical safeguards in place before the start of the first Performance Year to protect the privacy and security of protected health information in accordance with 45 CFR § 164.530(c). |
| 3. | The ACO shall maintain the privacy and security of all Model-related information that identifies individual Beneficiaries in accordance with the Health Insurance Portability and Accountability (HIPAA) Privacy and Security Rules and all relevant HIPAA Privacy and Security guidance applicable to the use and disclosure of protected health information by covered entities, as well as applicable state laws and regulations. |
| VI. | Data Sharing and Reports |
| A. | General |
| 1. | Subject to the limitations discussed in this Agreement, and in accordance with applicable law, CMS will offer the ACO an opportunity to request certain data and reports, which are described in Sections VI.B, V.C, and Appendix D in this Agreement. |
| 2. | The data and reports provided to the ACO under the preceding paragraph will omit individually identifiable data for Next Generation Beneficiaries who have opted out of data sharing with the ACO, as described in Section VI.D. of this Agreement. The data and reports provided to the ACO will also omit substance abuse data for any Next Generation Beneficiaries who have not opted into substance abuse data sharing, as described in Section VI.E. of this Agreement. |
| B. | Provision of Certain Claims Data |
| 1. | CMS believes that the care coordination and quality improvement work of the ACO (that is acting on its own behalf as a HIPAA covered entity (CE) or who is a business associate (BA) acting on behalf of its Next Generation Participants or Preferred Providers that are HIPAA covered entities) would benefit from the receipt of certain beneficiary-identifiable claims data on Next Generation Beneficiaries. CMS will therefore offer to the ACO an opportunity to request specific beneficiary-identifiable claims data by completing the HIPAA-Covered Disclosure Request Attestation and Data Specification Worksheet (Appendix D). All requests for beneficiary-identifiable claims data will be granted or denied at CMS’ sole discretion based on CMS’ available resources, the limitations in this Agreement, and applicable law. |
| 2. | In offering this beneficiary-identifiable claims data, CMS does not represent that the ACO or any Next Generation Participant or Preferred Provider has met all applicable HIPAA requirements for requesting data under 45 CFR 164.506(c)(4). The ACO and its Next Generation Participants and Preferred Providers should consult with their own counsel to make those determinations prior to requesting this data from CMS. |
| 27 |
| 3. | The beneficiary-identifiable claims data available is the data described in Appendix D. |
| 4. | The parties mutually agree that, except for data covered by VI.B.13 below, CMS retains all ownership rights to the data files referred to in Appendix D, and the ACO does not obtain any right, title, or interest in any of the data furnished by CMS. |
| 5. | The ACO represents, and in furnishing the data files specified in Appendix D CMS relies upon such representation, that such data files will be used solely for the purposes described in this Agreement. The ACO agrees not to disclose, use or reuse the data except as specified in this Agreement or except as CMS shall authorize in writing or as otherwise required by law. The ACO further agrees not to sell, rent, lease, loan, or otherwise grant access to the data covered by this Agreement. |
| 6. | The ACO intends to use the requested information as a tool to deliver seamless, coordinated care for patients with Original Medicare to promote better care, better health, and lower growth in expenditures. Information derived from the CMS files specified in Appendix D may be shared and used within the legal confines of the ACO and its Next Generation Participants and Preferred Providers in a manner consistent with paragraph 7 below to enable the ACO to improve care integration and be a patient-centered organization. |
| 7. | The ACO may reuse original or derivative data without prior written authorization from CMS for clinical treatment, care management and coordination, quality improvement activities, and provider incentive design and implementation, but shall not disseminate individually identifiable original or derived information from the files specified in Appendix D to anyone who is not a HIPAA CE Next Generation Participant or Preferred Provider in a treatment relationship with the subject Next Generation Beneficiary(ies); a HIPAA BA of such a CE Next Generation Participant or Preferred Provider; the ACO’s BA, where that ACO is itself a HIPAA CE; the ACO’s sub-BA, which is hired by the ACO to carry out work on behalf of the CE Next Generation Participants; or a non-participant HIPAA CE in a treatment relationship with the subject Next Generation Beneficiary(ies). When using or disclosing protected health information (PHI) or personally identifiable information (PII), obtained from files specified in Appendix D, the ACO must make “reasonable efforts to limit” the information to the “minimum necessary” to accomplish the intended purpose of the use, disclosure or request. The ACO shall further limit its disclosure of such information to the types of disclosures that CMS itself would be permitted make under the “routine uses” in the applicable systems of records listed in Appendix D. |
Subject to the limits specified above and elsewhere in this Agreement and applicable law, the ACO may link individually identifiable information specified in Appendix D (including directly or indirectly identifiable data) or derivative data to other sources of individually-identifiable health information, such as other medical records available to the ACO and its Next Generation Participants or Preferred Providers. The ACO may disseminate such data that has been linked to other sources of individual identifiable health information provided such data has been de-identified in accordance with HIPAA requirements in 45 CFR 164.514(b).
| 28 |
| 8. | The ACO agrees to establish appropriate administrative, technical, and physical safeguards to protect the confidentiality of the data and to prevent unauthorized use or access to it. The safeguards shall provide a level and scope of security that is not less than the level and scope of security requirements established for federal agencies by the Office of Management and Budget (OMB) in OMB Circular No. A-130, Appendix I—Responsibilities for Protecting and Managing Federal Information Resources (https://www.whitehouse.gov/omb/circulars_default) as well as Federal Information Processing Standard 200 entitled “Minimum Security Requirements for Federal Information and Information Systems” (http://csrc.nist.gov/publications/fips/fips200/FIPS-200-final-march.pdf); and, NIST Special Publication 800-53 “Recommended Security Controls for Federal Information Systems” (http://nvlpubs.nist.gov/nistpubs/SpecialPublications/NIST.SP.800-53r4.pdf). The ACO acknowledges that the use of unsecured telecommunications, including the Internet, to transmit directly or indirectly identifiable information from the files specified in Appendix D or any such derivative data files is strictly prohibited. Further, the ACO agrees that the data specified in Appendix D must not be physically moved, transmitted or disclosed in any way from or by the site of the custodian indicated in Appendix D other than as provided in this Agreement without written approval from CMS, unless such movement, transmission or disclosure is required by a law. |
| 9. | The ACO agrees to grant access to the data and/or the facility(ies) in which the data is maintained to the authorized representatives of CMS or DHHS Office of the Inspector General, including at the site of the custodian indicated in Appendix D, for the purpose of inspecting to confirm compliance with the terms of this Agreement. |
| 10. | The ACO agrees that any use of CMS data in the creation of any document concerning the purpose specified in this section and Appendix D must adhere to CMS’ current cell size suppression policy. This policy stipulates that no cell (e.g., admittances, discharges, patients, services) representing 10 or fewer beneficiaries may be displayed. Also, no use of percentages or other mathematical formulas may be used if they result in the display of a cell representing 10 or fewer beneficiaries. |
| 11. | The ACO agrees to report any breach of personal health information (PHI) or personally identifiable information (PII) from or derived from the CMS data files, loss of these data or improper use or disclosure of such data to the CMS Action Desk by telephone at (410) 786-2850 or by email notification at cms_it_service_desk@cms.hhs.gov within one hour. Furthermore, the ACO agrees to cooperate fully in any federal incident security process that results from such improper use or disclosure. |
| 29 |
| 12. | The parties mutually agree that the individual named in Appendix D is designated as Custodian of the CMS data files on behalf of the ACO and will be responsible for the observance of all conditions of use and disclosure of such data and any derivative data files, and for the establishment and maintenance of security arrangements as specified in this Agreement to prevent unauthorized use or disclosure. Furthermore, such Custodian is responsible for contractually binding any downstream recipients of such data to the terms and conditions in this agreement as a condition of receiving such data. The ACO agrees to notify CMS within fifteen (15) days of any change of custodianship. The parties mutually agree that CMS may disapprove the appointment of a custodian or may require the appointment of a new custodian at any time. |
| 13. | Data disclosed to the ACO pursuant to Appendix D may be retained by the ACO until the termination of this Agreement. The ACO is permitted to retain any individually identifiable health information from such data files or derivative data files after the termination of the Agreement if the ACO is a HIPAA CE, and the data has been incorporated into the subject beneficiaries’ medical records that are part of a designated record set under HIPAA. Furthermore, any HIPAA CE to whom the ACO provides such data in the course of carrying out the Model initiative may also retain such data if the recipient entity is a HIPAA CE or BA and the data is incorporated into the subject beneficiaries’ medical records that are part of a designated record set under HIPAA. The ACO shall destroy all other data and send written certification of the destruction of the data files and/or any derivative data files to CMS within 30 days following the termination of the Agreement. Except for disclosures for treatment purposes, the ACO shall bind any downstream recipients to these terms and conditions as a condition of disclosing such data to downstream entities and permitting them to retain such records under this paragraph. These retention provisions survive termination of the Agreement. |
| C. | De-Identified Reports |
CMS will provide the following reports to the ACO, which will be de-identified in accordance with HIPAA requirements in 45 CFR 164.514(b):
| 1. | Monthly Financial Reports |
These reports will include monthly and year-to-date information on total Medicare expenditures and expenditures for selected categories of services for Next Generation Beneficiaries. This aggregate information will not include individually identifiable health information and will incorporate de-identified data from Next Generation Beneficiaries who have opted out of data sharing.
| 2. | Quarterly Benchmark Reports |
CMS will provide quarterly benchmark reports (“BRs”) to the ACO to monitor ACO financial performance throughout the year. The BRs will not contain individually identifiable data. The design and data source used to generate the BRs is also used for the final year-end financial settlement report. In the event that data contained in the BRs conflicts with data provided from any other source, the data in the BRs will control with respect to settlement under Section XIV.B of the Agreement.
| 30 |
| D. | Beneficiary Rights to Opt Out of Data Sharing |
| 1. | The ACO shall provide Next Generation Beneficiaries who inquire about and wish to modify their preferences regarding claims data sharing for care coordination and quality improvement purposes with information about how to modify their data sharing preferences via 1-800-MEDICARE. Such communications shall note that, even if a Next Generation Beneficiary has elected to decline claims data sharing, CMS may still engage in certain limited data sharing for quality improvement purposes. |
| 2. | The ACO shall allow Next Generation Beneficiaries to reverse a data sharing preference at any time by calling 1-800-MEDICARE. |
| 3. | CMS will maintain the data sharing preferences of Next Generation Beneficiaries who elect to decline data sharing in this Model, the MSSP, or the Pioneer ACO Model. |
| 4. | The ACO may affirmatively contact a Next Generation Beneficiary who has elected to decline claims data sharing no more than one time in a given Performance Year to provide information regarding data sharing. Such contact includes mailings, phone calls, electronic communications, or other methods of communicating with Next Generation Beneficiaries outside of a clinical setting. |
| 5. | In the event that a Next Generation Professional is terminated from the ACO for any reason, if that departing Next Generation Professional is the sole Next Generation Professional in the ACO to have submitted claims for a particular Next Generation Beneficiary during the 12-month period prior to the effective date of the termination, CMS will administratively opt the Next Generation Beneficiary out of all claims data-sharing under this Section VI within 30 days of the effective date of the termination, unless— |
| (a) | The Next Generation Beneficiary affirmatively consents to continued data sharing of such claims with the ACO through an authorization that meets the requirements under 45 CFR 164.508(b); or |
| (b) | The Next Generation Beneficiary has become the patient of another Next Generation Professional participating in the ACO. |
| 6. | Notwithstanding the foregoing, an ACO shall receive claims data regarding substance abuse treatment only if the Next Generation Beneficiary has not elected to decline data sharing or otherwise been opted out of data sharing and has also submitted a CMS-approved form pursuant to Section VI.E of this Agreement. |
| 7. | CMS will administratively opt a Next Generation Beneficiary back into such claims data sharing if they were administratively opted out of data sharing solely due to the termination of a Next Generation Professional within the given ACO. That is, if he or she is subsequently aligned to the ACO, unless the Next Generation Beneficiary affirmatively opts out of data sharing according to this Section VI.C. |
| 31 |
| E. | Beneficiary Substance Abuse Data Opt-In |
| 1. | The ACO may inform each newly-aligned Next Generation Beneficiary, in compliance with applicable law: |
| (a) | That he or she may elect to allow the ACO to receive beneficiary-identifiable data regarding his or her utilization of substance abuse services; |
| (b) | Of the mechanism by which the Next Generation Beneficiary can make this election; and |
| (c) | That 1-800-Medicare will answer any questions regarding data sharing of substance abuse services. |
| 2. | A Next Generation Beneficiary may opt in to substance abuse data sharing only by submitting a CMS-approved substance abuse opt in form to the ACO. The ACO shall promptly send the opt-in form to CMS. |
| F. | Certification of Data and Information |
| 1. | With respect to data and information that are generated or submitted by the ACO, Next Generation Participants, Preferred Providers, or other individuals or entities performing functions or services related to ACO Activities, the ACO shall ensure that an individual with the authority to legally bind the individual or entity submitting such data or information certifies the accuracy, completeness, and truthfulness of the data and information to the best of his or her knowledge information, and belief. Such certifications are a condition of receiving Shared Savings and Other Monies Owed. |
| 2. | At the end of each performance year, an individual with the legal authority to bind the ACO must certify to the best of his or her knowledge, information, and belief— |
| (a) | That the ACO, its Next Generation Participants, its Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities are in compliance with program requirements; and |
| (b) | The accuracy, completeness, and truthfulness of all data and information that are generated or submitted by the ACO, Next Generation Participants, Preferred Providers, or other individuals or entities performing functions or services related to ACO Activities, including any quality data or other information or data relied upon by CMS in determining the ACO's eligibility for, and the amount of Shared Savings, or the amount of Shared Savings or Other Monies Owed. |
| 32 |
| VII. | Care Improvement Objectives |
| A. | General |
| 1. | The ACO shall implement processes and protocols that relate to the following objectives for patient-centered care: |
| (a) | Promotion of evidence-based medicine, such as through the establishment and implementation of evidence-based guidelines at the organizational or institutional level. An evidence-based approach would also regularly assess and update such guidelines. |
| (b) | Process to ensure Beneficiary/caregiver engagement, and shared decision making processes employed by Next Generation Participants that takes into account the Beneficiaries' unique needs, preferences, values, and priorities. Measures for promoting Beneficiary engagement include, but are not limited to, the use of decision support tools and shared decision making methods with which the Beneficiary can assess the merits of various treatment options in the context of his or her values and convictions. Beneficiary engagement also includes methods for fostering what might be termed "health literacy" in Beneficiaries and their families. |
| (c) | Coordination of Beneficiaries’ care and care transitions (e.g., sharing of electronic summary records across providers, telehealth, remote Beneficiary monitoring, and other enabling technologies). |
| (d) | Providing Beneficiaries access to their own medical records and to clinical knowledge so that they may make informed choices about their care. |
| (e) | Ensuring individualized care for Beneficiaries, such as through personalized care plans. |
| (f) | Routine assessment of Beneficiary and caregiver and/or family experience of care and seek to improve where possible. |
| (g) | Providing care that is integrated with the community resources Beneficiaries require. |
| 2. | The ACO shall require its Next Generation Participants to comply with and implement these designated processes and protocols, and shall institute remedial processes and penalties, as appropriate, for Next Generation Participants that fail to comply with or implement a required process or protocol. |
| B. | Outcomes-Based Contracts with Other Purchasers |
| 1. | CMS may require the ACO to report to CMS, in a manner and by a date determined by CMS, information regarding the scope of outcomes-based contracts held by the ACO and/or its Next Generation Participants with non- Medicare Purchasers. For purposes of this provision, outcomes-based contracts mean contracts that evaluate Beneficiary experiences of care, include financial accountability (e.g., shared savings or financial risk) and/or quality performance standards. |
| 33 |
| 2. | Notwithstanding other sections of this Agreement, failure to comply with this Section VII.B.2 may result in CMS imposing appropriate remedial actions under Section XIX.A but shall not be cause for CMS to terminate this Agreement. |
| VIII. | ACO Quality Performance |
| A. | Quality Scores |
CMS shall use the ACO’s quality scores calculated under this Section to determine, in part, the ACO’s Performance Year Benchmark according to the methodology described in Appendix B.
| B. | Quality Measures |
CMS shall assess quality performance using the quality measures set forth in Appendix F and the quality measure data reported by the ACO. Notwithstanding Section XXI.D, CMS may amend the quality measures to be used in a Performance Year without the consent of the ACO prior to the beginning of the Performance Year. CMS shall notify the ACO of any measure set change prior to the beginning of each Performance Year.
| C. | Quality Measure Reporting |
| 1. | Except as set forth in paragraph 2, the ACO shall completely, timely, and accurately report quality measures for each Performance Year and shall require its Next Generation Participants to cooperate in quality measure reporting. Complete reporting means that the ACO meets all of the reporting requirements including timing and reporting the requested data for all measures. |
| 2. | The ACO shall not report quality measures data on behalf of its Next Generation Participants unless it remains in the Model for the entire Performance year with financial risk. |
| 3. | CMS shall use the following sources for quality reporting: |
| (a) | ACO reporting via the Group Practice Reporting Option (GPRO) Web Interface tool; |
| (b) | ACO reporting of results from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) or other patient experience surveys; |
| (c) | Medicare claims submitted for service to Next Generation Beneficiaries; and |
| (d) | Any other relevant data shared between the ACO and CMS pursuant to this Agreement. |
| 4. | For each Performance Year, the ACO is responsible for procuring a CMS- approved vendor to conduct the CAHPS or other patient experience surveys. The ACO is responsible for paying for the surveys for ensuring that the survey results are transmitted to CMS by a date and in a manner established by CMS. |
| 34 |
| D. | Quality Performance Scoring |
| 1. | CMS shall use the ACO’s performance on each of the quality measures to calculate the ACO’s total quality score according to a methodology to be determined by CMS prior to the start of each Performance Year. |
| 2. | Prior to the start of each Performance Year, CMS shall notify the ACO of the methodology for calculating the quality performance benchmarks and the methodology for calculating the ACO’s total quality score for that Performance Year. Notwithstanding Section XXI.D, CMS may amend these methodologies without the consent of the ACO prior to the beginning of each Performance Year. |
| 3. | Starting in the ACO’s second Performance Year in the Model, the ACO’s quality score may be adjusted downward based on quality measure validation (“QMV”) findings. Prior to the start of the ACO’s second Performance Year and each subsequent Performance Year, CMS will provide additional information regarding how the quality score will be adjusted based on the QMV findings. |
| IX. | Use of Certified EHR Technology |
Beginning in 2017, the ACO and its Next Generation Participants shall use certified EHR technology (as defined in section 1848(o)(4) of the Act) in a manner sufficient to meet the requirements for an “eligible alternative payment entity” under section 1833(z)(3)(D)(i)(I) of the Act (added by section 101(e)(2) of the Medicare Access and CHIP Reauthorization Act of 2015) as prescribed through regulation.
| X. | ACO Selections and Approval |
| A. | ACO Selections |
For each Performance Year, by one or more deadlines and in a manner determined by CMS in advance of the relevant Performance Year, the ACO shall submit to CMS its selections for the following:
| 1. | The ACO’s selected Risk Arrangement from the alternatives described in Appendix B; |
| 2. | The ACO’s selected Savings/Loss Cap, between 5.0% and 15%; |
| 3. | The ACO’s selected Alternative Payment Mechanism, if any; |
| 4. | The Benefit Enhancements, if any, that it elects to offer through its Next Generation Participants and Preferred Providers; and |
| 5. | The ACO’s decision with respect to participation in Voluntary Alignment pursuant to Section V.C and Appendix C. |
| 35 |
| B. | Risk Arrangement and Savings/Loss Cap Approval |
The ACO’s Risk Arrangement and Savings/Loss Cap selection for the first Performance Year, and for each subsequent Performance Year, shall be deemed approved unless rejected in writing by CMS within 30 days after submission.
| C. | Alternative Payment Mechanism Approval |
| 1. | If the ACO selects an Alternative Payment Mechanism for a Performance Year, CMS shall send the ACO written notice of approval or rejection of the selected Alternative Payment Mechanism within 15 days after the ACO submission of its Alternative Payment Mechanism selection. In the event that CMS does not send such written notice within 15 days after the ACO submission of its selection, the ACO’s selection shall be deemed approved. |
| 2. | CMS shall assess the ACO’s Alternative Payment Mechanism selection according to the eligibility criteria set forth in Appendix G or H, whichever is relevant. |
| XI. | Benefit Enhancements |
| A. | General |
| 1. | The ACO may elect to provide one or more Benefit Enhancements for a Performance Year. The ACO shall submit an “Implementation Plan” to CMS in a manner and by a date determined by CMS for each Benefit Enhancement for the first time that Benefit Enhancement is elected under Section X by the ACO. |
| 2. | If the ACO elects to provide one or more Benefit Enhancements for a Performance Year, the ACO’s Next Generation Participants and Preferred Providers, as indicated on the relevant Participant List and Preferred Provider List under Section IV, may submit claims for services furnished pursuant to a Benefit Enhancement as described in this Section during the Performance Year for which the ACO elected to provide the Benefit Enhancement. Appendices I, J, and K shall apply to this Agreement only if the ACO elected under Section X to provide the relevant Benefit Enhancement for a given Performance Year. |
| 3. | CMS may require the ACO to report data on the use of Benefit Enhancements to CMS. Such data shall be reported in a form in manner to be determined by CMS. |
| B. | 3-Day SNF Rule Waiver Benefit Enhancement |
| 1. | Appendix I shall apply to this Agreement for any Performance Year for which the ACO submits an Implementation Plan for the 3-Day SNF Rule Waiver Benefit Enhancement. |
| 2. | The ACO shall require that, in order to be eligible to submit claims for services furnished to Next Generation Beneficiaries pursuant to the 3-Day SNF Rule Waiver Benefit Enhancement, an entity must be: |
| (a) | A Next Generation Participant or Preferred Provider; and |
| 36 |
| (b) | A skilled-nursing facility (“SNF”) or a hospital or critical access hospital that has swing-bed approval for SNF services (“Swing-Bed Hospital”); and |
| (c) | Designated on the Participant List or Preferred Provider List as participating in the 3-Day SNF Rule Waiver Benefit Enhancement; and |
| (d) | Approved by CMS according to the criteria described in Appendix I. |
| 3. | If CMS notifies the ACO that a SNF or Swing-Bed Hospital has not been approved for participation in the 3-Day SNF Rule Waiver Benefit Enhancement under this Section XI.B, but the provider is otherwise eligible to be a Next Generation Participant or Preferred Provider, the ACO may either remove the provider from the Participant List or Preferred Provider List, or amend the relevant list to reflect that the provider will not participate in the 3-Day SNF Rule Waiver Benefit Enhancement. The ACO shall amend the relevant list no later than 30 days after the date of the notice from CMS. |
| C. | Telehealth Expansion |
| 1. | Appendix J shall apply to this Agreement for any Performance Year for which the ACO submits an Implementation Plan for the Telehealth Expansion Benefit Enhancement. |
| 2. | In order to be eligible to bill for telehealth services furnished to Next Generation Beneficiaries pursuant to the Telehealth Expansion Benefit Enhancement, an individual or entity must be: |
| (a) | A Next Generation Professional or Preferred Provider [who is a physician or other practitioner]; and |
| (b) | Authorized under relevant Medicare rules and state law to bill for telehealth services; and |
| (c) | Designated on the Participant List or Preferred Provider List as participating in the Telehealth Expansion Benefit Enhancement; and |
| (d) | Approved by CMS according to the criteria described in Appendix J. |
| 3. | The ACO shall ensure that Next Generation Participants and Preferred Providers do not substitute telehealth services for in-person services when in-person services are more clinically appropriate. |
| 4. | The ACO shall ensure that Next Generation Participants and Preferred Providers only furnish Medically Necessary telehealth services and do not use telehealth services to prevent or deter a Beneficiary from seeking or receiving in-person care when such care is Medically Necessary. |
| D. | Post-Discharge Home Visits |
| 1. | Appendix K shall apply to this Agreement for any Performance Year for which the ACO submits an Implementation Plan for the Post-Discharge Home Visits Benefit Enhancement. |
| 37 |
| 2. | In order to be eligible to submit claims for post-discharge home visits furnished to Next Generation Beneficiaries pursuant to the Post-Discharge Home Visit Benefit Enhancement, the supervising physician or other practitioner must be: |
| (a) | A Next Generation Professional or a physician or non-physician practitioner who is a Preferred Provider; and |
| (b) | Eligible under Medicare rules to submit claims for “incident to” services as defined in Chapter 15, Section 60 of the Medicare Benefit Policy Manual; and |
| (c) | Designated on the Next Generation Participant List or Preferred Provider List as participating in the Post-Discharge Home Visit Benefit Enhancement. |
| 3. | The individual performing services under this Benefit Enhancement must be “auxiliary personnel” as defined at 42 CFR § 410.26(a)(1). |
| 4. | The ACO shall ensure that post-discharge home visits are not used to prevent or deter a Beneficiary from seeking or receiving other Medically Necessary care. |
| E. | Requirements for Termination of Benefit Enhancements |
| 1. | The ACO must obtain CMS consent before voluntarily discontinuing any Benefit Enhancement during a Performance Year. |
| 2. | In the event that during a Performance Year a Benefit Enhancement will cease to be in effect with respect to the ACO or any Next Generation Participant or Preferred Provider pursuant to Section XIX, the effective date of such termination shall be the date specified by CMS in the notice to the ACO. |
| (a) | Within 30 days after the effective date of termination, the ACO shall send notice in writing to the affected Beneficiaries and/or Next Generation Beneficiaries. Such notification shall state that following a date that is 90 days after the effective date of termination or the end of the Performance Year, whichever is sooner, the Benefit Enhancement will no longer be covered by Medicare and the Beneficiary may be responsible for the payment of such services. |
| (b) | CMS shall cease coverage of claims for a terminated Benefit Enhancement 90 days after the effective date of such termination. |
| 3. | In the event that the ACO elects to discontinue a Benefit Enhancement through the selection process under Section X of this Agreement, the ACO shall notify all its Next Generation Participants and Preferred Providers no later than 30 days prior to the start of the subsequent Performance Year. |
| F. | Termination of Benefit Enhancements upon Termination |
If this Agreement is terminated by either party prior to the end of a Performance Year, CMS shall terminate the ACO’s Benefit Enhancements and the ACO shall notify its Next Generation Beneficiaries in accordance with Section XI.E. The ACO shall also notify its Next Generation Participants and Preferred Providers within 10 business days after the effective date of the termination.
| 38 |
| XII. | Coordinated Care Reward |
| A. | Reward Payment |
CMS may make direct Coordinated Care Reward payments directly to eligible Beneficiaries and Next Generation Beneficiaries. CMS will determine the methodology for calculating which Beneficiaries are eligible to receive the payment, the amount of the payment, and the manner in which the payment will be issued.
| B. | ACO Obligations and Limitations Regarding the Coordinated Care Reward |
| 1. | In any Performance Year in which CMS elects to make Coordinated Care Reward payments, the ACO shall ensure that all Next Generation Participants and Preferred Providers will, upon any Next Generation Beneficiary’s inquiry about the Coordinated Care Reward, provide an accurate and current list of all Next Generation Participants and Preferred Providers, either in hard copy or by reference to the ACO’s website, to the Next Generation Beneficiary. |
| 2. | In any Performance Year in which CMS elects to make Coordinated Care Reward payments, the ACO shall ensure that all Next Generation Beneficiaries will be directed by the ACO, Next Generation Participants, Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities to 1-800-MEDICARE to obtain additional information about the Coordinated Care Reward. |
| 3. | In any Performance Year in which CMS elects to make Coordinated Care Reward payments, the ACO and its Next Generation Participants and Preferred Providers may communicate in writing with Next Generation Beneficiaries regarding the coordinated care reward. Any such written materials must comply with the requirements under Section V.E of this Agreement. |
| 4. | In any Performance Year in which CMS elects to make Coordinated Care Reward payments, the ACO shall ensure that any communication with Next Generation Beneficiaries regarding the Coordinated Care Reward, whether by the ACO, a Next Generation Participant, or Preferred Provider, clearly conveys that CMS is solely responsible for the terms and payment of the coordinated care reward and that the reward does not limit the Beneficiaries’ freedom of choice of Medicare providers and suppliers. |
| 5. | The ACO shall not, and shall ensure that its Next Generation Participants, Preferred Providers, and any other individuals or entities performing services related to ACO Activities do not, provide gifts or other remuneration to Next Generation Beneficiaries as inducements for receiving the Coordinated Care Reward or to influence a Next Generation Beneficiary’s decision to qualify for the Coordinated Care Reward. |
| 39 |
| XIII. | ACO Benchmark |
| A. | Prospective Benchmark |
| 1. | For each Performance Year, CMS shall determine the ACO’s Performance Year Benchmark according the methodology in Appendix B. |
| 2. | No later than 15 days before the beginning of each Performance Year, CMS shall provide the ACO with a report (“Performance Year Benchmark Report”) consisting of the ACO’s Performance Year Benchmark. |
| 3. | On a quarterly basis during each Performance Year, CMS shall provide the ACO with a financial report (“Quarterly Financial Report”). The Quarterly Financial Report may comprise adjustments to the Performance Year Benchmark resulting from updated information regarding any factors that affect the Performance Year Benchmark calculation in Appendix B. |
| B. | Trend Adjustments |
| 1. | At its sole discretion, CMS may make retroactive adjustments to the Performance Year Benchmark if CMS determines any policies and/or events during the Performance Year render the trend used in calculating the Performance Year Benchmark inaccurate or inappropriate for payment purposes. |
| 2. | If CMS determines that any such policies and/or events have occurred, CMS shall adjust the Performance Year Benchmark according to the methodology in Appendix B. |
| 3. | CMS shall make a reasonable effort to notify the ACO of any adjustments to the Performance Year Benchmark made under this Section XIII.B. Such notification shall not limit CMS’ discretion to make determinations regarding retroactive adjustment under this Section. |
| 4. | In order to accommodate the trend adjustment, CMS may at its sole discretion delay settlement under Section XIV.C of this Agreement for the affected Performance Year for no more than 60 days. |
| 5. | Except for revisions made pursuant to Section XIV.C.4, no trend adjustments shall be made under this Section XIII.B after the issuance of the settlement report for the relevant Performance Year. |
| XIV. | Payment |
| A. | General |
For each Performance Year, CMS shall pay the ACO in accordance with (i) the Alternative Payment Mechanism, if any, for which CMS has approved the ACO under Section X; (ii) the Risk Arrangement for which the ACO has been approved or deemed approved by CMS under Section X.B; (iii) Appendix B; (iv) Section XIII; and (v) this Section XIV.
| 40 |
| B. | Alternative Payment Mechanisms |
| 1. | General |
| (a) | The ACO may elect to receive only one Alternative Payment Mechanism. The ACO shall select such Alternative Payment Mechanism, if any, and CMS shall approve or reject the ACO’s selection, in accordance with Section X. |
| (b) | By the deadline specified by CMS, the ACO shall submit to CMS a financial disclosure statement demonstrating sufficient financial reserves to repay Other Monies Owed incurred as a result of participation in an Alternative Payment Mechanism. |
| 2. | Infrastructure Payments |
| (a) | If the ACO selects and CMS approves participation in Infrastructure Payments, CMS shall make payments to the ACO in accordance with the methodology in Appendix G. |
| (b) | The ACO shall spend the amounts received as Infrastructure Payments only on ACO Activities. |
| (c) | The ACO shall repay CMS all Infrastructure Payments it received during a Performance Year as Other Monies Owed at the Performance Year settlement or through settlement reports issued at such other times under Section XIV.C. |
| 3. | Population-Based Payments (PBP) |
| (a) | If the ACO wishes to participate in PBP, it must elect PBP as an Alternative Payment Mechanism in accordance with Section I.A. of Appendix H. CMS shall review and respond to the ACO’s election in accordance with Sections I.A and I.B. of Appendix H. |
| (b) | If CMS approves the ACO's election to participate in PBP, CMS shall make Monthly PBP Payments to the ACO in accordance with the methodology in Appendix H. Each party shall comply with the terms of Appendix H that are applicable to that party. |
| (c) | As part of settlement for a Performance Year under Section XIV.C, CMS shall calculate the difference between the total Monthly PBP Payments amounts that CMS paid the ACO during the Performance Year and the total amount of PBP Fee Reductions. Such calculations shall be made in accordance with Appendix H. Any difference would constitute Other Monies Owed and may be subject to recoupment or offset in accordance with Appendix H and Section XIV.C of this Agreement. |
| 4. | All-Inclusive Population-Based Payments (AIPBP) |
| (a) | If the ACO wishes to participate in AIPBP, it must elect AIPBP as an Alternative Payment Mechanism in accordance with Section I.A of Appendix N. CMS shall review and respond to the ACO’s election in accordance with Sections I.A and I.B of Appendix N. |
| 41 |
| (b) | If CMS approves the ACO’s election to participate in AIPBP, CMS shall make Monthly AIPBP Payments to the ACO in accordance with the methodology in Appendix N. Each party shall comply with the terms of Appendix N that are applicable to that party. |
| (c) | As part of settlement for a Performance Year under Section XIV.C, CMS shall calculate the difference between the total Monthly AIPBP Payments that CMS paid to the ACO during the Performance Year and the total amount of AIPBP Fee Reductions in accordance with Appendix N. Such calculations shall be made in accordance with Appendix N. Any difference would constitute Other Monies Owed and may be subject to recoupment or offset in accordance with Appendix N and Section XIV.C of this Agreement. |
| C. | Settlement |
| 1. | General |
| (a) | Following the end of each Performance Year, and at such other times as may be required under this Agreement, CMS will issue a settlement report to the ACO setting forth the amount of any Shared Savings or Shared Losses and the amount of Other Monies Owed. CMS shall calculate Shared Savings, Shared Losses, and Other Monies Owed according to the methodology in Appendix B. |
| (b) | CMS shall make reasonable efforts to issue the settlement report for each Performance Year no later than 240 days after the end of the Performance Year. |
| (c) | Any amounts determined to be owed as a result of a settlement or revised settlement upon reopening shall be paid in accordance with Section XIV.C.5. |
| 2. | Error Notice |
| (a) | The settlement report will be deemed final 30 days after the date it is issued, unless the ACO submits to CMS written notice of an error in the mathematical calculations in the settlement report within 30 days after the settlement report is issued (“Timely Error Notice”). |
| (b) | Upon receipt of a Timely Error Notice, CMS shall review the calculations in question and any mathematical issues raised by the ACO in its written notice. |
| (c) | If CMS issues a written determination that the settlement report is correct, the settlement report is final on the date the written determination is issued. |
| (d) | If CMS issues a revised settlement report, the revised settlement report is final on the date it is issued. |
| (e) | There shall be no further administrative or judicial review of the settlement report or a revised settlement report. |
| 42 |
| 3. | Deferred Settlement |
| (a) | The ACO may elect, in a manner and by a date specified by CMS, to defer settlement for a period not to exceed 180 days (“Deferred Settlement”). |
| (b) | As a condition of Deferred Settlement, CMS may require the ACO to increase the amount of its financial guarantee under Section XIV.D in an amount and by a date determined by CMS. |
| 4. | Settlement Reopening |
| (a) | For a given Performance Year, for a period of one year following issuance of the settlement report for that performance year, or until issuance of the settlement report for the subsequent performance year, whichever comes earlier, CMS reserves the right to reopen the settlement report in order to include payments or recoupments specified in Section 3.9 of Appendix B that were not included in the initial settlement, issue a revised settlement report, and make or demand payment of any additional amounts owed to or by the ACO. |
| (b) | CMS reserves the right, for a period of six years following the end of the term or termination of this Agreement, to reopen a final settlement report in order to recalculate the amounts owed, issue a revised settlement report, and make or demand payment of any additional amounts owed to or by the ACO if, as a result of later inspection, evaluation, investigation, or audit, it is determined that the amount due to the ACO by CMS or due to CMS by the ACO has been calculated in error due to CMS data source file errors, computational errors, or other similar CMS technical errors. |
| (c) | The parties shall pay any amounts determined to be owed as a result of a reopening under this Section XIV.C.4 in accordance with Section XIV.C.5. |
| (d) | CMS may reopen and revise a settlement report at any time in the event of fraud or similar fault by the ACO, a Next Generation Participant or Preferred Provider. |
| 5. | Payment of Amounts Owed |
| (a) | If CMS owes the ACO Shared Savings or Other Monies Owed as a result of a final settlement, or revised settlement upon reopening, CMS shall pay the ACO in full within 30 days after the date on which the relevant settlement report is deemed final, except that CMS shall not make any payment of Shared Savings if this Agreement is terminated by CMS pursuant to Section XIX, and CMS may reduce amounts owed to the ACO under this Agreement by amounts owed by the ACO under this Agreement or any other CMS program or initiative. |
| (b) | If the ACO owes CMS Shared Losses or Other Monies Owed as a result of a final settlement, or revised settlement upon reopening, the ACO shall pay CMS in full within 30 days after the relevant settlement report is deemed final. |
| 43 |
| (c) | If CMS does not timely receive payment in full, the remaining amount owed will be considered a delinquent debt subject to the provisions of Section XIV.E. |
| 6. | Transition from the ACO Investment Model (AIM) |
If the ACO participated in AIM prior to the Start Date, the ACO shall be responsible for repayment of all Pre-Paid Shared Savings (as such term is defined in the AIM agreement) owed to CMS according to the terms of the AIM Agreement. Notwithstanding the terms of the AIM Agreement, CMS may deduct such amounts from any Shared Savings earned by the ACO during settlement under the Next Generation ACO Model.
| D. | Financial Guarantee |
| 1. | The ACO must have the ability to repay all Shared Losses and Other Monies Owed for which it may be liable under the terms of this Agreement and shall provide a financial guarantee for each Performance Year in accordance with the terms set forth in Appendix L. |
| 2. | The ACO shall submit such documentation of such financial guarantee for the first Performance Year to CMS by a date determined by CMS, and thereafter in accordance with Appendix L. |
| 3. | Any changes made to a financial guarantee must be approved in advance by CMS. |
| 4. | Nothing in this Agreement or its Appendices shall be construed to limit the ACO’s liability to pay any Shared Losses or Other Monies Owed in excess of the guarantee amount. |
| E. | Delinquent Debt |
| 1. | If CMS does not receive payment in full by the date payment is due, CMS shall pursue payment under the financial guarantee required under Section XIV.D and may withhold payments otherwise owed to the ACO under this Agreement or any other CMS program or initiative. |
| 2. | If the ACO fails to pay the amounts due CMS in full within 30 days after the date of a demand letter or settlement report, CMS shall assess simple interest on the unpaid balance at the rate applicable to other Medicare debts under 45 CFR § 30.18 and 42 CFR § 405.378. Interest shall be calculated in 30-day periods and shall be assessed for each 30-day period that payment is not made in full. |
| 3. | CMS and the U.S. Department of the Treasury may use any applicable debt collection tools available to collect the total amount owed by the ACO. |
| 44 |
| XV. | Participation in Evaluation, Shared Learning Activities, and Site Visits |
| A. | Evaluation Requirement |
| 1. | General |
| (a) | The ACO shall participate and cooperate in any independent evaluation activities conducted by CMS and/or its designees aimed at assessing the impact of the Model on the goals of better health, better health care, and lower Medicare per capita costs for Next Generation Beneficiaries. The ACO shall require its Next Generation Participants and Preferred Providers to participate and cooperate in any such independent evaluation activities conducted by CMS and/or its designees. |
| (b) | The ACO shall ensure that it has written agreements and/or legal relationships with any individuals and entities performing functions and services related to ACO Activities, that are necessary to ensure CMS or its designees can carry out evaluation activities. |
| 2. | Primary Data |
In its evaluation activities, CMS may collect qualitative and quantitative data from the following sources:
| (a) | Site visits; |
| (b) | Interviews with Next Generation Beneficiaries and their caregivers; |
| (c) | Focus groups of Next Generation Beneficiaries and their caregivers; |
| (d) | Interviews with ACO, Next Generation Participant and Preferred Provider staff; |
| (e) | Focus groups with ACO, Next Generation Participant and Preferred Provider staff; |
| (f) | Direct observation of Beneficiary interactions with Next Generation Participant and Preferred Provider staff, care management meetings among Next Generation Participant and Preferred Provider staff, and other activities related to the ACO’s participation in the Model; and |
| (g) | Surveys. |
| 3. | Secondary Data |
In its evaluation activities, CMS may use data or information submitted by the ACO as well as claims submitted to CMS for items and services furnished to Next Generation Beneficiaries. This data may include, but is not limited to:
| (a) | Survey data from CAHPS surveys; |
| (b) | Clinical data such as lab values; |
| (c) | Medical records; and |
| (d) | ACO Implementation Plans. |
| 45 |
| B. | Shared Learning Activities |
| 1. | The ACO shall participate in CMS-sponsored learning activities designed to strengthen results and share learning that emerges from participation in the Model. |
| 2. | The ACO shall participate in periodic conference calls, site visits, and virtual or in-person meetings, and actively share resources, tools and ideas as prescribed by CMS. |
| C. | Site Visits |
| 1. | The ACO shall cooperate in periodic site visits by CMS and/or its designees in order to facilitate evaluation, shared learning activities, or the fulfilment of the terms of this Agreement. |
| 2. | CMS shall schedule site visits with the ACO no fewer than 15 days in advance. To the extent practicable, CMS will attempt to accommodate the ACO’s request for particular dates in scheduling site visits. However, the ACO may not request a date that is more than 60 days after the date of the initial site visit notice from CMS. |
| 3. | The ACO shall ensure that personnel with the appropriate responsibilities and knowledge associated with the purpose of the site visit are available during site visits. |
| 4. | Notwithstanding the foregoing, CMS may perform unannounced site visits at the office of any Next Generation Participant or Preferred Provider at any time to investigate concerns about the health or safety of Next Generation Beneficiaries or other program integrity issues. |
| 5. | Nothing in this Agreement shall be construed to limit or otherwise prevent CMS from performing site visits permitted by applicable law or regulations. |
| D. | Rights in Data and Intellectual Property |
| 1. | CMS may use any data obtained pursuant to the Next Generation ACO Model to evaluate the Model and to disseminate quantitative results and successful care management techniques, to other providers and suppliers and the public. Data to be disseminated may include results of patient experience of care and quality of life surveys as well as measures based upon claims and medical records. The ACO will be permitted to comment on evaluation reports for factual accuracy but may not edit conclusions or control the dissemination of reports. |
| 2. | Notwithstanding any other provision in this Agreement, all proprietary trade secret information and technology of the ACO or its Next Generation Participants and Preferred Providers is and shall remain the sole property of the ACO, the Next Generation Participant, or Preferred Provider and, except as required by federal law, shall not be released by CMS without the express written consent of the ACO. The regulation at 48 CFR § 52.227-14, “Rights in Data-General” is hereby incorporated by reference into this Agreement. CMS does not acquire by license or otherwise, whether express or implied, any intellectual property right or other rights to the ACO’s, Next Generation Participants’, or Preferred Providers’ proprietary information or technology. |
| 46 |
| 3. | The ACO acknowledges that it has submitted to CMS a form identifying specific examples of what it considers proprietary and confidential information currently contained in its program that should not be publicly disclosed. This form is attached as Appendix M. |
| XVI. | Public Reporting and Release of Information |
| A. | ACO Public Reporting and Transparency |
The ACO shall report the following information on a publicly accessible website maintained by the ACO. CMS may publish some or all of this information on the CMS website.
| 1. | Organizational information including all of the following: |
| (a) | Name and location of the ACO; |
| (b) | Primary contact information for the ACO; |
| (c) | Identification of all Next Generation Participants and Preferred Providers; |
| (d) | Identification of all joint ventures between or among the ACO and any of its Next Generation Participants and Preferred Providers; |
| (e) | Identification of the ACO’s key clinical and administrative leaders and the name of any company by which they are employed; and |
| (f) | Identification of members of the ACO’s governing body and the name of any entity by which they are employed. |
| 2. | Shared Savings and Shared Losses information, including: |
| (a) | The amount of any Shared Savings or Shared Losses for any Performance Year; |
| (b) | The proportion of Shared Savings invested in infrastructure, redesigned care processes, and other resources necessary to improve outcomes and reduce Medicare costs for Beneficiaries; and |
| (c) | The proportion of Shared Savings distributed to Next Generation Participants and Preferred Providers. |
| 3. | The ACO’s performance on the quality measures described in Appendix F. |
| B. | ACO Release of Information |
| 1. | The ACO, its Next Generation Participants, and Preferred Providers shall obtain prior approval from CMS during the term of this Agreement and for six months thereafter for the publication or release of any press release, external report or statistical/analytical material that materially and substantially references the ACO’s participation in the Model or the ACO’s financial arrangement with CMS. External reports and statistical/analytical material may include, but are not limited to, papers, articles, professional publications, speeches, and testimony. |
| 47 |
| 2. | All external reports and statistical/analytical material that are subject to this section must include the following statement on the first page: “The statements contained in this document are solely those of the authors and do not necessarily reflect the views or policies of CMS. The authors assume responsibility for the accuracy and completeness of the information contained in this document.” |
| XVII. | Compliance and Oversight |
| A. | ACO Compliance Plan |
| 1. | The ACO shall have a compliance plan that includes at least the following elements: |
| (a) | A designated compliance official or individual who is not legal counsel to the ACO and reports directly to the ACO's governing body; |
| (b) | Mechanisms for identifying and addressing compliance problems related to the ACO's operations and performance; |
| (c) | A method for employees or contractors of the ACO, its Next Generation Participants and Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities to anonymously report suspected problems related to the ACO to the compliance official; |
| (d) | Compliance training for the ACO and its Next Generation Participants and Preferred Providers; |
| (e) | A requirement for the ACO to report probable violations of law to an appropriate law enforcement agency. |
| 2. | The ACO's compliance plan must be in compliance with all applicable laws and regulations and be updated periodically to reflect changes in those laws and regulations. |
| B. | CMS Monitoring and Oversight Activities |
| 1. | CMS shall conduct monitoring activities to evaluate compliance by the ACO, its Next Generation Participants, and Preferred Providers with the terms of this Agreement. Such monitoring activities may include, without limitation: |
| (a) | Interviews with any individual or entity participating in ACO Activities, including members of the ACO leadership and management, Next Generation Participants, and Preferred Providers; |
| (b) | Interviews with Next Generation Beneficiaries and their caregivers; |
| (c) | Audits of charts, medical records, Implementation Plans, and other data from the ACO, its Next Generation Participants and Preferred Providers; |
| (d) | Site visits to the ACO and its Next Generation Participants and Preferred Providers; and |
| 48 |
| (e) | Documentation requests sent to the ACO, its Next Generation Participants, and/or Preferred Providers, including surveys and questionnaires. |
| 2. | In conducting monitoring and oversight activities, CMS or its designees may use any relevant data or information including, without limitation, all Medicare claims submitted for items or services furnished to Next Generation Beneficiaries. |
| 3. | CMS shall, to the extent practicable and as soon as practicable, provide the ACO with a comprehensive schedule of planned comprehensive annual audits related to compliance with this Agreement. |
| (a) | Such schedule does not preclude the ability of CMS to conduct more limited, targeted or ad hoc audits as necessary. |
| (b) | CMS may alter such schedule without the consent of the ACO. CMS shall notify the ACO within 15 days of altering such schedule. |
| C. | ACO Compliance with Monitoring and Oversight Activities |
The ACO shall cooperate with, and the ACO shall require its Next Generation Participants, Preferred Providers and other individuals and entities performing functions and services related to ACO Activities to cooperate with all CMS monitoring and oversight requests and activities.
| D. | Compliance with Laws |
| 1. | Agreement to Comply |
| (a) | The ACO shall comply with, and shall require all Next Generation Participants, Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities to comply with the applicable terms of this Agreement and all applicable statutes regulations, and guidance, including without limitation: (a) federal criminal laws; (b) the False Claims Act (31 U.S.C. § 3729 et seq.); (c) the anti-kickback statute (42 U.S.C. § 1320a-7b(b)); (d) the civil monetary penalties law (42 U.S.C. § 1320a-7a); and (e) the physician self-referral law (42 U.S.C. § 1395nn). |
| (b) | This Agreement does not waive any obligation of the ACO or the ACO’s Next Generation Participants or Preferred Providers to comply with the terms of any other CMS contract, agreement, model, or demonstration. |
| 2. | State Recognition |
During all Performance Years of this Agreement, the ACO shall be in compliance with applicable state licensure requirements in each state in which it operates regarding risk-bearing entities unless it has provided a written attestation to CMS that it is exempt from such state laws. If the ACO is exempt from such laws, it shall submit a certification to CMS no later than 60 days after the Start Date or after the date on which it becomes exempt from any such laws.
| 49 |
| 3. | Reservation of Rights |
| (a) | Nothing contained in this Agreement or in the application process for the Next Generation ACO Model is intended or can be construed as a waiver by the United States Department of Justice, the Internal Revenue Service, the Federal Trade Commission, HHS Office of the Inspector General, or CMS of any right to institute any proceeding or action for violations of any statutes, rules or regulations administered by the Government, or to prevent or limit the rights of the Government to obtain relief under any other federal statutes or regulations, or on account of any violation of this Agreement or any other provision of law. This Agreement cannot be construed to bind any Government agency except CMS and this Agreement binds CMS only to the extent provided herein. |
| (b) | The failure by CMS to require performance of any provision of this Agreement does not affect CMS’s right to require performance at any time thereafter, nor does a waiver of any breach or default of this Agreement constitute a waiver of any subsequent breach or default or a waiver of the provision itself. |
| 4. | Office of Inspector General of the Department of Health and Human Services (OIG) Authority |
None of the provisions of this Agreement limit or restrict the OIG’s authority to audit, evaluate, investigate, or inspect the ACO or its Next Generation Participants and Preferred Providers.
| 5. | Other Government Authority |
None of the provisions of this Agreement limit or restrict any other Government authority that is permitted by law to audit, evaluate, investigate, or inspect the ACO or its Next Generation Participants and Preferred Providers.
| E. | Certification of Data and Information |
| 1. | With respect to data and information generated or submitted to CMS by the ACO, Next Generation Participants, Preferred Providers, or other individuals or entities performing functions or services related to ACO Activities, the ACO shall ensure that an individual with the authority to legally bind the individual or entity submitting such data or information certifies the accuracy, completeness, and truthfulness of that data and information to the best of his or her knowledge information, and belief. Such certifications are a condition of receiving Shared Savings and Other Monies Owed. |
| 2. | At the end of each Performance Year, an individual with the legal authority to bind the ACO must certify to the best of his or her knowledge, information, and belief: |
| 50 |
| (a) | That the ACO, its Next Generation Participants, its Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities are in compliance with program requirements; and |
| (b) | The accuracy, completeness, and truthfulness of all data and information that are generated or submitted by the ACO, Next Generation Participants, Preferred Providers, or other individuals or entities performing functions or services related to ACO Activities, including any quality data or other information or data relied upon by CMS in determining the ACO’s eligibility for, and the amount of Shared Savings, or the amount of Shared Savings or Other Monies Owed. |
| XVIII. | Audits and Record Retention |
| A. | Right to Audit and Correction |
The ACO agrees, and must require all of its Next Generation Participants and Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities to agree, that the Government, including CMS, HHS, and the Comptroller General or their designees, has the right to audit, inspect, investigate, and evaluate any books, contracts, records, documents and other evidence of the ACO and its Next Generation Participants, Preferred Providers, and other individuals or entities performing functions or services related to ACO Activities that pertain to the following:
| 1. | The ACO’s compliance with the terms of this Agreement, including provisions that require the ACO impose duties or requirements on Next Generation Participants or Preferred Providers; |
| 2. | Whether Next Generation Participants and Preferred Providers complied with the duties and requirements imposed on them by the ACO pursuant to the terms of this Agreement; |
| 3. | The quality of the services performed under this Agreement; |
| 4. | The ACO’s right to, and distribution of, Shared Savings; and |
| 5. | The ability of the ACO to bear the risk of potential losses and to repay any losses to CMS. |
| B. | Maintenance of Records |
The ACO agrees, and must require all Next Generation Participants, Preferred Providers, and individuals and entities performing functions or services related to ACO Activities to agree, to the following:
| 51 |
| 1. | To maintain and give the Government, including CMS, HHS, and the Comptroller General or their designees, access to all books, contracts, records, documents, and other evidence (including data related to Medicare utilization and costs, quality performance measures, and other financial arrangements) sufficient to enable the audit, evaluation, inspection, or investigation of the following: the ACO’s compliance with the terms of this Agreement, including provisions that require the ACO impose duties or requirements on Next Generation Participants or Preferred Providers; whether Next Generation Participants or Preferred Providers complied with the duties and requirements imposed on them by the ACO pursuant to the terms of this Agreement; the quality of services furnished to Next Generation Beneficiaries; the ACO’s right to, and distribution of, Shared Savings; and the ACO’s obligation and ability to repay any Shared Losses or Other Monies Owed to CMS. |
| 2. | To maintain such books, contracts, records, documents, and other evidence for a period of 10 years from the expiration or termination of this Agreement or from the date of completion of any audit, evaluation, inspection, or investigation, whichever is later, unless: |
| (a) | CMS determines there is a special need to retain a particular record or group of records for a longer period and notifies the ACO at least 30 calendar days before the normal disposition date; or |
| (b) | There has been a termination, dispute, or allegation of fraud or similar fault against the ACO, its Next Generation Participants, Preferred Providers, or other individuals or entities performing functions or services related to ACO Activities, in which case the records shall be maintained for an additional six years from the date of any resulting final resolution of the termination, dispute, or allegation of fraud or similar fault. |
| XIX. | Remedial Action and Termination |
| A. | Remedial Action |
| 1. | If CMS determines that any provision of this Agreement may have been violated, CMS may take one or more of the following actions: |
| (a) | Notify the ACO and, if appropriate, the Next Generation Participant, and/or Preferred Provider of the violation; |
| (b) | Require the ACO to provide additional information to CMS or its designees; |
| (c) | Conduct on-site visits, interview Beneficiaries, or take other actions to gather information; |
| (d) | Place the ACO on a monitoring and/or auditing plan developed by CMS; |
| (e) | Require the ACO to remove a Next Generation Participant or Preferred Provider from the Participant List or Preferred Provider List and to terminate its agreement, immediately or within a timeframe specified by CMS, with such Next Generation Participant or Preferred Provider with respect to this Model; |
| (f) | Require the ACO to terminate its relationship with any other individual or entity performing functions or services related to ACO Activities; |
| 52 |
| (g) | Prohibit the ACO from distributing Shared Savings to a Next Generation Participant or Preferred Provider; |
| (h) | Request a corrective action plan (“CAP”) from the ACO that is acceptable to CMS, in which case, the following requirements apply: |
| i. | The ACO shall submit a CAP for CMS approval by a deadline established by CMS; and |
| ii. | The CAP must address what actions the ACO will take (or will require any Next Generation Participant, Preferred Provider or other individual or entity performing functions or services related to ACO Activities to take) within a specified time period to ensure that all deficiencies will be corrected and that the ACO will be in compliance with the terms of this Agreement; |
| (i) | Amend this Agreement without the consent of the ACO to provide that any or all waivers of existing law made pursuant to section 1115A(d)(1) of the Act will be inapplicable; |
| (j) | Amend this Agreement without the consent of the ACO to deny the use of any Alternative Payment Mechanism by the ACO or any Next Generation Participant and to require that the ACO terminate any agreements effectuating such Alternative Payment Mechanism by a date determined by CMS, in which case, the ACO (and any Next Generation Participant or Preferred Provider, if applicable) shall be paid under normal FFS following the effective date determined by CMS, and Other Monies Owed will be calculated and paid in accordance with Section XIV.C and Appendix B; |
| (k) | Discontinue the provision of data sharing and reports to the ACO under Section VI; |
| (l) | Amend this Agreement without the consent of the ACO to deny the use of one or more Benefit Enhancements by the ACO or any Next Generation Participant or Preferred Provider and to require that the ACO terminate any agreements effectuating such Benefit Enhancements by a date determined by CMS. |
| 2. | CMS may impose additional remedial actions or terminate this Agreement pursuant to Section XIX.B if CMS determines that remedial actions were insufficient to correct noncompliance with the terms of this Agreement. |
| 3. | CMS may require the ACO to remove a Next Generation Participant or Preferred Provider from the ACO’s Participant List or Preferred Provider List and terminate its written agreement with the removed Next Generation Participant or Preferred Provider if CMS determines that the Next Generation Participant or Preferred Provider: |
| (a) | Has failed to comply with any Medicare program requirement, rule, or regulation; |
| 53 |
| (b) | Has failed to comply with the ACO’s corrective action plan, the monitoring and/or auditing plan developed by CMS for the ACO, or other remedial action imposed by CMS; or |
| (c) | Has taken any action that threatens the health or safety of a Beneficiary or other patient. |
| B. | Termination of Agreement by CMS |
CMS may immediately or with advance notice terminate this Agreement if:
| 1. | CMS determines that the Agency no longer has the funds to support the Model; |
| 2. | CMS terminates the Model pursuant to Section 1115A(b)(3)(B) of the Act; |
| 3. | CMS determines that the ACO: |
| (a) | Has failed to comply with any term of this Agreement or any other Medicare program requirement, rule, or regulation; |
| (b) | Has failed to comply with a monitoring and/or auditing plan; |
| (c) | Has failed to submit, obtain approval for, implement or fully comply with the terms of a CAP; |
| (d) | Has failed to demonstrate improved performance following any remedial action; |
| (e) | Has taken any action that threatens the health or safety of a Beneficiary or other patient; |
| (f) | Has submitted false data or made false representations, warranties, or certifications in connection with any aspect of the Model; |
| (g) | Is subject to sanctions or other actions of an accrediting organization or a federal, state or local government agency; |
| (h) | Is subject to investigation or action by HHS (including HHS-OIG and CMS) or the Department of Justice due to an allegation of fraud or significant misconduct, including being subject to the filing of a complaint, filing of a criminal charge, being subject to an indictment, being named as a defendant in a False Claims Act qui tam matter in which the government has intervened, or similar action; or |
| (i) | Assigns or purports to assign any of the rights or obligations under this Agreement, voluntarily or involuntarily, whether by merger, consolidation, dissolution, operation of law, or any other manner, without the written consent of CMS. |
| 4. | CMS determines that one or more of the ACO’s Next Generation Participants or Preferred Providers has submitted false data or made false representations, warranties, or certifications in connection with any aspect of the Model; or |
| 5. | The state in which the ACO operates enters into an arrangement with CMS that is based on a statewide global or per-capita Medicare payment. |
| 54 |
| C. | Termination of Agreement by ACO |
The ACO may terminate this Agreement prior to the end of the Performance Year upon advance written notice to CMS. Such notice must specify the effective date of the termination, which date may be no sooner than 30 days following the date of the notice.
| D. | Financial Settlement upon Termination |
| 1. | If this Agreement is terminated by either party, except as otherwise provided in this section, CMS shall conduct settlement for the entire Performance Year in which the Agreement is terminated in accordance with Section XIV.C of this Agreement. |
| 2. | If this Agreement is terminated by CMS under Section XIX.B, CMS shall not make any payments of Shared Savings to the ACO, and the ACO shall remain liable for any Shared Losses, for the Performance Year in which termination becomes effective. |
| 3. | If the ACO voluntarily terminates this Agreement during a Performance Year pursuant to Section XIX.C.1 by providing notice to CMS on or before February 28, with an effective date 30 days after the date of notice, the ACO shall neither be eligible to receive Shared Savings nor liable for Shared Losses for such Performance Year. |
| 4. | Upon termination or expiration of this Agreement, the ACO shall immediately pay all Other Monies Owed to CMS and shall remain liable for any amounts included in a settlement report issued for any Performance Year in accordance with Section XIV.C.5. |
| E. | Notifications to Participants, Preferred Providers, and Beneficiaries upon Termination |
| 1. | If this Agreement is terminated under Sections XIX.B or XIX.C, the ACO shall provide written notice of the termination to all Next Generation Participants and Preferred Providers. The ACO shall also post a notice of the termination on its ACO website. The ACO shall deliver such written notice in a manner determined by CMS and no later than 30 days before the effective date of termination unless a later date is specified by CMS. The ACO shall include in such notices any content specified by CMS, including information regarding data destruction and the discontinuation of Benefit Enhancements, as applicable. |
| 2. | The ACO may also provide written notice of the termination to Next Generation Beneficiaries. If the ACO elects to send a notice of termination to Next Generation Beneficiaries, the ACO shall deliver such notices in a manner determined by CMS and no later than 30 days before the effective date of termination unless a later date is specified by CMS. The ACO shall include in such notices any content specified by CMS, including information regarding the discontinuation of Benefit Enhancements and the CCR, as applicable. Any notice to Next Generation Beneficiaries is subject to review and approval by CMS under Section V.E., as “Descriptive ACO Materials and Activities.” |
| 55 |
| XX. | Limitation on Review and Dispute Resolution |
| A. | Limitations on Review |
There is no administrative or judicial review under sections 1869 or 1878 of the Act or otherwise for the following:
| 1. | The selection of organizations, sites, or participants to test the selected models, including the decision by CMS to terminate this Agreement or to require the termination of any individual’s or entity’s status as a Next Generation Participant or Preferred Provider; |
| 2. | The elements, parameters, scope, and duration of such models for testing or dissemination; |
| 3. | Determinations regarding budget neutrality under subsection 1115A(b)(3); |
| 4. | The termination or modification of the design and implementation of a model under subsection 1115A(b)(3)(B); |
| 5. | Decisions about expansion of the duration and scope of a model under subsection 1115A(c), including the determination that a model is not expected to meet criteria described in paragraph (1) or (2) of such subsection; |
| 6. | The selection of quality performance standards; |
| 7. | The assessment of the quality of care furnished by the ACO; |
| 8. | The alignment of Beneficiaries to the ACO; and |
| 9. | A final settlement report issued pursuant to Section XIV.C, including without limitation the determination of— |
| (a) | the Historical Expenditure Baseline; |
| (b) | the Performance Year Benchmark; |
| (c) | the ACO Performance Year Expenditures; |
| (d) | the determination of whether the ACO is eligible for Shared Savings or liable for Shared Losses or Other Monies Owed; and |
| (e) | the amount of such Shared Savings, Shared Losses, and/or Other Monies Owed. |
| B. | Dispute Resolution |
| 1. | Right to Reconsideration |
The ACO may request reconsideration of a determination made by CMS pursuant to this Agreement only if such reconsideration is not precluded by Section 1115A(d)(2) of the Act or this Agreement.
| 56 |
| (a) | Such a request for reconsideration by the ACO must satisfy the following criteria: |
| i. | The request must be submitted to a designee of CMS (“reconsideration official”) who— |
| A. | Is authorized to receive such requests; and |
| B. | Did not participate in the determination that is the subject of the reconsideration request. |
| ii. | The request must contain a detailed, written explanation of the basis for the dispute, including supporting documentation. |
| iii. | The request must be made within 30 days of the date of the determination for which reconsideration is being requested via email to CMS at the address specified in Section XXI.A or such other address as may be specified by CMS. |
| (b) | Requests that do not meet the requirements of Section XX.B.1(a) will be denied by the reconsideration official. |
| (c) | Within 10 business days of receiving a request for reconsideration, the reconsideration official will send to the ACO and to CMS a written acknowledgement of receipt of the reconsideration request. Such an acknowledgement will set forth: |
| i. | The review procedures; and |
| ii. | A briefing schedule that permits each party to submit only one written brief, including any evidence, for consideration by the reconsideration official in support of the party’s position. The submission of any additional briefs or supplemental evidence will be at the sole discretion of the reconsideration official. |
| 2. | Standards for reconsideration. |
| (a) | The parties shall proceed diligently with the performance of this Agreement during the course of any dispute arising under the Agreement. |
| (b) | The reconsideration will consist of a review of documentation that is submitted timely and in accordance with the standards specified by the reconsideration official. |
| (c) | The burden of proof is on the ACO to demonstrate to the reconsideration official with clear and convincing evidence that the determination is inconsistent with the terms of the Agreement. |
| 3. | Reconsideration determination. |
| (a) | The reconsideration determination will be based only upon |
| i. | Position papers and supporting documentation that are timely submitted to the reconsideration official and meet the standards for submission; and |
| 57 |
| ii. | Documents and data that were timely submitted to CMS in the required format before the agency made the determination that is the subject of the reconsideration request. |
| (b) | The reconsideration official will issue to CMS and to the ACO a written notification of the reconsideration determination. Absent unusual circumstances, written notification will be issued within 60 days of receipt of timely filed position papers and supporting documentation. |
| (c) | Effect of the Reconsideration Determination |
| i. | The determination of the reconsideration official is final and binding. |
| ii. | The reconsideration review process under this Agreement shall not be construed to negate, diminish, or otherwise alter the applicability of existing laws, rules, and regulations or determinations made by other government agencies. |
| XXI. | Miscellaneous |
| A. | Agency Notifications and Submission of Reports |
Unless otherwise stated in writing after the Effective Date, all notifications and reports required under this Agreement shall be submitted to the parties at the addresses set forth below.
CMS: Next Generation ACO Model
Centers for Medicare & Medicaid Services
7500 Security Boulevard
Mailstop: WB-06-05
Baltimore, MD 21244
Email: NextGenerationACOModel@cms.hhs.gov
| ACO: | ||
| B. | Notice of Bankruptcy |
In the event the ACO enters into proceedings relating to bankruptcy, whether voluntary or involuntary, the ACO agrees to furnish, by certified mail, written notification of the bankruptcy to CMS. This notification shall be furnished within 5 calendar days of the initiation of the proceedings relating to bankruptcy filing. This notification shall include the date on which the bankruptcy petition was filed, the court in which the bankruptcy petition was filed, and a listing of Government contracts, project agreements, contract officers, and project officers for all Government contracts and project agreements against which final payment has not been made. This obligation remains in effect until the expiration or termination of this Agreement and final payment by the ACO under this Agreement has been made.
| 58 |
| C. | Severability |
In the event that any one or more of the provisions of this Agreement is, for any reason, held to be invalid, illegal or unenforceable in any respect, such invalidity, illegality or unenforceability shall not affect any other provisions of this Agreement, and this Agreement shall be construed as if such invalid, illegal or unenforceable provisions had never been included in the Agreement, unless the deletion of such provision or provisions would result in such a material change to the Agreement so as to cause continued participation under the terms of the Agreement to be unreasonable.
| D. | Entire Agreement; Amendment |
This Agreement, including all Appendices, constitutes the entire agreement between the parties. The parties may amend this Agreement or any Appendix hereto at any time by mutual written agreement; provided, however, that CMS may amend this Agreement or any Appendix hereto without the consent of the ACO as specified in this Agreement or Appendix, or for good cause or as necessary to comply with applicable federal or state law, regulatory requirements, accreditation standards or licensing guidelines or rules. To the extent practicable, CMS shall provide the ACO with 30 calendar days advance written notice of any such unilateral amendment, which notice shall specify the amendment’s effective date.
| E. | Survival |
Expiration or termination of this Agreement by any party shall not affect the rights and obligations of the parties accrued prior to the effective date of the expiration or termination of this Agreement, except as provided in this Agreement. The rights and duties under the following sections of this agreement shall also survive termination of this agreement and apply thereafter:
| 1. | Section XVIII (Audits and Record Retention); |
| 2. | Section VI.B (Data Sharing and Reports); |
| 3. | Section VIII.C. (Quality Measure Reporting); |
| 4. | Section XVII.C (Compliance and Oversight); |
| 5. | Section XV. A (Evaluation Requirement); |
| 6. | Section XIV. B (Alternative Payment Mechanisms) |
| 7. | Section XIV. C (Settlement); |
| 8. | Section XIV. D (Financial Guarantee); |
| 9. | Section XIX. D, E (Financial Settlement upon Termination; Notifications to Participants, Preferred Providers, and Beneficiaries upon Termination); |
| 59 |
| 10. | Section XXI. B (Notice of Bankruptcy); and |
| 11. | Appendix B (Next Generation ACO Alignment and Financial Reconciliation). |
Provisions of this Agreement that survive the expiration or termination of this Agreement, as specified in this Section E may be amended after the effective date of the expiration or termination of this Agreement with the mutual consent of the parties as necessary to achieve the purpose of the Next Generation ACO Model.
| F. | Precedence |
If any provision of this Agreement conflicts with a provision of any document incorporated herein by reference, the provision of this Agreement shall prevail.
| G. | Change of ACO Name |
If the ACO changes its name, the ACO shall forward to CMS a copy of the document effecting the name change, authenticated by the appropriate state official, and the parties shall execute an agreement reflecting the change of the ACO’s name.
| H. | Prohibition on Assignment |
Except with the prior written consent of CMS, the ACO shall not transfer, including by merger (whether the ACO is the surviving or disappearing entity), consolidation, dissolution, or otherwise: (1) any discretion granted it under this Agreement; (2) any right that it has to satisfy a condition under this Agreement; (3) any remedy that it has under this Agreement; or (4) any obligation imposed on it under this Agreement. The ACO shall provide CMS 90 days advance written notice of any such transfer. This obligation remains in effect until the expiration or termination of this Agreement and final payment by the ACO under this Agreement has been made. CMS may condition its consent to such transfer on full or partial reconciliation of Shared Losses and Other Monies Owed. Any purported transfer in violation of this Section is voidable at the discretion of CMS.
| I. | Change in Control |
CMS may terminate this Agreement or require immediate reconciliation of Shared Losses and Other Monies Owed if the ACO undergoes a Change in Control. For purposes of this paragraph, a “Change in Control” shall mean: (1) the acquisition by any “person” (as such term is used in Sections 13(d) and 14(d) of the Securities Exchange Act of 1934) of beneficial ownership (within the meaning of Rule 13d-3 promulgated under the Securities Exchange Act of 1934), directly or indirectly, of voting securities of the ACO representing more than 50% of the ACO’s outstanding voting securities or rights to acquire such securities; (2) upon any sale, lease, exchange or other transfer (in one transaction or a series of transactions) of all or substantially all of the assets of the ACO; or (3) a plan of liquidation of the ACO or an agreement for the sale or liquidation of the ACO is approved and completed. The ACO shall provide CMS 90 days advance written notice of a Change in Control. This obligation remains in effect until the expiration or termination of this Agreement and final payment by the ACO under this Agreement has been made.
| 60 |
| J. | Certification |
The ACO executive signing this Agreement certifies to the best of his or her knowledge, information, and belief that the information submitted to CMS and contained in this Agreement (inclusive of Appendices), is accurate, complete, and truthful, and that he or she is authorized by the ACO to execute this Agreement and to legally bind the ACO on whose behalf he or she is executing this Agreement to its terms and conditions.
| K. | Execution in Counterpart |
This Agreement and any amendments hereto may be executed in counterparts, each of which shall be deemed to be an original, but all of which, taken together, shall constitute one and the same agreement. In the event that any signature is delivered by facsimile transmission or by e-mail delivery of a “.pdf” format data file, such signature shall create a valid and binding obligation of the party executing (or on whose behalf such signature is executed) with the same force and effect as if such facsimile or “.pdf” signature page were an original thereof.
[SIGNATURE PAGE FOLLOWS]
| 61 |
Each party is signing this Agreement on the date stated opposite that party’s signature. If a party signs but fails to date a signature, the date that the other party receives the signing party’s signature will be deemed to be the date that the signing party signed this Agreement.
| ACO: | ||||
| Date: | By: | |||
| Name of authorized signatory | ||||
| Title | ||||
CMS:
| Date: | By: | |||
| Name of authorized signatory | ||||
| Title | ||||
Appendices
| A. | Non-Duplication Waiver and Participant Exclusivity |
| B. | Next Generation ACO Alignment and Financial Reconciliation |
| C. | Voluntary Alignment |
| D. | HIPAA-Covered Disclosure Request Attestation and Data Specification Worksheet |
| E. | [RESERVED] |
| F. | Quality Measures |
| G. | Alternative Payment Mechanism - Infrastructure Payments |
| H. | Alternative Payment Mechanism - Population-Based Payment |
| I. | Benefit Enhancement - 3-Day SNF Rule Waiver |
| J. | Benefit Enhancement - Telehealth Expansion |
| K. | Benefit Enhancement - Post-Discharge Home Visits |
| L. | Financial Guarantees - Requirements and Guidance |
| M. | ACO Proprietary Information |
| N. | Alternative Payment Mechanism – All-Inclusive Population-Based Payment |
| 62 |
Next Generation ACO Model
Appendix A
Non-Duplication Waiver and Participant Overlap
| I. | Waiver |
In order to support the ACO’s ability to enter into agreements with Medicare-enrolled providers and suppliers to participate as Preferred Providers, and thus enable the ACO to better care for its Next Generation Beneficiaries in an environment where increasing numbers of providers and suppliers are participating in ACOs under the Medicare Shared Savings Program and in other Medicare shared savings initiatives, CMS waives the non-duplication requirements under section 1899(b)(4)(A) of the Act and 42 C.F.R. § 425.114(a) as they apply to Preferred Providers, subject to the requirements set forth in this Appendix A.
| II. | ACO Overlap |
| A. | The ACO may not simultaneously participate in any other Medicare shared savings initiatives (e.g., MSSP, Pioneer ACO Model, Comprehensive ESRD Care (CEC) Initiative). |
| B. | If the ACO is otherwise eligible, the ACO may participate in other Medicare demonstrations or models. CMS may issue guidance or work directly with the ACO in determining how participation in certain demonstrations or models can be combined with participation in the Next Generation ACO Model. |
| III. | Next Generation Participant and Preferred Provider Overlap |
| A. | Pursuant to section 1899(b)(4)(A), a Next Generation Participant may not also be an ACO participant, ACO provider/supplier and/or ACO professional in an accountable care organization in the MSSP. |
| B. | A Next Generation Professional who is a primary care specialist as defined in Appendix B may not: (a) be identified as a Next Generation Participant by a different accountable care organization in the Model; (b) be an ACO participant, ACO provider/supplier or ACO professional in the Medicare Shared Savings Program; or (c) participate in another Medicare ACO model, except as expressly permitted by CMS. |
| C. | A Next Generation Participant who is a non-primary care specialist according to Appendix B of this Agreement may be a Next Generation Participant in another accountable care organization in this Model, a Pioneer Provider/Supplier in the Pioneer ACO Model, or serve in an equivalent role in or any other model or program in which such non-primary care specialists are not required to be exclusive to one participating entity. |
| 1 |
| D. | A Preferred Provider may serve in the following roles provided all other applicable requirements are met: |
| 1. | Preferred Provider for one or more other accountable care organizations participating in the Next Generation ACO Model; |
| 2. | Subject to Section III.B of this Appendix, Next Generation Participant in one or more other accountable care organizations participating in the Next Generation ACO Model; |
| 3. | Pursuant to the waiver in Section I of this Appendix, ACO participant, ACO provider/supplier and/or ACO professional in an accountable care organization in the MSSP; and/or |
| 4. | Role similar in function to the Next Generation Participant in another shared savings initiative. |
| 2 |
Next Generation ACO Model
Benchmarking Methods
Performance Years 1 through 3
October 1, 2016
Revision: 1.02.01
Document Number: RTI.NGACO.BNCH.1.02.01
Contact Number: HHSM-500-2014-0037I/HHSM-500-T0001
Prepared for:
Centers for Medicare & Medicaid Services (CMS)
Center for Medicare & Medicaid Innovation
Seamless Care Models Group
7500 Security Boulevard, N2-13-16
Baltimore, MD 21244-1850
Prepared by:
RTI International
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Front Matter | ii |
Revision History
| Revision | Date | Revisions | ||
| 1.00 | November 17, 2015 | Final post-OGC review version | ||
| 1.00.01 | November 19, 2015 | Revised §3.7.5 Revision to §5.3 Revision to §8.1 |
||
| 1.00.02 | November 19, 2015 | Revision to §3.7.1 Revision to §3.7.5 Revision to §3.7.9 |
||
| 1.00.03 | December 14, 2015 |
Non-substantive copy editing corrections to §§2.0, 2.2, 2.4, 2.4.1, 2.4.2, 3.3, 3.4, 3.7.5, 4.0, 5.2, 5.3, 6.1, 6.2, 6.3, 6.4, 7.0, 7.1.1, 7.1.2, 7.2, 7.3, 8.0, 8.1, A.1, A.2.6, A.2.7, A.5. Deleted footnote in §5.4.1. |
||
| 1.02.01 | October 1, 2016 |
Addition of §3.7.6 Revision of §§2.4, 2.7, 3.9, 7.0, 7.1, 8.1, A.2.4, A.2.6, A.4, A.6 |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Front Matter | iii |
Reference documents
| Document | Date | Title | ||
| 00/00/0000 |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Front Matter | iv |
Acronyms
| ACO | Accountable Care Organization |
| CMMI | Center for Medicare & Medicaid Innovation |
| CMS | Centers for Medicare & Medicaid Services |
| NGACO | Next Generation ACO |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Front Matter | v |
Table of Contents
| Revision History | ii | |
| Reference documents | iii | |
| Acronyms | iv | |
| Table of Contents | v | |
| 1.0 | Introduction | 1 |
| 2.0 | Overview of the Next Generation ACO Model Benchmark | 1 |
| 2.1 | NGACO baseline expenditure | 2 |
| 2.2 | Projected regional trend | 2 |
| 2.3 | Risk adjustment | 3 |
| 2.4 | Efficiency- and quality-adjusted discount | 3 |
| 2.4.1 | Quality adjustment to the standard discount | 3 |
| 2.4.2 | Efficiency adjustments to standard discount | 4 |
| 2.7 | Illustrative Example of Benchmark Calculation | 4 |
| 3.0 | Definitions | 4 |
| 3.1 | Base and performance years | 5 |
| 3.2 | Entitlement categories | 5 |
| 3.3 | NGACO region | 5 |
| 3.4 | Alignment-eligible beneficiaries | 5 |
| 3.5 | Aligned beneficiaries | 6 |
| 3.6 | Reference beneficiaries | 7 |
| 3.7 | Expenditure | 7 |
| 3.7.1 | Exclusion of certain provider payments | 7 |
| 3.7.2 | Indirect Medicare Education and Disproportionate Share Hospital payments | 8 |
| 3.7.3 | Budget sequestration | 8 |
| 3.7.4 | Effect of Population-based Payment (PBP) | 8 |
| 3.7.5 | Adjustment for performance-based provider payment incentives | 8 |
| 3.7.6. | Bundled Payments for Care Improvement initiative | 8 |
| 3.8 | Capped expenditure | 9 |
| 3.9 | Provider payments made outside of standard claims systems | 9 |
| 3.10 | Quality Measures | 9 |
| 4.0 | NGACO benchmark for each entitlement category | 9 |
| 5.0 | Trended baseline | 10 |
| 5.1 | NGACO baseline expenditure | 10 |
| 5.2 | Projected regional trend | 10 |
| 5.3 | Projected national FFS trend | 10 |
| 5.4 | GAF trend adjustment | 11 |
| 5.4.1 | Calculation of GAF trend adjustment factors | 12 |
| 5.4.2 | GAF trend-adjusted baseline claims | 12 |
| 6.0 | Risk Adjustment of Trended Baseline | 13 |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Front Matter | vi |
| 6.1 | Risk scores | 13 |
| 6.2 | “Re-normalization” of Risk Scores | 13 |
| 6.3 | Risk ratio | 14 |
| 6.4 | Risk-adjusted trended baseline | 15 |
| 7.0 | Quality- and efficiency-adjusted discount | 15 |
| 7.1 | Quality adjustment to the standard discount | 16 |
| 7.1.1 | Use of prior year quality score for the initial benchmark calculation | 16 |
| 7.1.2 | Use of performance-year quality score for purposes of financial settlement | 17 |
| 7.1.3 | Minimum Quality Requirement | 17 |
| 7.2 | Regional Baseline Efficiency Adjustment to the standard discount | 17 |
| 7.2.1 | Regional baseline efficiency ratio | 18 |
| 7.2.2 | GAF baseline standardization factors | 18 |
| 7.2.3 | GAF-adjusted baseline claims | 19 |
| 7.2.4 | Risk- and GAF-adjusted expenditure PBPM for each county | 19 |
| 7.2.5 | Regional Efficiency Adjustment | 20 |
| 7.3 | National Baseline Efficiency Adjustment to the Savings Requirement | 21 |
| 7.3.1 | National Efficiency Ratio | 21 |
| 7.3.2 | National Efficiency Adjustment | 22 |
| 8.0 | NGACO Financial Settlement | 22 |
| 8.1 | Savings/Losses Amount | 23 |
| 8.2 | Alternative payment arrangements | 24 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 25 | |
| A.1 | Alignment Years | 25 |
| A.2 | Definitions used in alignment procedures | 25 |
| A.2.1 | Alignment-eligible beneficiary | 25 |
| A.2.2 | “Alignable” beneficiary | 25 |
| A.2.3 | NGACO Service Area | 26 |
| A.2.4 | Qualified Evaluation & Management services | 26 |
| A.2.5 | Primary care services | 26 |
| A.2.6 | Primary care specialists | 26 |
| A.2.7 | Next Generation Participant | 27 |
| A.2.8 | Participating practice | 27 |
| A.2.9 | Participating practitioner (professional) | 27 |
| A.2.10 | Legacy practice identifiers | 28 |
| A.3 | Quarterly exclusion of beneficiaries during the Performance Year | 28 |
| A.4 | Alignment of beneficiaries | 28 |
| A.5 | Use of weighted allowable charges in alignment | 29 |
| A.6 | The 2-stage alignment algorithm | 29 |
| A.7 | Tie-breaker rule | 30 |
| A.8 | Voluntary alignment | 30 |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Front Matter | vii |
| Appendix B. Formal statement of Next Generation ACO Model benchmarking methods | 39 | |
| B.1 | Notational conventions | 39 |
| B.2 | NGACO savings or loss | 39 |
| B.3 | Benchmark expenditure | 40 |
| B.4 | Benchmark PBPM for an entitlement category | 40 |
| B.5 | Baseline expenditure PBPM for an entitlement category | 41 |
| B.6 | Capped expenditure accrued to an entitlement category by a beneficiary | 41 |
| B.6.1 | Capped base-year expenditure | 41 |
| B.6.1 | Capped Performance-Year expenditure | 42 |
| B.7 | Regional GAF trend adjustment for an entitlement category | 42 |
| B.8 | Risk adjustment to the trended baseline | 43 |
| B.8.1 | Re-normalized base year average risk score for an entitlement category | 43 |
| B.8.2 | Re-normalized Performance-Year average risk score for an entitlement category | 45 |
| B.9 | Adjusted discount | 47 |
| B.9.1 | Regional efficiency adjustment to the standard discount | 48 |
| B.9.2 | National efficiency adjustment to the standard discount | 48 |
| B.9.3 | Quality adjustment to the standard discount | 49 |
| B.10 | Standardized baseline expenditure PBPM for an entitlement category | 49 |
| B.10.1 | Standardized NGACO baseline expenditure PBPM for an entitlement category | 49 |
| B.10.2 | Standardized regional baseline expenditure PBPM for an entitlement category | 50 |
| B.10.3 | Standardized national baseline expenditure PBPM for an entitlement category | 50 |
| B.11 | Base-year average operating expense PBPM | 51 |
| B.11.1 | Operating expenditure incurred by a beneficiary | 51 |
| B.11.2 | Capped base-year operating expenditure for a beneficiary | 52 |
| B.12 | Terms used in the formal statement of the NGACO benchmarking methods | 52 |
| Appendix C. Technical description of the GAF trend adjustment | 57 | |
| C.1 | Overview of the GAF trend adjustment | 57 |
| C.1.1 | GAF-adjustable claims | 58 |
| C.1.2 | Attribution of expenditures to counties | 58 |
| C.2 | Regional GAF trend adjustment factor for an NGACO | 58 |
| C.3 | County-level GAF trend adjustment factor | 59 |
| C.3.1 | Formal statement of county-level GAF trend-adjustment factor | 60 |
| C.3.2 | Budget-neutrality factor for class of GAF-adjustable claims | 61 |
| C.3.3 | County-level GAF trend-adjusted base-year expenditure (before budget neutrality) | 62 |
| C.3.4 | Beneficiary-level GAF trend-adjusted base-year expenditure | 63 |
| C.3.5 | GAF trend-adjusted base-year payment amount (expenditure) | 63 |
| C.4 | Adjustment of Inpatient Prospective Payment System (IPPS) claims | 64 |
| C.5 | Adjustment of Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS) claims | 65 |
| C.6 | Adjustment of Long-term Care Hospital Prospective Payment System (LTCH PPS) claims | 66 |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Front Matter | viii |
| C.7 | Adjustment of Skilled Nursing Facility Prospective Payment System (SNF PPS) claims | 67 |
| C.8 | Adjustment of Home Health Prospective Payment System (HH PPS) claims | 69 |
| C.9 | Adjustment of Hospice Per-diem Payment System (Hospice PDPS) claims | 70 |
| C.10 | Adjustment of Hospital Outpatient Prospective Payment System (OPPS) claims | 71 |
| C.11 | Adjustment of ESRD Prospective Payment System (ESRD PPS) claims | 72 |
| C.12 | Adjustment of Physician Fee Schedule (PFS) claims | 72 |
| Technical Note C-1: | 73 | |
| Appendix D. Technical description of the GAF baseline-adjustment | 76 | |
| D.1 | Overview of the GAF baseline-adjustment | 76 |
| D.1.1 | GAF-adjustable claims | 77 |
| D.1.2 | Attribution of expenditures to counties | 77 |
| D.2 | GAF baseline-adjustment factor for an NGACO | 77 |
| D.3 | County-level GAF trend adjustment factor | 78 |
| D.3.1 | Formal statement of county-level GAF baseline-adjustment factor | 79 |
| D.3.2 | Budget-neutrality factor for class of GAF-adjustable claims | 80 |
| D.3.3 | County-level GAF trend-adjusted base-year expenditure (before budget neutrality) | 81 |
| D.3.4 | Beneficiary-level GAF trend-adjusted base-year expenditure | 82 |
| D.3.5 | GAF trend-adjusted base-year payment amount (expenditure) | 82 |
| D.4 | Adjustment of Inpatient Prospective Payment System (IPPS) claims | 83 |
| D.5 | Adjustment of Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS) claims | 84 |
| D.6 | Adjustment of Long-term Care Hospital Prospective Payment System (LTCH PPS) claims | 85 |
| D.7 | Adjustment of Skilled Nursing Facility Prospective Payment System (SNF PPS) claims | 86 |
| D.8 | Adjustment of Home Health Prospective Payment System (HH PPS) claims | 87 |
| D.9 | Adjustment of Hospice Per-diem Payment System (Hospice PDPS) claims | 88 |
| D.10 | Adjustment of Hospital Outpatient Prospective Payment System (OPPS) claims | 89 |
| D.11 | Adjustment of ESRD Prospective Payment System (ESRD PPS) claims | 90 |
| D.12 | Adjustment of Physician Fee Schedule (PFS) claims | 90 |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 1.0 | Introduction | 1 |
| 1.0 | Introduction |
Building upon experience from the Pioneer ACO Model and the Medicare Shared Savings Program (MSSP), the Next Generation ACO (NGACO) Model offers a new opportunity in accountable care—one that sets predictable financial targets, enables providers and beneficiaries greater opportunities to coordinate care, and aims to attain the highest quality standards of care. The purpose of the NGACO Model is to test whether strong financial incentives for ACOs, coupled with tools to support better patient engagement and care management, can improve health outcomes and reduce expenditures for Medicare fee-for-service (FFS) beneficiaries.
The Model offers financial arrangements with higher levels of risk and reward than current Medicare ACO initiatives, using benchmarking methods that: (1) reward quality performance; (2) reward both attainment of and improvement in cost containment; and (3) ultimately transition away from reference to ACO historical expenditures. The Model offers a choice of two risk arrangements that determine the portion of the savings or losses that accrue to the ACO. The risk arrangement applies to the difference between actual expenditures and the prospective benchmark.
This document describes the NGACO Model’s benchmarking methodology. Section 2 is an overview of the methodology, and Section 3 provides definitions of key concepts. Each of the major components of the methodology is then described in greater detail in Sections 4 to 10.
| 2.0 | Overview of the Next Generation ACO Model Benchmark |
This Section provides an overview of the Performance Year Benchmark (or, for purposes of this methodology paper, “Benchmark”). This prospective benchmark is a core feature of the NGACO Model. The Performance Year Benchmark used in the NGACO Model is prospective because the trend that is used to project the ACO’s baseline expenditure is set prior to the start of the Performance Year.1
The Performance Year Benchmark will be set initially using the expenditure, risk score, and quality data that are available at the time the Performance-Year trended baseline is calculated. The Benchmark will be updated at the time of financial reconciliation using the average Performance-Year risk scores of Next Generation Beneficiaries aligned to the NGACO for the Performance-Year and the quality score for the Performance-Year. Neither the baseline expenditure data nor the projected regional trend will be updated after the calculation of the Benchmark, except as allowed under the terms of the Participation Agreement between the NGACO and CMS.
1 The Next Generation ACO benchmark is prospective in the same way that a Medicare Advantage plan’s negotiated rate is prospective. The base payment rate of a Medicare Advantage plan is determined through the prospective bidding process. However, the PBPM payment that the Medicare Advantage plan receives depends on the risk scores of enrolled beneficiaries, and the number of months that are paid under the Aged/Disabled and ESRD payment rates, neither of which is known definitively until after the end of the fiscal year. For example, the CY2016 revenue under the negotiated rates will not be known until mid-2017 when the final risk-score data for CY2016 enrollees is available.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 2.1 | Overview of the Next Generation ACO Model Benchmark | 2 |
In the first three Performance Years (calendar years 2016-2018), the Performance Year Benchmark will be calculated in four steps:
| 1. | Step 1: Calculate the NGACO baseline expenditure for the entitlement category; |
| 2. | Step 2: Calculate the trended baseline by applying a projected regional trend component; |
| 3. | Step 3: Calculate the risk-adjusted trended baseline by applying a risk adjustment factor reflecting the difference between the average risk of the base-year aligned beneficiaries and the average risk of the performance-year aligned beneficiaries; and, |
| 4. | Step 4: Calculate the Benchmark by applying a quality- and efficiency-adjusted discount to the risk-adjusted trended baseline. |
This document describes the NGACO benchmarking methodology. Section 2 is an overview of the methodology, section 3 defines key terms, and sections 4 through 10 describe in greater detail the calculation of the NGACO baseline, the trended baseline, risk adjustment, and the adjustments to the baseline that are made to arrive at the Benchmark.
| 2.1 | NGACO baseline expenditure |
The NGACO baseline expenditure is the expenditure incurred in a single baseline year (CY2014) by base- year (CY2014) aligned beneficiaries. The baseline expenditure will be calculated prior to the start of each performance year. CY2014 is the baseline year for the first three performance years. The baseline expenditure will be updated each year to reflect the ACO’s Participant List for the given Performance Year.2
| 2.2 | Projected regional trend |
The NGACO baseline expenditure will be trended to each Performance Year. The expenditure Benchmark will incorporate a projected regional trend, which will be:
| 1. | A national projected expenditure trend; |
| 2. | Adjusted to reflect the impact of Performance-Year Medicare geographic pricing factors on base-year expenditures. |
The national projected trend will be developed using a method similar to that used by the Medicare Office of the Actuary to develop the Medicare Advantage county rate book. Under limited circumstances, CMS would adjust the projected trend in response to unforeseeable events such as legislative actions that have a substantial impact on Medicare FFS expenditures.
2 If the NGACO’s Participant List is the same in all three Performance-Years, the NGACO baseline will be the same in all three Performance-Years. If an NGACO modifies its Participant List, the NGACO baseline expenditure will change because a different set of beneficiaries will be aligned in the base-year (CY2014).
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 2.0 | Overview of the Next Generation ACO Model Benchmark | 3 |
| 2.3 | Risk adjustment |
To calculate the Performance Year Benchmark, the trended baseline expenditure will be risk adjusted to account for the difference in the risk (or expected cost) of the beneficiaries aligned with the NGACO in the base year and the Next Generation Beneficiaries aligned with the NGACO in the Performance Year.
This adjustment will be based on the difference in the average Medicare Hierarchical Condition Categories (HCC) risk scores of the base-year and Performance-Year aligned beneficiaries. The HCC risk score (using both demographic and diagnostic components) will be used for all aligned beneficiaries.
The risk-adjustment to the ACO’s trended baseline will limited to a maximum of ±3%. Financial settlement will be based on the Performance-Year risk scores of the Next Generation Beneficiaries aligned to the ACO during the Performance Year 3
| 2.4 | Efficiency- and quality-adjusted discount |
The Performance Year Benchmark will be calculated by applying to the risk-adjusted trended baseline an efficiency- and quality-adjusted discount that will range from 0.5% to 4.5%. The adjusted discount is:
| 1. | A standard discount of 2.25%. |
| 2. | MINUS: A regional efficiency adjustment of ±1.0% |
| 3. | MINUS: A national efficiency adjustment of ±0.5% |
| 4. | MINUS: A quality adjustment to the standard discount of up to +1.0% |
The minimum adjusted discount is, therefore, 0.5% and the maximum is 4.5% as shown in section 7.0.2.4.1.
| 2.4.1 | Quality adjustment to the standard discount |
The standard discount will be reduced by up to 1% depending on the quality score attained by the NGACO in the Performance-Year. The quality adjustment to the standard discount in PY1/CY2016 for an NGACO whose agreement is effective January 1, 2016, will be 100% if the NGACO submits all data required to calculate a quality score in PY1 as described in the Participation Agreement. The quality adjustment to the standard discount in PY2/CY2017 for an NGACO whose agreement is effective January 1, 2017, will be 100% if the NGACO submits all data required to calculate a quality score in PY2.
The Performance-Year quality score for an ACO that does not report all data required to calculate the Performance-Year quality score or that does not otherwise satisfy quality scoring standards will be zero (0.00%). An ACO that has a quality score of zero will not be eligible to receive any savings bonus, but will be required to repay losses.
3 CMMI will endeavor to make use of preliminary or mid-year risk scores for the Performance-Year aligned beneficiaries, when they become available, in quarterly financial reports.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 3.0 | Definitions | 4 |
| 2.4.2 | Efficiency adjustments to standard discount |
The standard discount will be decreased or increased based on an ACO’s efficiency in the base-year relative to its region and to the nation as a whole.
| 1. | The regional efficiency adjustment to the standard discount will be ±1%. |
| 2. | The national efficiency adjustment to the standard discount will be ±0.5%. |
The efficiency adjustments will be set prospectively on the basis of base-year (CY2014) experience.
| 2.7 | Illustrative Example of Benchmark Calculation |
Table 2.7 illustrates the benchmark calculation.
Table 2.7. Calculation of Performance Year Benchmark for Aged/Disabled beneficiaries
|
Baseline (CY2014) |
Benchmark |
|||||||
| ACO baseline (CY2014) expenditure: | $ | 876.54 | $ | 876.54 | ||||
| Projected PY1/CY2016 regional trend adjustment: | $ | 30.36 | ||||||
| Projected PY1/CY2016 national trend: | 3.00 | % | ||||||
| CY2016 GAF trend adjustment | 0.45 | % | ||||||
| Projected PY1/CY2016 regional trend: | 3.46 | % | ||||||
| Trended baseline1 | $ | 906.90 | ||||||
| PY1 baseline risk adjustment factor2 | 1.010 | |||||||
| Risk-adjusted trended baseline3 | $ | 915.97 | ||||||
| Adjusted NGACO discount | ||||||||
| Standard discount | 2.25 | % | 2.25 | % | ||||
| National baseline efficiency adjustment to the standard discount | -0.04 | % | -0.04 | % | ||||
| National efficiency ratio | 0.993 | |||||||
| Regional baseline efficiency adjustment to the standard discount | -0.13 | % | -0.13 | % | ||||
| Regional efficiency ratio | 0.987 | |||||||
| Quality adjustment to the standard discount | -1.00 | % | ||||||
| Quality- and efficiency-adjusted discount | 1.08 | % | ||||||
| LESS: NGACO discount4 | $ | 9.89 | ||||||
| Benchmark5 | $ | 906.08 | ||||||
| 1 | The ACO baseline plus the regional trend adjustment (906.90 = 876.54 + 30.36 = 876.54 x (1 + 0.0346). |
| 2 | The ratio of the PY1 risk score to the base-year risk score (subject to a ±3% limit). The example assumes the PY1 risk score is 1% higher than the base-year risk score, therefore a risk adjustment factor of 1.010. |
| 3 | The product of the trended baseline and the risk adjustment factor (915.97 = 906.90 x 1.010). |
| 4 | The NGACO discount is equal to the risk-adjusted trended baseline multiplied by quality- and efficiency-adjusted discount ($899.12 = 0.0184 x $915.97). |
| 5 | The benchmark is equal to the risk-adjusted trended baseline less the NGACO discount ($899.12 = $915.97 – $16.85). |
| 3.0 | Definitions |
This section defines certain terms that are used throughout this document unless otherwise noted.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 3.0 | Definitions | 5 |
| 3.1 | Base and performance years |
Performance Year 1 (PY1) is calendar year 2016 (CY2016).
Performance Year 2 (PY2) is calendar year 2017 (CY2017).
Performance Year 3 (PY3) is calendar year 2018 (CY2018).
The base year (BY) for the first three performance years is calendar year 2014 (CY2014).
| 3.2 | Entitlement categories |
NGACO baseline and benchmark calculations are performed separately for:
| 1. | Aged and Disabled (A/D) aligned beneficiaries (aligned beneficiaries eligible for Medicare by age or disability) who do not have End Stage Renal Disease (ESRD). |
| 2. | End stage renal disease (ESRD) aligned beneficiaries (aligned beneficiaries eligible for Medicare by ESRD). 4 |
Each month of experience accrued during a year by an aligned beneficiary will be attributed to either the A/D or ESRD entitlement category.
| 3.3 | NGACO region |
The ACO’s region consists of all counties in which its base-year aligned beneficiaries reside. The ACO region is used in two components of the benchmark calculation:
| 1. | The calculation of the regional trend; and, |
| 2. | The calculation of the regional efficiency adjustment to the standard discount. |
For these components of the benchmark calculation, a person-month weighted average of county- specific values (i.e., the regional trend and the standardized regional baseline expenditure) will be calculated.
| 3.4 | Alignment-eligible beneficiaries |
A beneficiary is alignment-eligible during the base- or Performance-Year if the beneficiary:
4 ESRD status in a month is determined based on Medicare enrollment/eligibility files not dialysis claims. A beneficiary’s experience accrues to the ESRD entitlement category if, during a month, the beneficiary was receiving maintenance dialysis for kidney failure or was in the 3-month period starting in the month when a kidney transplant was performed.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 3.1 | Definitions | 6 |
| 1. | Is covered under Part A in January of the base- or performance-year and in every month of the base- or performance-year in which the beneficiary is alive; |
| 2. | Has no months of coverage under only Part A; |
| 3. | Has no months of coverage under only Part B; |
| 4. | Has no months of coverage under a Medicare Advantage or other Medicare managed care plan; |
| 5. | Has no months in which Medicare was the secondary payer; and, |
| 6. | Was a resident of the United States. |
Alignment is performed prior to the start of the Performance-Year, and alignment-eligibility will be determined on a quarterly basis throughout the Performance-Year.
Note that a beneficiary may be alignment-eligible in the base-year but not a Performance-Year and may be alignment-eligible in a Performance-Year but not the base-year.
| 3.5 | Aligned beneficiaries |
Prior to the start of the Performance Year, the Next Generation Beneficiaries for the Performance Year will be identified using the Participant List for that Performance Year.5 The same methods and Participant List will be used to identify two panels of aligned beneficiaries:
| 1. | Those beneficiaries aligned with the NGACO in the base-year; and, |
| 2. | Those beneficiaries aligned with the NGACO in the Performance -Year. |
To be included in the financial settlement, beneficiaries must be alignment-eligible during the Performance Year. A beneficiary who is not alignment-eligible in one or more months of the Performance-Year will be excluded from the aligned population of the ACO retroactive to the start of the Performance-Year.
Prior to financial settlement, Next Generation Beneficiaries will also be excluded if:
| 1. | The Next Generation Beneficiary was a resident of a county that was part of the ACO’s service area in the last month of the 2-year alignment period but was a resident of a county that was not part of the ACO’s service area in the performance-year. |
| 2. | During the base- or Performance-Year (respectively, for base-year and performance-year aligned beneficiaries) at least 50% of Qualified Evaluation and Management (QEM) services used by the Next Generation Beneficiary were from providers practicing outside the ACO’s service area. |
The same requirements apply to the base year. However, all alignment-eligibility requirements can be applied to beneficiaries aligned in the base-year at the time alignment is performed.
5 Alignment methods are described in Appendix A.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 3.0 | Definitions | 7 |
| 3.6 | Reference beneficiaries |
The reference beneficiaries, or population, for the base-year or Performance-Year will consist of all beneficiaries who are alignment-eligible in the base-year or Performance-Year.
| 3.7 | Expenditure |
Subject to the exceptions discussed below, the expenditure incurred by an alignment-eligible beneficiary, for purposes of financial calculations for any Performance Year or baseline period, is the sum of all Medicare payments on claims for services covered by Part A or Part B of Medicare. All services covered by Part A or Part B are used in financial calculations, including, but not limited to:
| 1. | Inpatient claims; |
| 2. | Skilled Nursing Facility (SNF) claims; |
| 3. | Home Health Agency (HHA) claims; |
| 4. | Hospice claims. |
| 5. | Physician claims: |
| 6. | Outpatient claims; and, |
| 7. | Durable Medical Equipment (DME) claims. |
The expenditure used in financial calculations is the total amount paid to providers on claims:
| 1. | For services covered by Medicare Parts A and B; |
| 2. | That are incurred during the base- or Performance-Year; and |
| 3. | That are paid within 3 months of the close of the base- or Performance-Year. |
The incurred date for a claim is determined by the date of service. The date of service is the “through date” of the period covered by the claim. In the case of claims for inpatient, outpatient, SNF, HHA and hospice claims, the “date of service” is the through date on the Part A claim header record. In the case of hospital physician, and DME claims, the date of service is the through date on the line item claim record.
The paid date for a claim is the effective date of the claim in conjunction with the date the claim is loaded into the Integrated Data Repository (IDR).
| 3.7.1 | Exclusion of certain provider payments |
Medicare inpatient pass-through payment amounts (estimates) for inpatient services are excluded from expenditures.
Direct Graduate Medical Education, PQRS, eRx, and EHR incentive payments for eligible professionals, and EHR incentive payments to hospitals that are not reflected in provider payments under the FFS payment systems are excluded from expenditure calculations.
Uncompensated Care (UCC) payments are excluded from the baseline and performance-year expenditure of beneficiaries.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 3.0 | Definitions | 8 |
| 3.7.2 | Indirect Medicare Education and Disproportionate Share Hospital payments |
Indirect Medical Education (IME) and Disproportionate Share Hospital (DSH) payments are included in calculation of the baseline and Performance-Year expenditure, but are excluded from the expenditure used in the calculation of the regional and national efficiency adjustments.6
| 3.7.3 | Budget sequestration |
All financial calculations will be based on the amount of payment that would have been made to providers if sequestration had not been required (i.e., on a pre-sequestration basis).
| 3.7.4 | Effect of Population-based Payment (PBP) |
Under the NGACO Model, an ACO can elect to participate in Population-Based Payments, under which certain Next Generation Participants may agree to receive Population Based Payment Fee Reductions, which will reduce their FFS payment reimbursements from CMS. These reductions in FFS payments will not be included in the calculation of the base-year or Performance-Year expenditure of the ACO (i.e., the baseline and Performance-Year expenditure will be the amount that would have been paid to the Next Generation Participant if the Population-Based Payment Fee Reductions had not been made).
| 3.7.5 | Adjustment for performance-based provider payment incentives |
By November 2016, CMS will determine whether and how to adjust the NGACO Benchmark and Performance-Year expenditure so that performance-based provider payment incentives (including but not limited to value-based purchasing, physician payment value modifiers, PQRS, and incentives to promote meaningful use of electronic health records) do not under- or over-state savings or losses.
If determined to be necessary, the NGACO Benchmark and Performance-Year expenditure will be adjusted not earlier than Performance-Year 2 (CY2017), and quarterly financial reporting will identify these adjustments.
| 3.7.6. | Bundled Payments for Care Improvement Initiative |
When determining the expenditures incurred by NGACO-aligned beneficiaries for purposes of financial reconciliation for a performance year, CMS will exclude Bundled Payments for Care Improvement (BPCI) initiative Net Payment Reconciliation Amounts only in those cases where including these BPCI Net Payment Reconciliation Amounts would be the sole reason that an ACO would incur shared losses or not qualify to receive shared savings. Consistent with Section 3.9 of this Appendix, in all other cases, the BPCI Net Reconciliation Amounts will be included in the determination of expenditures incurred by NGACO-aligned beneficiaries.
6 IME and DSH payments are excluded from the expenditure used to calculate the efficiency ratios because they are unrelated to an ACO’s efficiency.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 4.0 | NGACO benchmark for each entitlement category | 9 |
| 3.8 | Capped expenditure |
The capped expenditure for a base-year or Performance-Year that accrues to the entitlement category by the beneficiary is the lesser of:
| 1. | The expenditure accrued to the category by the beneficiary during the year; and, |
| 2. | The expenditure cap that applies to that entitlement category for that year. |
The expenditure cap is based on the experience accrued by the beneficiary to the entitlement category. It is equal to the product of:
| 1. | The PBPM cap on expenditures for the entitlement category for that year; |
| 2. | The number of months that the beneficiary accrued to the entitlement category during the year; |
The PBPM cap on expenditures for a given entitlement category is the 99th percentile of the expenditure PBPM amount incurred by all alignment-eligible beneficiaries who accrue experience to the entitlement category during the year. Expenditure caps will be based on national experience.
When required by a calculation (e.g., for a capped baseline or for the calculation of an efficiency ratio), the capped expenditure incurred by a beneficiary is determined separately by entitlement category based on the expenditure incurred by a beneficiary during months in which the beneficiary contributed experience to an entitlement category.
| 3.9 | Provider payments made outside of standard claims systems |
Subject to Section 3.7.6 of this Appendix, payments and adjustments to payments for services provided to identifiable beneficiaries that are made outside the standard Part A and Part B claims systems will also be included in calculation of the ACO and reference baseline and performance-period expenditures.
| 3.10 | Quality Measures |
Quality measures and performance standards in the NGACO Model will be aligned with those in MSSP and other CMS quality measurement efforts. For each Performance Year, the Model will generally follow quality domains, measures, benchmarking methodology, sampling, and scoring as reflected in the most recent final regulations for MSSP and the Physician Fee Schedule. Appendix F describes quality measurement for the NGACO Model.
| 4.1 | NGACO benchmark for each entitlement category |
Separate benchmarks will be calculated for each entitlement category. The Benchmark for an entitlement category is calculated in four steps:
| 1. | Step 1: Calculate the NGACO baseline expenditure for the entitlement category; |
| 2. | Step 2: Calculate the trended baseline by applying a projected regional trend component; |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 5.0 | Trended baseline | 10 |
| 3. | Step 3: Calculate the risk-adjusted trended baseline by apply a risk adjustment factor reflecting the difference between the average risk of the base-year aligned beneficiaries and the average risk of the performance-year aligned beneficiaries; and, |
| 4. | Step 4: Calculate the Benchmark by applying a quality- and efficiency-adjusted discount. |
The baseline expenditure and projected regional trend are discussed in section 5. Risk adjustment is discussed in section 6. The calculation of the quality- and efficiency-adjusted discount is discussed in section 7. The use of the Benchmark in financial settlement is discussed in section 8.
| 5.0 | Trended baseline |
The trended baseline for an entitlement category will be set prospectively on the basis of the NGACO’s baseline expenditure for the entitlement category and a projected regional trend.
For a given Performance Year, the trended baseline for each entitlement category is the product of the NGACO baseline expenditure and the regional trend.
| 5.1 | NGACO baseline expenditure |
The baseline expenditure PBPM for an entitlement category is the total capped expenditure accrued to the entitlement category by all base-year aligned beneficiaries divided by the total months accrued to the entitlement category by those beneficiaries.
| 5.2 | Projected regional trend |
A projected regional trend will be calculated for each entitlement category. It will be the product of:
| 1. | A National projected FFS trend (expenditure percentage growth rate) for the entitlement category similar to that currently used by the Medicare Office of the Actuary (OACT) in its calculation of the Medicare Advantage county ratebook; and, |
| 2. | A regional GAF trend-adjustment that accounts for the impact of the performance-year Medicare geographic price factors on baseline expenditure. |
The projected regional trend will be set prior to the start of the Performance Year and will be applied to final settlement without retrospective adjustments to account for the difference between projected and actual trend. Under limited circumstances, CMS may adjust the projected trend in response to unforeseeable events such as legislative actions that have a substantial impact on Medicare FFS expenditures.
| 5.3 | Projected national FFS trend |
The projected national FFS expenditure trend (percentage growth rate) will be determined using assumptions and methods similar to those used by the Medicare Office of the Actuary (OACT) to calculate the Medicare Advantage (MA) county ratebook. OACT calculates a projected FFS United States
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 5.1 | Trended baseline | 11 |
Per Capita Cost (USPCC), which is used in the calculation of the ratebook.7 Adjustments to the projected FFS USPCC may be made to take into account differences in the expenditure trend of the FFS population as a whole, and the subset of FFS beneficiaries eligible to be aligned to ACOs (see Section 3.5). The beneficiaries eligible for alignment to an NGACO (i.e., NGACO reference beneficiaries) are the vast majority of FFS beneficiaries.
For each Performance Year the projected trend will be the projected percentage difference between the base year (CY2014) and:
| 1. | In PY1: CY2016 |
| 2. | In PY2: CY2017 |
| 3. | In PY3: CY2018 |
The prospective projected trend will be set in the quarter prior to the start of the performance-year using OACT’s most recent projection of FFS spending for the performance year. For example, in Performance Year 1 (2016), the trend is from 2014 through 2016, and will be set during the last quarter of 2015.
| 5.4 | GAF trend adjustment |
Medicare FFS payments under most Medicare payment systems are adjusted to reflect the cost-of- doing-business in the local geographic area in which the provider operates. Examples of these Geographic Adjustment Factors (GAFs) are the Medicare area wage index (AWI) and the geographic practice cost index (GPCI). These local geographic price adjustments are updated annually.
The purpose of the GAF trend adjustment in the NGACO Model is to prevent the benchmark from being unfairly understated (or overstated) because of differences between the GAFs that Medicare used to calculate provider payments in the base-year (CY2014) and the performance-year.
Separate GAF trend-adjustments will be calculated for the Aged/Disabled and ESRD populations.
7 The methodology used by OACT to project the FFS spending is described in the Annual Report of the Trustees of the Federal Hospital insurance and Federal Supplementary Medical Insurance Trust Funds: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/Downloads/TR2015.pdf. The projected FFS USPCC is used by OACT in the calculation of the Medicare Advantage county ratebook. The projected FFS USPCC for 2016 was published in the Announcement of Calendar Year (CY) 2016 Medicare Advantage Capitation Rates and Medicare Advantage and Part D Payment Policies and Final Call Letter published April 6: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/Announcement2016.pdf.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 5.0 | Trended baseline | 12 |
| 5.4.1 | Calculation of GAF trend adjustment factors |
The GAF trend adjustment factor for a county is an estimate of the impact on base-year provider payments for services provided to reference beneficiaries residing in the county of the difference between the base-year Medicare GAFs and the performance year Medicare GAFs.
The GAF trend-adjustment factor for a county will be the ratio of:
| 1. | The county PBPM expenditure calculated after adjusting base year claims to reflect the impact on provider payments of the geographic pricing factors that Medicare will use in the performance year; to, |
| 2. | The actual incurred county PBPM expenditure (reflecting the geographic pricing factors that Medicare used to calculate provider payments in the base year). |
The GAF-trend adjustment factor will be calculated prospectively for alignment-eligible beneficiaries in each county in the base year and will have no impact on the national FFS trend.
The GAF trend-adjustment factor for an ACO will be the person-month weighted average of county GAF- trend adjustment factors, where the weights are the ACO aligned beneficiary person months residing in each county.
| 5.4.2 | GAF trend-adjusted baseline claims |
To calculate the GAF trend adjustment, baseline claims will be adjusted to reflect the impact of Performance-Year GAFs on baseline expenditures. Baseline claims will be adjusted using appropriately weighted performance year geographic pricing factors. For example:
| · | The geographic price adjustment under the Inpatient Prospective Payment System (IPPS), the Area Wage Index (AWI), is weighted by the proportion of cost that is attributable to labor. |
| · | Under the Physician Fee Schedule, the three Geographic Practice Cost Indexes (GPCIs) are weighted by the corresponding relative value units. |
Adjusted payment amounts using Performance-Year geographic pricing factors will be calculated for each the following types of claims:
| 1. | Inpatient claims paid under Prospective Payment Systems. |
| 2. | Outpatient claims paid under the Hospital Outpatient Prospective Payment System (HOPPS). |
| 3. | Skilled Nursing Facility claims paid under the SNF Prospective Payment System. |
| 4. | Home Health claims paid under the HHA Prospective Payment System. |
| 5. | Hospice claims. |
| 6. | Physician claims paid under the Physician Fee Schedule. |
| 7. | Claims paid under the Renal Dialysis Prospective Payment System. |
For all other claims, the adjusted payment amount will be equal to the amount actually paid.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 6.0 | Risk Adjustment of Trended Baseline | 13 |
| 6.1 | Risk Adjustment of Trended Baseline |
The trended baseline (see Section 5) will be risk adjusted to account for the difference between:
| 1. | The average health status of the ACO’s base-year aligned beneficiaries; and, |
| 2. | The average health status of Next Generation Beneficiaries aligned in the Performance Year. |
This difference in risk will be measured using Centers for Medicare & Medicaid Services Hierarchical Condition Categories risk scores (HCC risk scores).
| 6.1 | Risk scores |
HCC risk scores are used to more accurately measure the expected expenditure for a Performance Year of a beneficiary that is based on the clinical conditions for which a beneficiary was treated in the prior year. CMS maintains HCC prospective risk adjustment models for the Medicare Advantage (MA) program. HCC risk models are prospective in the sense that diagnoses obtained from claims in the prior year are used to predict expenditure in the current year. For example, diagnoses from claims for services provided in CY2013 are used to calculate the CY2014 risk score, which represents the beneficiary’s expected CY2014 expenditures. HCC risk scores are calculated for all Medicare beneficiaries, including FFS beneficiaries. Thirteen separate models are used to predict the cost of different beneficiary subpopulations including:
| 1. | Community-residing Aged/Disabled beneficiaries; |
| 2. | Aged/Disabled beneficiaries residing in long-term institutional settings; |
| 3. | New Aged/Disabled Medicare enrollees; |
| 4. | Aged/Disabled beneficiaries with functioning graft (post-kidney-transplant); |
| 5. | ESRD beneficiaries receiving dialysis; |
| 6. | ESRD beneficiaries during the three months following a kidney transplant. |
One or more of the risk scores calculated using these models may be applicable to a beneficiary during a given calendar month. For example, a beneficiary who has been living in the community may become a resident of a long-term care institution during the year. The risk score from the community-residing model will be used for months in which the beneficiary was living in the community, while the long-term institutional risk score will be used for months in which the beneficiary is a long-term resident of a nursing facility.
The MA risk adjustment model(s) that are used for each Benchmark and Performance Year will be used for risk adjustment in the NGACO Model. For example, the BY (CY2014) risk score(s) for a beneficiary will be the risk score(s) that were developed for the beneficiary using the MA risk adjustment models for CY2014. Risk scores without the MA coding intensity adjustment will be used for ACO risk adjustment.
| 6.2 | “Re-normalization” of Risk Scores |
Risk scores will be “re-normalized” to the average risk score of all alignment-eligible beneficiaries contributing experience to an entitlement category (e.g., A/D or ESRD) in each base- or Performance- Year. As a result, in each base- or Performance-Year the average re-normalized risk score for an entitlement category has a value of one (1.000). In other words, the risk scores are re-normalized to the reference population. A beneficiary’s “re-normalized” risk score for months in which a beneficiary contributes experience to an entitlement category is:
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 6.1 | Risk Adjustment of Trended Baseline | 14 |
| 1. | The beneficiary’s average risk score for months in which the beneficiary contributed experience to the entitlement category during the base- or Performance-Year; divided by, |
| 2. | The average risk score of all beneficiaries who contribute experience to the category during the base- or Performance-Year. |
The re-normalized risk score is calculated on a person-month weighted basis. An ACO’s re-normalized risk score measures the extent to which the beneficiaries aligned with the ACO who contribute experience to an entitlement category have a higher or lower expected cost in a base- or a Performance- Year relative to the average beneficiary contributing experience to that entitlement category in that year.
Using Aged/Disabled beneficiaries as an example,
| 1. | If the average risk score of the BY/CY2014 Next Generation Beneficiaries for a given NGACO is 1.052; and, |
| 2. | The average risk score of all BY/CY2014 reference beneficiaries is 1.038; |
| 3. | Then the re-normalized risk score of the Next Generation Beneficiaries is 1.013 (= 1.052 ÷ 1.038). |
The re-normalized risk score can be interpreted as an estimate of the amount by which the expected cost of NGACO’s aligned Aged/Disabled beneficiaries in a given entitlement category differs from the expected cost of all NGACO alignment-eligible beneficiaries in that entitlement category. In the above example, the expected cost of the NGACO’s Next Generation Beneficiaries is 1.3% higher than the expected cost of all NGACO alignment-eligible (reference) beneficiaries.
| 6.3 | Risk ratio |
For a given Performance Year and entitlement category, the risk ratio will equal the ratio of:
| 1. | The average HCC risk score of Next Generation Beneficiaries aligned in the Performance Year; to |
| 2. | The average HCC risk score for aligned beneficiaries in the base year. |
For example, in PY1 (CY2016), the risk ratio for an entitlement category is equal to:
| 1. | The average PY1 (CY2016) HCC risk score of all CY2016 Next Generation Beneficiaries belonging to the entitlement category in CY2016; divided by |
| 2. | The average BY (CY2014) HCC risk score of all CY2014-aligned beneficiaries belonging to the entitlement category in CY2014. |
The risk ratio for the ACO aligned beneficiaries between the baseline and the performance year will be capped at 0.97 and 1.03 (a percentage change of ±3% from base-year to performance-year).
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 7.0 | Quality- and efficiency-adjusted discount | 15 |
| 6.4 | Risk-adjusted trended baseline |
For a given performance year, the trended, risk adjusted baseline for each entitlement category is the product of the trended baseline and the risk ratio.
The risk-adjusted trended baseline will be retrospectively adjusted for final reconciliation based on the final risk scores for the Performance Year. For example, the PY1/CY2016 final risk scores are expected to be released in April 2017. The PY1/CY2016 final Benchmark will be updated to reflect the final PY1/CY2016 risk scores.
To the extent that preliminary or mid-year risk scores for the Performance Year are available during the Performance Year, CMMI may update the prospective Benchmark in the quarterly financial reports.
| 7.1 | Quality- and efficiency-adjusted discount |
The NGACO Benchmark will be calculated by applying to the trended, risk-adjusted baseline an efficiency- and quality-adjusted discount. The adjusted discount is:
| 1. | A standard discount of 2.25%. |
| 2. | MINUS: A regional efficiency adjustment of ±1.0% |
| 3. | MINUS: A national efficiency adjustment of ±0.5% |
| 4. | MINUS: A quality adjustment to the standard discount of up to +1.0% |
The adjusted discount for an NGACO can, therefore, vary from 0.0% to 3.75% as shown in table 7.0.
Table 7.0. Minimum and maximum quality- and efficiency-adjusted discount
| High efficiency / high quality ACO |
Low efficiency / low quality ACO |
|||||||
| The standard discount | 2.25 | % | 2.25 | % | ||||
| MINUS: Regional efficiency adjustment¹ | 1.0 | % | -1.0 | % | ||||
| MINUS: National efficiency adjustment² | 0.5 | % | -0.5 | % | ||||
| MINUS: Quality adjustment | 1.0 | % | 0.0 | % | ||||
| EQUALS: Quality- and efficiency-adjusted discount | 0.0 | % | 3.75 | % | ||||
| ¹ | The regional efficiency adjustment may be a positive or negative value between +1.0% and -1.0%. An “efficient” (low cost) ACO has a positive efficiency adjustment which is subtracted from the standard discount. The regional efficiency adjustment therefore reduces the standard discount for a low cost ACO. An “inefficient” (high cost) ACO has a negative efficiency adjustment that is subtracted from the standard discount. The regional efficiency adjustment therefore increases the standard discount for a high cost ACO. |
| ² | The national efficiency adjustment may be a positive or negative value between +0.5% and -0.5%. An “efficient” (low cost) ACO has a positive efficiency adjustment which is subtracted from the standard discount. The national efficiency adjustment therefore reduces the standard discount for a low cost ACO. An “inefficient” (high cost) ACO has a negative efficiency adjustment that is subtracted from the standard discount. The national efficiency adjustment therefore increases the standard discount for a high cost ACO. |
Separate quality- and efficiency-adjusted discounts will be calculated for Aged/Disabled and ESRD benchmarks. The efficiency adjustments will be calculated separately for Aged/Disabled and ESRD beneficiaries and may differ. However, the same quality adjustment will apply to both Aged/Disabled and ESRD components.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 7.0 | Quality- and efficiency-adjusted discount | 16 |
| 7.1 | Quality adjustment to the standard discount |
The quality adjustment to the standard Medicare savings requirement may be up to 1 percentage point. In other words, the standard discount of 2.25% may be reduced by as much as 1 percentage point based on the ACO’s quality performance. A higher quality score reduces the standard discount by more than a lower quality score.
For each performance year, the ACO’s quality score will range from 0% (0.000) to 100% (1.000). The quality adjustment to the standard discount will be the product of the quality score and 1%. Table 7.1 illustrates the relationship between the quality score and the quality adjustment to the standard discount.
Table 7.2.2 Quality adjustment to the standard discount for selected quality scores
| Quality score | Adjustment | |||
| 100 | +1.00% | |||
| 90 | +0.90% | |||
| 80 | +0.80% | |||
| 70 | +0.70% | |||
| 60 | +0.60% | |||
| 50 | +0.50% | |||
| 40 | +0.40% | |||
| 30 | +0.30% | |||
| 20 | +0.20% | |||
| 10 | +0.10% | |||
| 0 | +0.00% |
| 7.1.1 | Use of prior year quality score for the initial benchmark calculation |
In PY1/CY2016, for NGACOs with agreements effective January 1, 2016, the initial prospective Benchmark will be based on a quality score of 100 (or 100%) for all ACOs. In the event an ACO fails to successfully report for PY1, CMS will retrospectively adjust the quality score to zero.
In PY2/CY2017, the initial prospective Benchmark will be based on a quality score of 100% as PY1 quality scores will not be available at the time that the Benchmark is calculated. When PY1 quality scores are calculated at mid-year PY2, CMS will update the Performance Year Benchmark.8 For NGACOs with agreements effective January 1, 2017, the initial and mid-year update to the quality score will be 100%.
8 The PY1 quality score for purposes of calculation of the PY1 quality adjustment to the standard discount will be 100% assuming the NGACO reports all quality measures. However, a PY1 “baseline” quality score based on the NGACO’s performance on each quality measure will also be calculated. This PY1 “baseline” quality score will be used to calculate the mid-year quality adjustment to the standard discount in PY2.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 7.0 | Quality- and efficiency-adjusted discount | 17 |
For PY3, the prospectively-set quality score component will be based on the quality score from PY1. PY2 quality scores will be calculated in mid-2018. When PY2 quality scores become available, CMS will update the Performance Year Benchmark to reflect the PY2 quality score.
| 7.1.2 | Use of performance-year quality score for purposes of financial settlement |
The Performance Year Benchmark that is used in financial settlement will be based on an adjusted discount that reflects the actual performance-year quality score attained by the NGACO. In PY1/CY2016 the quality score used to calculate the final adjusted discount will be 100% if all quality data reporting requirements have been satisfied. In subsequent performance years, the quality score will be calculated as described in the Participation Agreement.
For NGACOs with agreements effective January 1, 2017, the PY2/CY2017 quality score used to calculate the final adjusted discount will be 100% unless the quality data reporting and other requirements described in the Participation Agreement have not been met.
| 7.1.3 | Minimum Quality Requirement |
Each NGACO must meet certain minimum quality requirements, including the submission of all data required to calculate quality scores. In the event an NGACO does not satisfy the minimum quality requirement, it will not be allowed to share in savings, but will be required to pay losses. The quality score for an NGACO that does not meet the quality measurement requirements of the Next Generation ACO Model will be zero. Details on the quality data reporting requirements are provided in Appendix F of the NGACO’s Participation Agreement.
| 7.2 | Regional Baseline Efficiency Adjustment to the standard discount |
The ratio of an ACO’s historic expenditures to regional FFS expenditures (regional efficiency), or the “regional efficiency ratio,” will be used to calculate a “regional efficiency” adjustment to the standard discount. The regional efficiency adjustment is intended to recognize the baseline expenditure “operating efficiency” of the NGACO when measured against a regional norm.
In this context, “operating efficiency” indicates whether the ACO’s baseline expenditure PBPM is higher or lower than the “average” baseline expenditure PBPM in the ACO’s region.9 Under this approach, ACOs achieve savings through year-to-year improvement over historic expenditures (improvement), but the magnitude by which they must improve will vary based on relative efficiency (attainment). The regional efficiency adjustment to the standard discount will be set prospectively. The regional baseline efficiency ratio will be calculated using capped expenditures for all NGACOs.
The regional baseline efficiency adjustment to the standard discount ranges from -1.0% to +1.0%. An NGACO with a base-year expenditure PBPM that is below the prevailing regional average base-year expenditure PBPM will therefore have a smaller adjusted discount than an NGACO with baseline expenditures that are above average in its region.
9 Risk adjustment and geographic pricing adjustment are applied to the regional efficiency adjustment. See below for details.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 7.0 | Quality- and efficiency-adjusted discount | 18 |
| 7.2.1 | Regional baseline efficiency ratio |
A regional baseline efficiency ratio will be calculated for each entitlement category. The regional efficiency ratio is a measure of the ACO’s efficiency relative to its region. The regional efficiency ratio will be the ratio of.
| 1. | The NGACO’s risk- and GAF-standardized baseline expenditure PBPM; and, |
| 2. | The NGACO’s regional risk- and GAF-standardized baseline expenditure PBPM. |
As noted in section 3.7.2, IME and DSH will be excluded from all expenditures when calculating the regional efficiency ratio. IME and DSH are not related to an ACO’s regional efficiency, and inclusion of IME and DSH in the regional expenditure ratio could create bias in the NGACO Model.
The NGACO’s risk- and GAF-standardized baseline expenditure PBPM for an entitlement category is:
| 1. | The NGACO’s baseline expenditure (excluding IME and DSH) PBPM; divided by |
| 2. | The product of: |
| a. | The NGACO’s re-normalized risk score; and |
| b. | The NGACO’s baseline GAF standardization factor. |
The NGACO’s regional risk- and GAF-standardized baseline expenditure PBPM is the weighted average of the risk- and GAF-standardized expenditure of the counties in which the NGACO’s base-year aligned beneficiaries reside. The weights used are the months accrued by the base-year aligned beneficiaries residing in each county.
| 7.2.2 | GAF baseline standardization factors |
A GAF baseline adjustment factor will be calculated for each county that reflects the impact on base- year payments to providers and suppliers for services provided to reference beneficiaries residing in the county of the base-year Medicare GAFs. The resulting GAF-standardized payment is an estimate of the payment that would have been made if no GAF adjustments had been applied when calculating payments to providers and suppliers.
The GAF baseline adjustment factor for a county will be the ratio of:
| 1. | The incurred PBPM expenditure (reflecting the geographic pricing factors that Medicare used in the base-year to calculate payments to providers and suppliers); to |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 7.0 | Quality- and efficiency-adjusted discount | 19 |
| 2. | The county PBPM expenditure calculated after adjusting base year claims to remove the impact on payments to providers and suppliers of the geographic pricing factors that Medicare used in the base-year. 10 |
The GAF baseline adjustment factor will be calculated prospectively for alignment-eligible beneficiaries in each county in the base year and will have no impact on the national FFS trend.
The GAF baseline adjustment for an ACO will be the person-month weighted average of county GAF baseline adjustment factors, where the weights are the ACO aligned beneficiary person months residing in each county.
| 7.2.3 | GAF-adjusted baseline claims |
The GAF baseline adjustment removes the impact on payments to providers and suppliers of the GAFs that Medicare applied when calculating payments in the base-year. Baseline claims will be adjusted using appropriately weighted base-year geographic pricing factors. For example:
| · | The geographic price adjustment under the Inpatient Prospective Payment System (IPPS), the Area Wage Index (AWI), is weighted by the proportion of cost that is attributable to labor. |
| · | Under the Physician Fee Schedule, the three Geographic Practice Cost Indexes (GPCIs) are weighted by the corresponding relative value units. |
Adjusted payment amounts using performance-year geographic pricing factors will be calculated for each the following types of claims:
| 1. | Inpatient claims paid under Prospective Payment Systems. |
| 2. | Outpatient claims paid under the Hospital Outpatient Prospective Payment System (HOPPS). |
| 3. | Skilled Nursing Facility claims paid under the SNF Prospective Payment System. |
| 4. | Home Health claims paid under the HHA Prospective Payment System. |
| 5. | Hospice claims. |
| 6. | Physician claims paid under the Physician Fee Schedule. |
| 7. | Claims paid under the Renal Dialysis Prospective Payment System. |
For all other claims, the adjusted payment amount will be equal to the amount actually paid.
| 7.2.4 | Risk- and GAF-adjusted expenditure PBPM for each county |
The risk- and GAF-adjusted baseline expenditure PBPM for each county is:
10 The calculation of the baseline GAF adjustment will be normalized such that the adjustment neither increases nor decreases the total expenditure of the reference population. That is the adjusted claim amount for the reference population will equal the incurred claim amount.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 7.1 | Quality- and efficiency-adjusted discount | 20 |
| 1. | The baseline expenditure (excluding IME and DSH) PBPM incurred by reference beneficiaries residing in the county; divided by |
| 2. | The product of: |
| a. | The weighted average re-normalized risk score of reference beneficiaries residing in the county; and |
| b. | The baseline GAF standardization factor of the county. |
Separate ESRD and Aged/Disabled risk- and GAF-adjusted baseline expenditure PBPM will be calculated for each county.
| 7.2.5 | Regional Efficiency Adjustment |
For each entitlement category, the regional efficiency adjustment to the Medicare savings requirement ranges from -1.0% to +1.0%. If the regional efficiency ratio is:
| · | Less than 0.9, then the regional efficiency adjustment is +1.0%; |
| · | Between 0.9 and 1.0, then the regional efficiency adjustment is between 0.0% and +1.0%; |
| · | Between 1.0 and 1.1, then the regional efficiency adjustment is between 0.0% and -1.0%; and, |
| · | Greater than 1.1, then the regional efficiency adjustment is -1.0%. |
The floor (and ceiling) for the risk adjusted, geographically price adjusted regional efficiency ratio that an ACO must attain to receive the “maximum” (or “minimum”) regional efficiency adjustment is thus 10% below or above average, respectively.
Table 7.2.5 shows the regional efficiency adjustment that will be applied at selected regional efficiency ratios. Between the minimum and maximum efficiency ratios, the adjustment is a simple linear interpolation based on the regional efficiency ratio.
Table 7.2.5 Regional efficiency adjustment for selected regional efficiency ratios
| Regional efficiency ratio | Adjustment¹ | Regional efficiency ratio | Adjustment¹ | |||||||||
| 0.90 or less | +1.00% | 1.00 | -0.00% | |||||||||
| 0.91 | +0.90% | 1.01 | -0.10% | |||||||||
| 0.92 | +0.80% | 1.02 | -0.20% | |||||||||
| 0.93 | +0.70% | 1.03 | -0.30% | |||||||||
| 0.94 | +0.60% | 1.04 | -0.40% | |||||||||
| 0.95 | +0.50% | 1.05 | -0.50% | |||||||||
| 0.96 | +0.40% | 1.06 | -0.60% | |||||||||
| 0.97 | +0.30% | 1.07 | -0.70% | |||||||||
| 0.98 | +0.20% | 1.08 | -0.80% | |||||||||
| 0.99 | +0.10% | 1.09 | -0.90% | |||||||||
| 1.00 | +0.00% | 1.10 or higher | -1.00% | |||||||||
| ¹ | The efficiency adjustment is subtracted from the standard discount. A positive adjustment therefore reduces the standard discount, and a negative adjustment increases it. |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 7.0 | Quality- and efficiency-adjusted discount | 21 |
| 7.3 | National Baseline Efficiency Adjustment to the Savings Requirement |
The ratio of an ACO’s historic expenditures to national FFS expenditures (national efficiency), or the “national efficiency ratio”, will be used to calculate a “national efficiency” adjustment to the standard discount. The national efficiency adjustment is intended to recognize the baseline expenditure “operating efficiency” of the NGACO when measured against a national norm.
In this context, “operating efficiency” simply means whether the ACO’s baseline expenditure PBPM is higher or lower than the “average” baseline expenditure PBPM in the nation as a whole. Under this approach, ACOs achieve savings through year-to-year improvement over historic expenditures (improvement), but the magnitude by which they must improve will vary based on relative efficiency (attainment). The national efficiency adjustment to the standard discount will be set prospectively.
The national baseline efficiency adjustment to the standard discount ranges from -0.5% to +0.5%. An NGACO with a base-year expenditure PBPM that is below the national average base-year expenditure PBPM will therefore have a smaller adjusted discount applied to its risk-adjusted trended baseline than an NGACO with baseline expenditures that are above average nationally.
The national baseline efficiency ratio will be calculated using capped expenditures for all NGACOs.
| 7.3.1 | National Efficiency Ratio |
A national baseline efficiency ratio will be calculated for each entitlement category. The national efficiency ratio is a measure of the ACO’s efficiency relative to the entire reference population. The national efficiency ratio will be the ratio of.
| 1. | The NGACO’s risk- and GAF-adjusted baseline expenditure PBPM; and, |
| 2. | The national risk- and GAF-adjusted baseline expenditure PBPM.11 |
As noted in section 3.7.2, IME and DSH will be excluded from all expenditures when calculating the national efficiency ratio. IME and DSH are not related to an ACO’s national efficiency, and inclusion of IME and DSH in the national expenditure ratio could create bias in the NGACO Model.
The NGACO’s risk- and GAF-adjusted baseline expenditure PBPM for an entitlement category is discussed in section 7.2.1.
11 The national risk- and GAF-adjusted baseline expenditure PBPM will, because of the steps taken to ensure that the standardization process neither increases nor decreases total expenditures, will equal the incurred expenditure PBPM of the reference population.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 8.1 | NGACO Financial Settlement | 22 |
| 7.3.2 | National Efficiency Adjustment |
The national efficiency adjustment to the Medicare savings requirement ranges from -0.5% to 0.5%. If the national efficiency ratio is:
| · | Less than 0.9, then the national efficiency adjustment is +0.5%; |
| · | Between 0.9 and 1.0, then the national efficiency adjustment is between 0.0% and +0.5%; |
| · | Between 1.0 and 1.1, then the national efficiency adjustment is between 0.0% and -0.5%; |
| · | Greater than 1.1, then the national efficiency adjustment is -0.5%. |
The floor (and ceiling) for the risk adjusted, geographically price adjusted national efficiency ratio that an ACO must attain to receive the “maximum” (or “minimum”) national efficiency adjustment is thus 10% below or above average, respectively. Between the minimum and maximum efficiency ratios, the adjustment is a simple linear interpolation based on the national efficiency ratio.
Table 8.3.2 shows the national efficiency adjustment that will be applied at selected national efficiency ratios.
Table 7.3.2. National efficiency adjustment for selected national efficiency ratios
| National efficiency ratio | Adjustment¹ | National efficiency ratio | Adjustment¹ | |||||||||
| 0.90 or less | +0.50% | 1.00 | -0.00% | |||||||||
| 0.91 | +0.45% | 1.01 | -0.05% | |||||||||
| 0.92 | +0.40% | 1.02 | -0.10% | |||||||||
| 0.93 | +0.35% | 1.03 | -0.15% | |||||||||
| 0.94 | +0.30% | 1.04 | -0.20% | |||||||||
| 0.95 | +0.25% | 1.05 | -0.25% | |||||||||
| 0.96 | +0.20% | 1.06 | -0.30% | |||||||||
| 0.97 | +0.15% | 1.07 | -0.35% | |||||||||
| 0.98 | +0.10% | 1.08 | -0.40% | |||||||||
| 0.99 | +0.05% | 1.09 | -0.45% | |||||||||
| 1.00 | +0.00% | 1.10 or higher | -0.50% | |||||||||
| ¹ | The efficiency adjustment is subtracted from the standard discount. A positive adjustment therefore reduces the standard discount, and a negative adjustment increases it. |
| 8.1 | NGACO Financial Settlement |
As discussed in section 4, the NGACO Benchmark PBPM for each entitlement category is the product of:
| 1. | The trended, risk adjusted ACO baseline; and, |
| 2. | The quality- and efficiency-adjusted discount.12 |
12 Technically, the PBPM benchmark is equal to the trended risk-adjusted baseline multiplied by 1 minus the quality- and efficiency adjusted discount.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 8.1 | NGACO Financial Settlement | 23 |
The overall NGACO Benchmark expenditure for a Performance-Year is the sum of two amounts:
| 1. | The Benchmark for Aged/Disabled beneficiaries multiplied by the person-months accrued by to the Aged/Disabled entitlement category by Next Generation Beneficiaries during the Performance-Year; and, |
| 2. | The Benchmark for ESRD beneficiaries multiplied by the person-months accrued by to the ESRD entitlement category by Next Generation Beneficiaries during the Performance-Year. |
This can be expressed as a PBPM Benchmark by dividing the Benchmark expenditure by the number of person-months accrued during the Performance-Year by aligned beneficiaries.13
| 8.1 | Savings/Losses Amount |
An NGACO’s aggregate gross savings or losses will be determined by subtracting the expenditure incurred by Performance-Year aligned beneficiaries in the Performance-Year from the NGACO’s Benchmark expenditure.
The risk arrangement selected by the NGACO will determine the portion of the aggregate gross savings that will be paid to (or the portion of the gross loss that will be recovered from) the NGACO. The NGACO Model offers two risk arrangements:
| 1. | Arrangement A: 80% shared savings/losses, ACO selects a savings/losses cap between 5-15%. |
| 2. | Arrangement B: 100% shared savings/losses, ACO selects a savings/losses cap between 5-15%. |
The shared savings (loss) for an NGACO that elects Arrangement A will be 80% of the difference between the Benchmark expenditure for the Performance Year and the expenditure incurred during the Performance-Year.
The shared savings (loss) for an NGACO that elects Arrangement B will be 100% of the difference between the Benchmark expenditure for the Performance Year and the expenditure incurred during the Performance-Year.
Budget sequestration will apply to shared savings payments, but will not apply to recover of shared losses. For example, if the budget sequestration rate is 2%, the shared savings payment to the NGACO will be 98% of the shared savings amount, but 100% of the shared loss amount will be recovered from the NGACO.
13 The combined benchmark is, therefore, simply the person-month weighted average of the Aged/Disabled and ESRD PBPM benchmarks.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| 8.0 | NGACO Financial Settlement | 24 |
| 8.2 | Alternative payment arrangements |
Under the Next Generation ACO Model, an NGACO may participate in alternative payment arrangements, including an infrastructure payment arrangement, population-based payment (PBP), and (starting in Performance Year 2) all-inclusive population-based payment (AIPBP).
The payment made over the course of the performance-year to an NGACO that receives infrastructure payments will be deducted from any savings (or added to any loss) during financial settlement and will be considered Other Monies Owed in accordance with Appendix G of the Participation Agreement.
The payments that are made to an NGACO that participates in population-based payment will be reconciled with the reduction in FFS payments in accordance with Appendix H of the Participation Agreement. If the FFS reduction is less than the PBP payment, the difference will be deducted from the savings payment or added to the loss and be considered Other Monies Owed. If the FFS reduction is greater than the PBP payment, the difference will be added to the savings payment or added to the loss and be considered Other Monies Owed.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 25 |
Appendix A. Next Generation ACO Model Alignment Procedures
| A.1 | Alignment Years |
Each Performance Year or base-year is associated with two alignment-years. The first alignment-year for a Performance Year or base-year is the 12-month period ending 18 months prior to the start of the Performance Year or base-year. The second-alignment year is the 12-month period ending 6 months prior to the start of the Performance Year or base-year. In this document, an Alignment Year is identified by the calendar year in which the alignment-year ends. For example, Alignment Year 2014 (AY2014) is the 12-month period ending in June 2014.
Table A.1 specifies the period covered by each base year and Performance Year, and their corresponding alignment years.
| A.2 | Definitions used in alignment procedures |
| A.2.1 | Alignment-eligible beneficiary |
A beneficiary is alignment-eligible for a base- or Performance-Year if:
| 1. | During the related 2-year alignment period, the beneficiary had at least one paid claim for a QEM (Qualified Evaluation and Management) service; and, |
| 2. | During the base- or Performance Year, the beneficiary: |
| a. | Was covered under Part A in January; |
| b. | Has no months of coverage under only Part A; |
| c. | Has no months of coverage under only Part B; |
| d. | Has no months of coverage under a Medicare Advantage or other Medicare managed care plan; |
| e. | Has no months in which Medicare was the secondary payer; |
| f. | Was a resident of the United States; |
A beneficiary may be alignment-eligible in a base-year but not a Performance Year and may be alignment-eligible in a Performance Year but not a base-year.
| A.2.2 | “Alignable” beneficiary |
To be aligned, a beneficiary necessarily must have at least one paid claim for a QEM service during the 2- year alignment period, but the beneficiary is not required to be alignment-eligible in either of the two alignment years. Consequently, the beneficiaries who are aligned for a base year or a Performance Year, prior to the application of the requirements for alignment-eligibility, include all beneficiaries who have at least one QEM service that was paid by fee-for-service Medicare during the 2-year alignment period. These beneficiaries may be referred to as “alignable” beneficiaries.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 26 |
| A.2.3 | NGACO Service Area |
The NGACO’s Service Area consists of all counties in which Next Generation Professionals who are primary care specialists have office locations and the adjacent counties. The counties in which Next Generation Participants have office locations will be referred to as the “core” service area. The counties adjacent to the “core” service area may be referred to as the “extended” service area. The NGACO is responsible for identifying the counties in which their Next Generation Professionals have office locations, i.e., the “core” service area.
| A.2.4 | Qualified Evaluation & Management services |
Qualified Evaluation & Management (QEM) services are identified by the Healthcare Common Procedure Coding System (HCPCS) codes listed in Addendum A, Table A-1, and physician specialty. Specifically, a QEM service is a claim for a primary care service provided by a primary care specialist or, for purposes of the 2nd stage of the 2-stage alignment algorithm discussed in section A.6, one of the selected non-primary care specialist.
In the case of claims submitted by physician practices, the specialty of the practitioner providing a primary care service will be determined by the CMS specialty code appearing on the claim. The specialty codes that identify primary care and selected non-primary care specialties are listed in Addendum A, Tables A-2 or A-3.
In the case of claims submitted by institutional practices, the specialty of the practitioner providing a primary care service will generally be determined based on the physician’s primary specialty as recorded in NPPES or PECOS.
| A.2.5 | Primary care services |
In the case of claims submitted by physician practices, a primary care service is identified by the HCPCS code appearing on the claim line. HCPCS codes identifying primary care services are listed in Addendum A, Table A-1.
In the case of claims submitted by an FQHC (type of bill = 77x) a primary care service is identified by HCPCS code appearing on the line item claim for the service.
In the case of claims submitted by an RHC (type of bill = 71x) a primary care service is identified by HCPCS code appearing on the line item claim for the service.
In the case of claims submitted by a CAH2 (type of bill = 85x) a primary care service is identified by HCPCS code appearing on the line item claim (for revenue centers 096x, 097x, or 098x) for the service.
| A.2.6 | Primary care specialists |
A primary care specialist is a physician or non-physician practitioner (NPP) whose principal specialty is included in Addendum A, Table A-2.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 27 |
For purposes of applying the provider exclusivity requirements, the physician or NPP’s specialty will be determined based on the physician or NPP’s current information in the National Plan & Provider Enumeration System (NPPES) at the time the participating provider data is submitted to the Center for Medicare and Medicaid Innovation (CMMI).
For purposes of applying the 2-stage alignment algorithm described in section A.6, the physician or NPP’s specialty will be determined based on the CMS Specialty Code recorded on the claim for a qualified E&M service. In the case of QEM services obtained from FQHC, RHC, or CAH Method 2 (CAH2) providers the specialty code may be determined based on the physician’s primary specialty as recorded in NPPES or PECOS.
| A.2.7 | Next Generation Participant |
A Next Generation Participant is a physician or non-physician practitioner (NPP) as defined in the Participation Agreement.
Next Generation Participants are identified by either:
| 1. | In the case of physician practices, a combination of Taxpayer Identification Number (TIN) and the practitioner’s individual National Provider Identifier (NPI). |
| 2. | In the case of institutional practices (including FQHCs, RHCs, and CAH2s), a combination of a CMS Certification Number (CCN) and the practitioner’s individual NPI. |
A Next Generation Participant who is a primary care specialist may be identified as a Next Generation Participant by one and only one NGACO.
| A.2.8 | Participating practice |
A participating practice is:
| 1. | A physician practice; |
| 2. | A Federally Qualified Health Center (FQHC); |
| 3. | A Rural Health Clinic (RHC); or, |
| 4. | A Critical Access Hospital that elects payment under Method 2 (CAH2) that has an agreement with an NGACO. |
A participating physician practice is identified by TIN.
An FQHC, RHC, or CAH2 practice is identified by TIN, CCN, and an organizational NPI.
| A.2.9 | Participating practitioner (professional) |
A participating practitioner (professional) is a physician or non-physician practitioner (NPP) identified by an individual National Provider Identifier (NPI) who is a member of a participating practice. A practitioner may be a member of more than one practice and may participate in more than one NGACO.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 28 |
| A.2.10 | Legacy practice identifiers |
A legacy practice identifier is a TIN or CCN that was used by a Next Generation Participant or Professional to bill for services provided to Medicare beneficiaries in an alignment-year for any of the base- or Performance-Years but that will not be used by that Next Generation Participant or Professional during the Performance Year.
A sunsetted legacy practice identifier means that the TIN or CCN is no longer used by any Medicare providers and/or suppliers. NGACOs may include sunsetted legacy practice identifiers on their Next Generation Participant list.
An active legacy practice identifier is a TIN or CCN that is no longer used by a Next Generation Participant, but is still in use by some Medicare providers and/or suppliers that are not Next Generation Participants. Active legacy practice identifiers may only be included on the NGACO Participant List with written agreement from the practice. Next Generation ACOs will submit legacy practice identifier acknowledgement forms annually for each active legacy practice.
A legacy practice identifier (a TIN or CCN) cannot be used to identify a Next Generation Participant if the practice it identifies is participating in or intends to participate in a Medicare Shared Savings Program ACO during the Performance Year.
| A.3 | Quarterly exclusion of beneficiaries during the Performance Year |
Alignment-eligibility requirements 2.a through 2.f (see section A.2.1) will be applied during the Performance Year in the first month of each calendar quarter.
A beneficiary who is determined not to be alignment-eligible in one quarter will be continue to be considered ineligible even if subsequent updates to eligibility data indicate that the beneficiary was eligible in a subsequent quarter. Once a beneficiary is excluded in a Performance Year, the beneficiary is removed from all financial calculations for that year. All alignment-eligible Next Generation Beneficiaries except those who die during the Performance Year will, therefore, contribute 12 months of experience to the Performance Year expenditures.
| A.4 | Alignment of beneficiaries |
Next Generation Beneficiaries are identified prospectively, prior to the start of the Performance Year. Similarly, the beneficiaries who are aligned in each base-year for the purpose of calculating the baseline expenditure are identified on the basis of each beneficiary’s use of QEM services in the 2-year alignment period ending prior to the start of the base-year.
Alignment of a beneficiary is determined by comparing:
| 1. | The weighted allowable charge for all QEM services that the beneficiary received from each NGACOs’ Next Generation Participants; |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 29 |
| 2. | The weighted allowable charge for all QEM services that the beneficiary received from each physician practice (including institutional practices) whose members are not participating in an NGACO. |
A beneficiary is aligned with the NGACO or the physician practice from which the beneficiary received the largest amount of QEM services during the 2-year alignment period. A beneficiary will generally be aligned with a Next Generation ACO if he or she received the plurality of QEM services during the 2-year alignment window from Next Generation Participants.
Only claims that are identified as being provided by the primary care specialists listed in Addendum A, Table A-2 and the non-primary care specialists listed in table A-3 will be used in alignment calculations.
| A.5 | Use of weighted allowable charges in alignment |
The allowable charge on paid claims for services received during the two alignment-years associated with each base- or Performance Year will be used to determine the Next Generation ACO or physician practice from which the beneficiary received the most QEM services.
| 1. | The allowable charge for QEM services provided during the 1st (earlier) alignment-year will be |
weighted by a factor of ⅓.
| 2. | The allowable charge for QEM services provided during the 2nd (later or more recent) alignment- |
year will be weighted by a factor of ⅔.
The allowable charge that is used in alignment will be obtained from claims for QEM services that are:
| 1. | Incurred in each alignment-year as determined by the date-of-service on the claim line-item; and, |
| 2. | Paid within 3 month following the end of the 2nd alignment-year as determined by the effective date of the claim. |
| A.6 | The 2-stage alignment algorithm |
Alignment for a base- or performance-year uses a two-stage alignment algorithm.
| 1. | Alignment based on primary care services provided by primary care specialists. If 10% or more of the allowable charges incurred on QEM services received by a beneficiary during the 2-year alignment period are obtained from physicians and practitioners with a primary care specialty as defined in Addendum A, Table A-2, then alignment is based on the allowable charges incurred on QEM services provided by primary care specialists. |
| 2. | Alignment based on primary care services provided by selected non-primary care specialties. If less than 10% of the QEM services received by a beneficiary during the 2-year alignment period are provided by primary care specialists, then alignment is based on the QEM services provided by physicians and practitioners with certain non-primary specialties as defined in Addendum A, Table A-3. |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 30 |
Provider specialty is determined by the specialty code that is assigned to the claim during claim processing, in the case of physician claims, or by the specialty associated with the NPI of the physician or NPP in the Medicare provider enrollment database in the case of certain FQHC, RHC and CAH2 claims.
| A.7 | Tie-breaker rule |
In the case of a tie in the dollar amount of the weighted allowed charges for QEM services, the beneficiary will be aligned with the provider from whom the beneficiary most recently obtained a QEM service.
| A.8 | Voluntary alignment |
A beneficiary who has agreed to voluntary alignment for a Performance-Year with an NGACO will be aligned to that NGACO for that Performance-Year (and related base-year) regardless of the NGACO with which the beneficiary would be aligned based on the 2-stage alignment algorithm.
Beneficiaries who have voluntarily aligned with an NGACO will also be excluded from the base- or Performance-Year alignment if they do not meet the alignment-eligibility requirements described in section A.2 during the base- or Performance-Year.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 31 |
Table 2.1: Definition of base years and Performance Years
| Period | Period covered¹ | Corresponding alignment years (AY) | ||
| Base Year (BY) | 01/01/2014 – 12/31/2014 | BY/AY1: 07/01/2011 – 06/30/2012 (AY2012) | ||
| BY/AY2: 07/01/2012 – 06/30/2013 (AY2013) | ||||
| Calendar Year 2015 (CY2015) | 01/01/2015 – 12/31/2015 | CY2015/AY1: 07/01/2012 – 06/30/2013 (AY2013) | ||
| CY2015/AY2: 07/01/2013 – 06/30/2014 (AY2014) | ||||
| Performance Year 1 (PY1) | 01/01/2016 – 12/31/2016 | PY1/AY1: 07/01/2013 – 06/30/2014 (AY2014) | ||
| PY1/AY2: 07/01/2014 – 06/30/2015 (AY2015) | ||||
| Performance Year 2 (PY2) | 01/01/2017 – 12/31/2017 | PY2/AY1: 07/01/2014 – 06/30/2015 (AY2015) | ||
| PY2/AY2: 07/01/2015 – 06/30/2016 (AY2016) | ||||
| Performance Year 3 (PY3) | 01/01/2018 – 12/31/2018 | PY3/AY1: 07/01/2015 – 06/30/2006 (AY2016) | ||
| PY3/AY2: 07/01/2016 – 06/30/2017 (AY2017) |
| ¹ | The period covered is the calendar year for which the expenditures of aligned beneficiaries will be calculated for purposes of setting the NGACO baseline or determining performance period savings. |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 32 |
Table A-1. Evaluation & Management Services – PY1/2016
| Office or Other Outpatient Services | |
| 99201 | New Patient, brief |
| 99202 | New Patient, limited |
| 99203 | New Patient, moderate |
| 99204 | New Patient, comprehensive |
| 99205 | New Patient, extensive |
| 99211 | Established Patient, brief |
| 99212 | Established Patient, limited |
| 99213 | Established Patient, moderate |
| 99214 | Established Patient, comprehensive |
| 99215 | Established Patient, extensive |
| Nursing Facility Care | |
| 99304 | Initial Nursing Facility Care, brief |
| 99305 | Initial Nursing Facility Care, moderate |
| 99306 | Initial Nursing Facility Care, comprehensive |
| 99307 | Subsequent Nursing Facility Care, brief |
| 99308 | Subsequent Nursing Facility Care, limited |
| 99309 | Subsequent Nursing Facility Care, comprehensive |
| 99310 | Subsequent Nursing Facility Care, extensive |
| 99315 | Nursing Facility Discharge Services, brief |
| 99316 | Nursing Facility Discharge Services, comprehensive |
| 99318 | Other Nursing Facility Services |
| Domiciliary, Rest Home, or Custodial Care Services | |
| 99324 | New Patient, brief |
| 99325 | New Patient, limited |
| 99326 | New Patient, moderate |
| 99327 | New Patient, comprehensive |
| 99328 | New Patient, extensive |
| 99334 | Established Patient, brief |
| 99335 | Established Patient, moderate |
| 99336 | Established Patient, comprehensive |
| 99337 | Established Patient, extensive |
| Domiciliary, Rest Home, or Home Care Plan Oversight Services | |
| 99339 | Brief |
| 99340 | Comprehensive |
| Home Services | |
| 99341 | New Patient, brief |
| 99342 | New Patient, limited |
| 99343 | New Patient, moderate |
| 99344 | New Patient, comprehensive |
| 99345 | New Patient, extensive |
| 99347 | Established Patient, brief |
| 99348 | Established Patient, moderate |
| 99349 | Established Patient, comprehensive |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 33 |
| Office or Other Outpatient Services | |
| 99350 | Established Patient, extensive |
| Wellness Visits | |
| G0402 | Welcome to Medicare visit |
| G0438 | Annual wellness visit |
| G0439 | Annual wellness visit |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 34 |
Table A-1. Evaluation & Management Services – PY2/2017
| Office or Other Outpatient Services | |
| 99201 | New Patient, brief |
| 99202 | New Patient, limited |
| 99203 | New Patient, moderate |
| 99204 | New Patient, comprehensive |
| 99205 | New Patient, extensive |
| 99211 | Established Patient, brief |
| 99212 | Established Patient, limited |
| 99213 | Established Patient, moderate |
| 99214 | Established Patient, comprehensive |
| 99215 | Established Patient, extensive |
| Domiciliary, Rest Home, or Custodial Care Services | |
| 99324 | New Patient, brief |
| 99325 | New Patient, limited |
| 99326 | New Patient, moderate |
| 99327 | New Patient, comprehensive |
| 99328 | New Patient, extensive |
| 99334 | Established Patient, brief |
| 99335 | Established Patient, moderate |
| 99336 | Established Patient, comprehensive |
| 99337 | Established Patient, extensive |
| Domiciliary, Rest Home, or Home Care Plan Oversight Services | |
| 99339 | Brief |
| 99340 | Comprehensive |
| Home Services | |
| 99341 | New Patient, brief |
| 99342 | New Patient, limited |
| 99343 | New Patient, moderate |
| 99344 | New Patient, comprehensive |
| 99345 | New Patient, extensive |
| 99347 | Established Patient, brief |
| 99348 | Established Patient, moderate |
| 99349 | Established Patient, comprehensive |
| 99350 | Established Patient, extensive |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 35 |
| Transitional Care Management Services | |
| 99495 | Communication (14 days of discharge) |
| 99496 | Communication (7 days of discharge) |
| Chronic Care Management Services | |
| 99490 | Comprehensive care plan establishment/implementations/revision/monitoring |
| Wellness Visits | |
| G0402 | Welcome to Medicare visit |
| G0438 | Annual wellness visit |
| G0439 | Annual wellness visit |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 36 |
Table A-2. Specialty codes used for alignment based on primary care specialists – PY1/2016
| Code¹ | Specialty |
| 1 | General Practice |
| 8 | Family Medicine |
| 11 | Internal Medicine |
| 38 | Geriatric Medicine |
| 50 | Nurse Practitioner |
| 97 | Physician Assistant |
| ¹ | The Medicare Specialty Code. A cross-walk between Medicare Specialty Codes and the Healthcare Provider Taxonomy is published on the CMS website at: https://www.cms.gov/Medicare/Provider-Enrollment-and- Certification/MedicareProviderSupEnroll/Downloads/TaxonomyCrosswalk.pdf |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 37 |
Table A-2. Specialty codes used for alignment based on primary care specialists – PY2/2017
| Code¹ | Specialty |
| 1 | General Practice |
| 8 | Family Medicine |
| 11 | Internal Medicine |
| 37 | Pediatric Medicine |
| 38 | Geriatric Medicine |
| 50 | Nurse Practitioner |
| 89 | Clinical nurse specialist |
| 97 | Physician Assistant |
| ¹ | The Medicare Specialty Code. A cross-walk between Medicare Specialty Codes and the Healthcare Provider Taxonomy is published on the CMS website at: https://www.cms.gov/Medicare/Provider-Enrollment-and- Certification/MedicareProviderSupEnroll/Downloads/TaxonomyCrosswalk.pdf |
Table A-3. Specialty codes used for alignment based on other selected specialists – PY1/2016
| Code¹ | Specialty |
| 6 | Cardiology |
| 13 | Neurology |
| 29 | Pulmonology |
| 39 | Nephrology |
| 46 | Endocrinology |
| 66 | Rheumatology |
| 83 | Hematology/oncology |
| 90 | Medical oncology |
| 91 | Surgical oncology |
| 92 | Radiation oncology |
| 98 | Gynecological/oncology |
| 86 | Neuropsychiatry |
Table A-3. Specialty codes used for alignment based on other selected specialists – PY2/2017
| Code¹ | Specialty |
| 6 | Cardiology |
| 12 | Osteopathic manipulative medicine |
| 13 | Neurology |
| 16 | Obstetrics/gynecology |
| 23 | Sports medicine |
| 25 | Physical medicine and rehabilitation |
| 26 | Psychiatry |
| 27 | Geriatric psychiatry |
| 29 | Pulmonology |
| 39 | Nephrology |
| 46 | Endocrinology |
| 70 | Multispecialty clinic or group practice |
| 79 | Addiction medicine |
| 82 | Hematology |
| 83 | Hematology/oncology |
| 84 | Preventative medicine |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
| Appendix A. Next Generation ACO Model Alignment Procedures | 38 |
| 90 | Medical oncology |
| 98 | Gynecological/oncology |
| 86 | Neuropsychiatry |
| ¹ | The Medicare Specialty Code. A cross-walk between Medicare Specialty Codes and the Healthcare Provider Taxonomy is published on the CMS website at: https://www.cms.gov/Medicare/Provider-Enrollment-and- Certification/MedicareProviderSupEnroll/Downloads/TaxonomyCrosswalk.pdf |
| NGACO Benchmarking Methods | Rev. 1.02.01 |
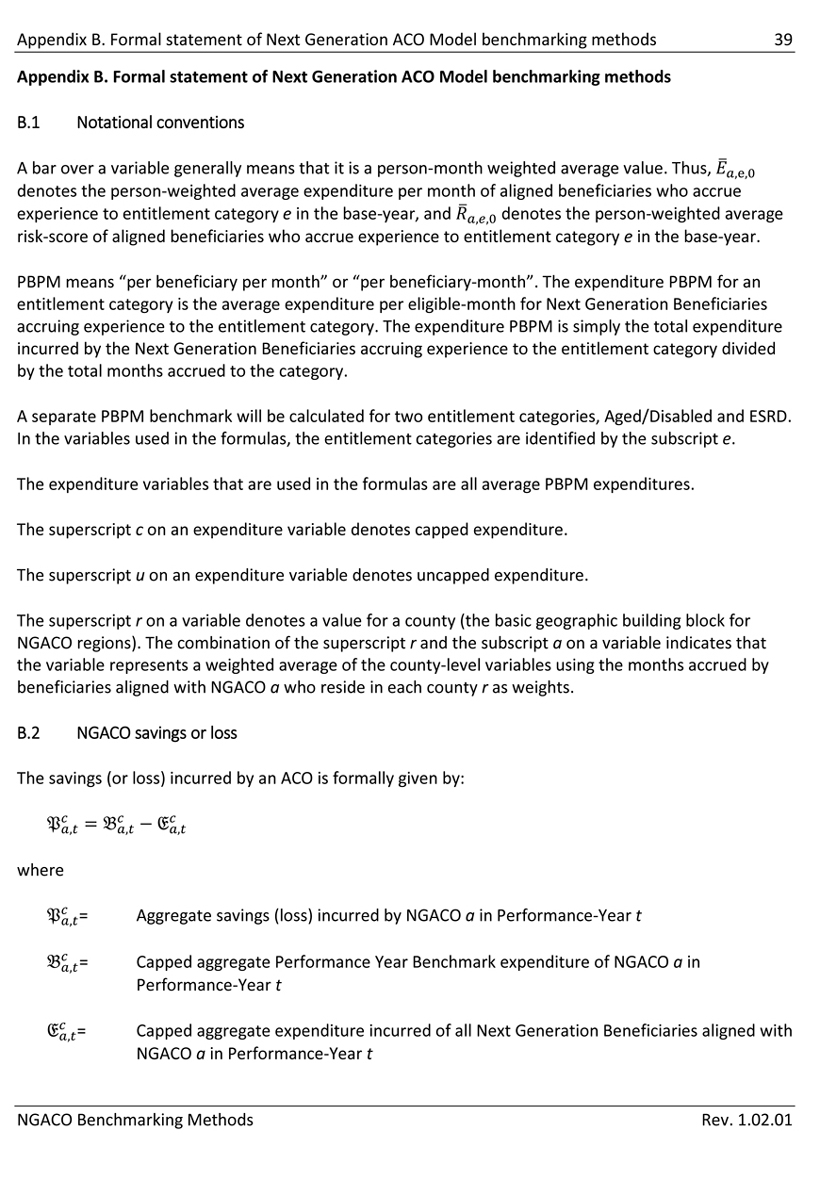
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 39 Appendix B. Formal statement of Next Generation ACO Model benchmarking methods B.1 Notational conventions A bar over a variable generally means that it is a person-month weighted average value. Thus, denotes the person-weighted average expenditure per month of aligned beneficiaries who accrue experience to entitlement category e in the base-year, and denotes the person-weighted average risk-score of aligned beneficiaries who accrue experience to entitlement category e in the base-year. PBPM means “per beneficiary per month” or “per beneficiary-month”. The expenditure PBPM for an entitlement category is the average expenditure per eligible-month for Next Generation Beneficiaries accruing experience to the entitlement category. The expenditure PBPM is simply the total expenditure incurred by the Next Generation Beneficiaries accruing experience to the entitlement category divided by the total months accrued to the category. A separate PBPM benchmark will be calculated for two entitlement categories, Aged/Disabled and ESRD. In the variables used in the formulas, the entitlement categories are identified by the subscript e. The expenditure variables that are used in the formulas are all average PBPM expenditures. The superscript c on an expenditure variable denotes capped expenditure. The superscript u on an expenditure variable denotes uncapped expenditure. The superscript r on a variable denotes a value for a county (the basic geographic building block for NGACO regions). The combination of the superscript r and the subscript a on a variable indicates that the variable represents a weighted average of the county-level variables using the months accrued by beneficiaries aligned with NGACO a who reside in each county r as weights. B.2 NGACO savings or loss The savings (or loss) incurred by an ACO is formally given by: where = Aggregate savings (loss) incurred by NGACO a in Performance-Year t = Capped aggregate Performance Year Benchmark expenditure of NGACO a in Performance-Year t = Capped aggregate expenditure incurred of all Next Generation Beneficiaries aligned with NGACO a in Performance-Year t NGACO Benchmarking Methods Rev. 1.02.01
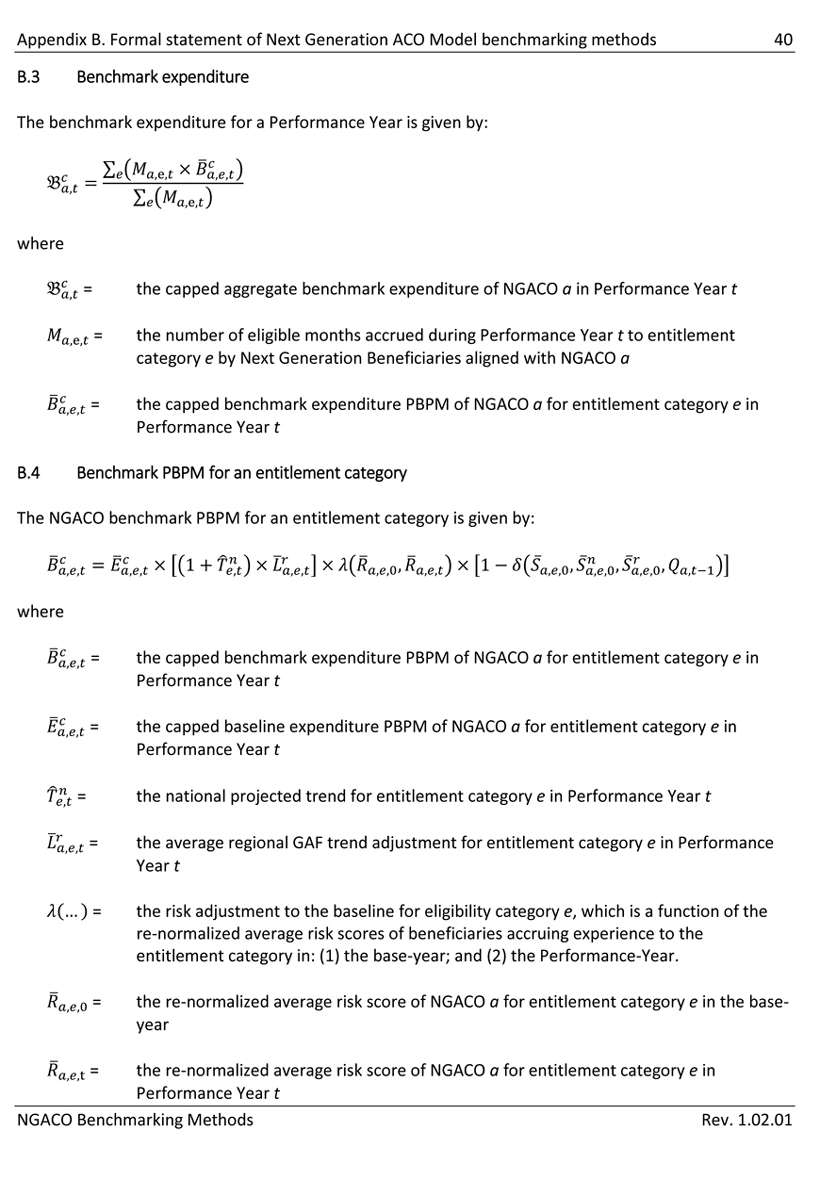
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 40 B.3 Benchmark expenditure The benchmark expenditure for a Performance Year is given by: where = the capped aggregate benchmark expenditure of NGACO a in Performance Year t ,e, = the number of eligible months accrued during Performance Year t to entitlement category e by Next Generation Beneficiaries aligned with NGACO a = the capped benchmark expenditure PBPM of NGACO a for entitlement category e in Performance Year t B.4 Benchmark PBPM for an entitlement category The NGACO benchmark PBPM for an entitlement category is given by: where = the capped benchmark expenditure PBPM of NGACO a for entitlement category e in Performance Year t = the capped baseline expenditure PBPM of NGACO a for entitlement category e in Performance Year t = the national projected trend for entitlement category e in Performance Year t = the average regional GAF trend adjustment for entitlement category e in Performance Year t (…) = the risk adjustment to the baseline for eligibility category e, which is a function of the re-normalized average risk scores of beneficiaries accruing experience to the entitlement category in: (1) the base-year; and (2) the Performance-Year. = the re-normalized average risk score of NGACO a for entitlement category e in the base- year = the re-normalized average risk score of NGACO a for entitlement category e in Performance Year t NGACO Benchmarking Methods Rev. 1.02.01
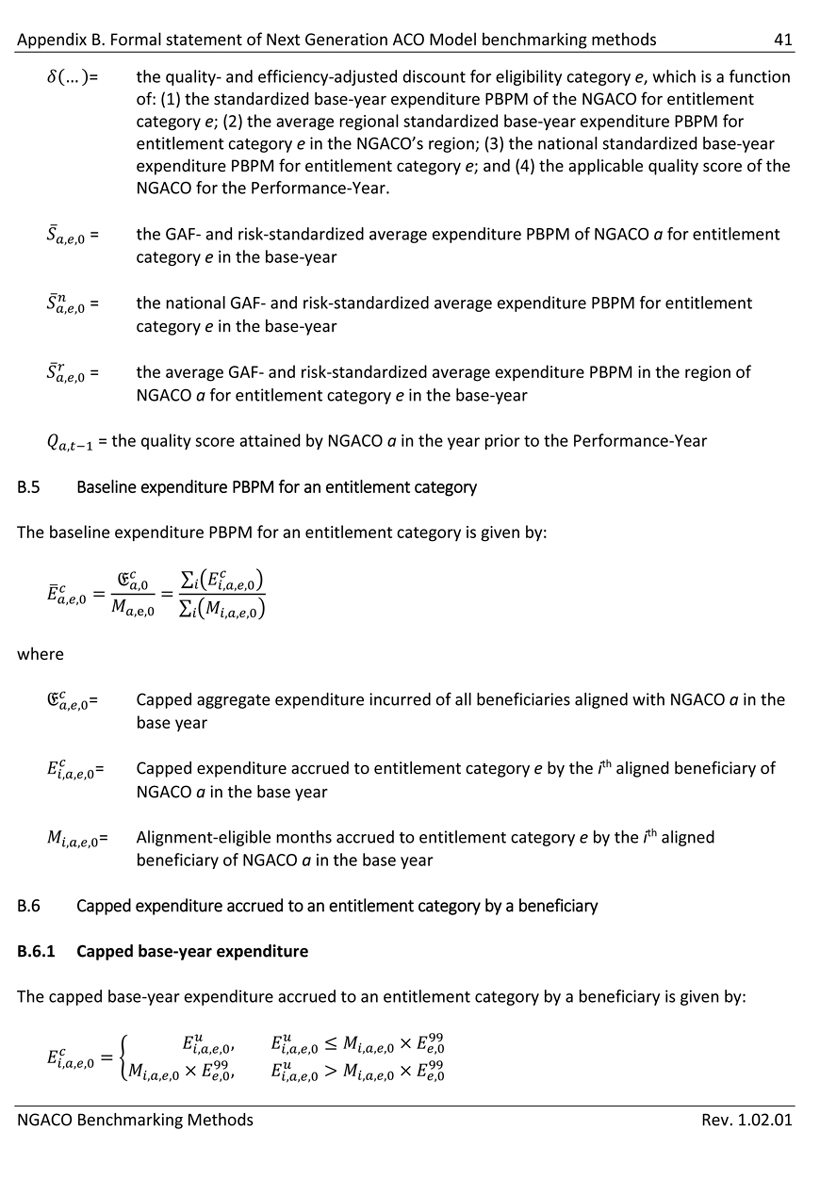
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 41 = the quality- and efficiency-adjusted discount for eligibility category e, which is a function of: (1) the standardized base-year expenditure PBPM of the NGACO for entitlement category e; (2) the average regional standardized base-year expenditure PBPM for entitlement category e in the NGACO’s region; (3) the national standardized base-year expenditure PBPM for entitlement category e; and (4) the applicable quality score of the NGACO for the Performance-Year. = the GAF- and risk-standardized average expenditure PBPM of NGACO a for entitlement category e in the base-year = the national GAF- and risk-standardized average expenditure PBPM for entitlement category e in the base-year = the average GAF- and risk-standardized average expenditure PBPM in the region of NGACO a for entitlement category e in the base-year = the quality score attained by NGACO a in the year prior to the Performance-Year B.5 Baseline expenditure PBPM for an entitlement category The baseline expenditure PBPM for an entitlement category is given by: where = Capped aggregate expenditure incurred of all beneficiaries aligned with NGACO a in the base year = Capped expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year = Alignment-eligible months accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year B.6 Capped expenditure accrued to an entitlement category by a beneficiary B.6.1 Capped base-year expenditure The capped base-year expenditure accrued to an entitlement category by a beneficiary is given by: NGACO Benchmarking Methods Rev. 1.02.01
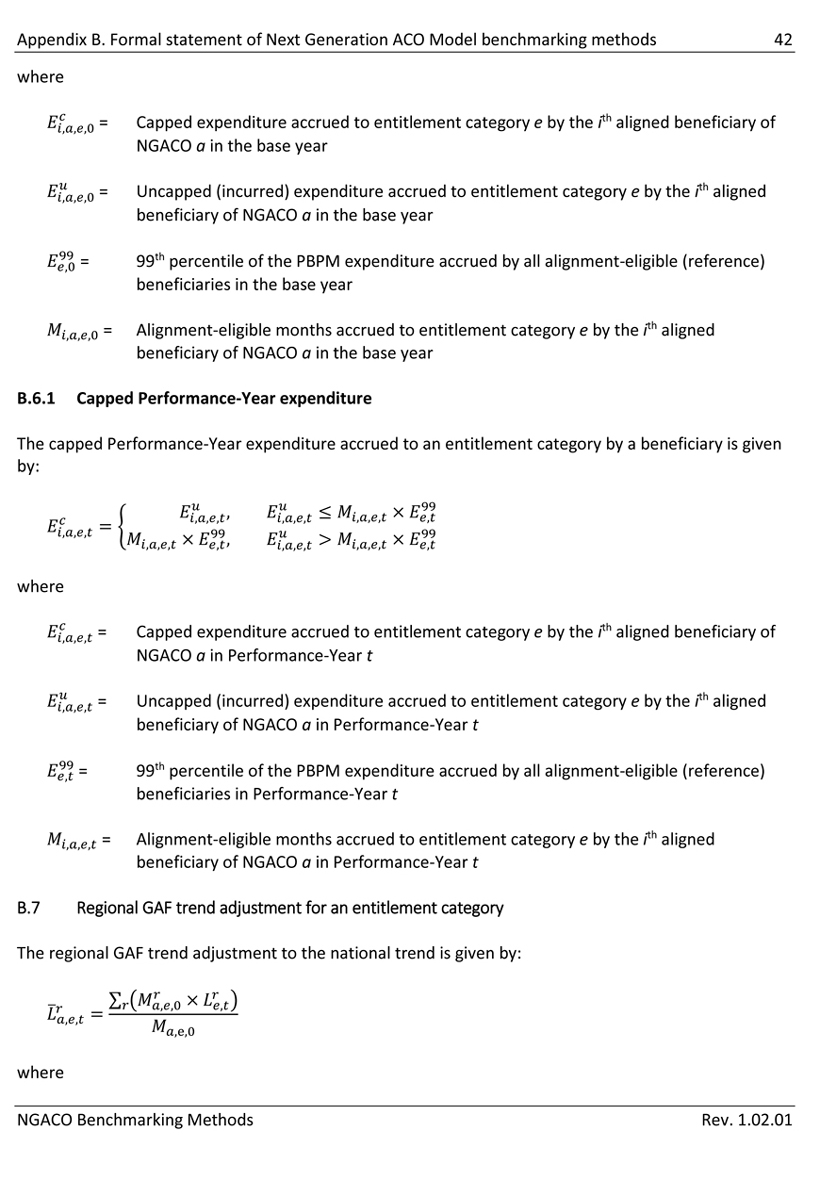
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 42 where = Capped expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year = Uncapped (incurred) expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year = 99th percentile of the PBPM expenditure accrued by all alignment-eligible (reference) beneficiaries in the base year = Alignment-eligible months accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year B.6.1 Capped Performance-Year expenditure The capped Performance-Year expenditure accrued to an entitlement category by a beneficiary is given by: where = Capped expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in Performance-Year t = Uncapped (incurred) expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in Performance-Year t = 99th percentile of the PBPM expenditure accrued by all alignment-eligible (reference) beneficiaries in Performance-Year t = Alignment-eligible months accrued to entitlement category e by the ith aligned beneficiary of NGACO a in Performance-Year t B.7 Regional GAF trend adjustment for an entitlement category The regional GAF trend adjustment to the national trend is given by: where NGACO Benchmarking Methods Rev. 1.02.01
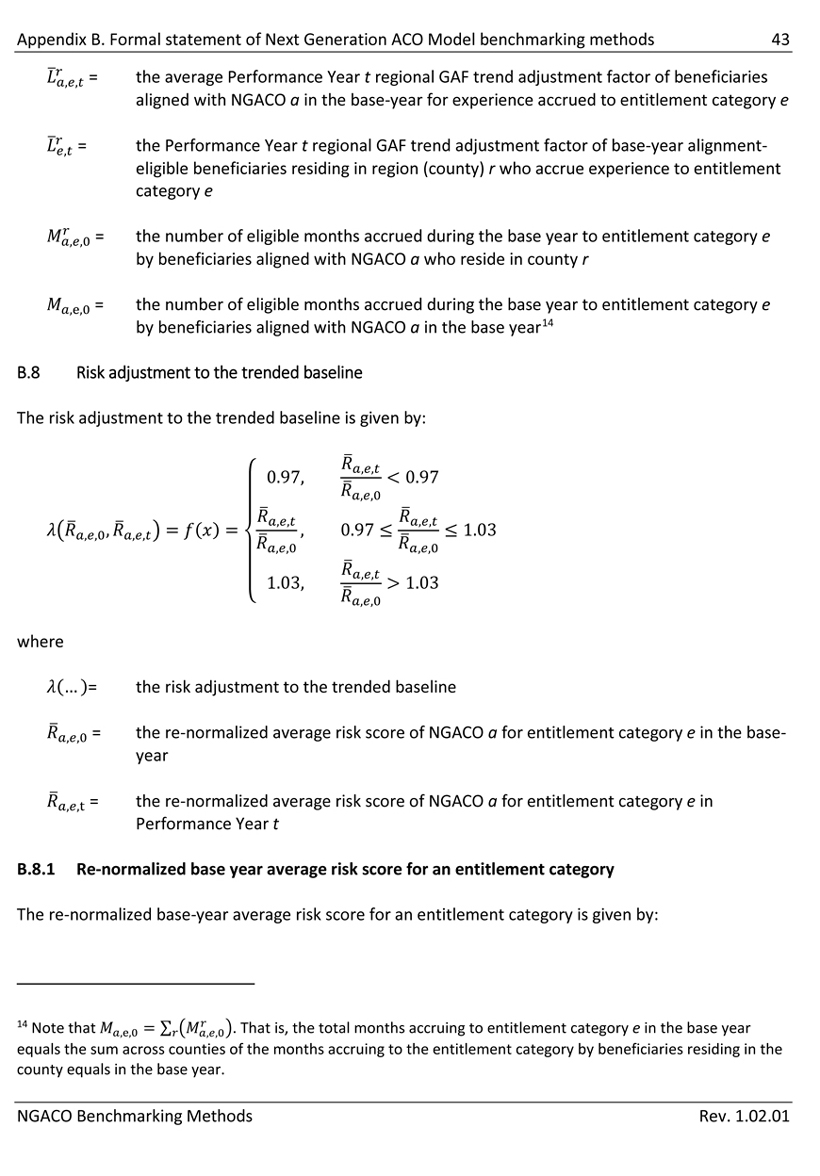
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 43 = the average Performance Year t regional GAF trend adjustment factor of beneficiaries aligned with NGACO a in the base-year for experience accrued to entitlement category e = the Performance Year t regional GAF trend adjustment factor of base-year alignment- eligible beneficiaries residing in region (county) r who accrue experience to entitlement category e = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a who reside in county r = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a in the base year14 B.8 Risk adjustment to the trended baseline The risk adjustment to the trended baseline is given by: where (…)= the risk adjustment to the trended baseline = the re-normalized average risk score of NGACO a for entitlement category e in the base- year = the re-normalized average risk score of NGACO a for entitlement category e in Performance Year t B.8.1 Re-normalized base year average risk score for an entitlement category The re-normalized base-year average risk score for an entitlement category is given by: 14 Note that. That is, the total months accruing to entitlement category e in the base year equals the sum across counties of the months accruing to the entitlement category by beneficiaries residing in the county equals in the base year. NGACO Benchmarking Methods Rev. 1.02.01
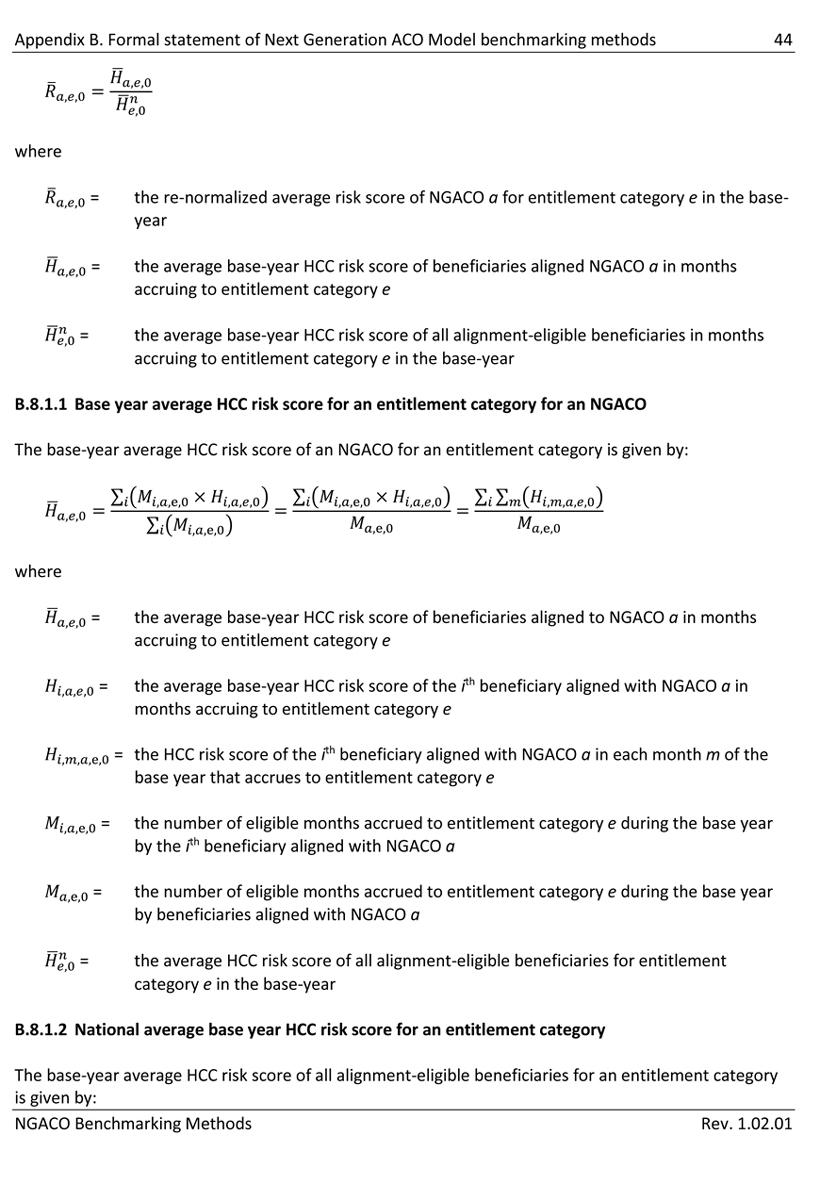
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 44 where = the re-normalized average risk score of NGACO a for entitlement category e in the base- year = the average base-year HCC risk score of beneficiaries aligned NGACO a in months accruing to entitlement category e = the average base-year HCC risk score of all alignment-eligible beneficiaries in months accruing to entitlement category e in the base-year B.8.1.1 Base year average HCC risk score for an entitlement category for an NGACO The base-year average HCC risk score of an NGACO for an entitlement category is given by: where = the average base-year HCC risk score of beneficiaries aligned to NGACO a in months accruing to entitlement category e = the average base-year HCC risk score of the ith beneficiary aligned with NGACO a in months accruing to entitlement category e = the HCC risk score of the ith beneficiary aligned with NGACO a in each month m of the base year that accrues to entitlement category e = the number of eligible months accrued to entitlement category e during the base year by the ith beneficiary aligned with NGACO a = the number of eligible months accrued to entitlement category e during the base year by beneficiaries aligned with NGACO a = the average HCC risk score of all alignment-eligible beneficiaries for entitlement category e in the base-year B.8.1.2 National average base year HCC risk score for an entitlement category The base-year average HCC risk score of all alignment-eligible beneficiaries for an entitlement category is given by: NGACO Benchmarking Methods Rev. 1.02.01
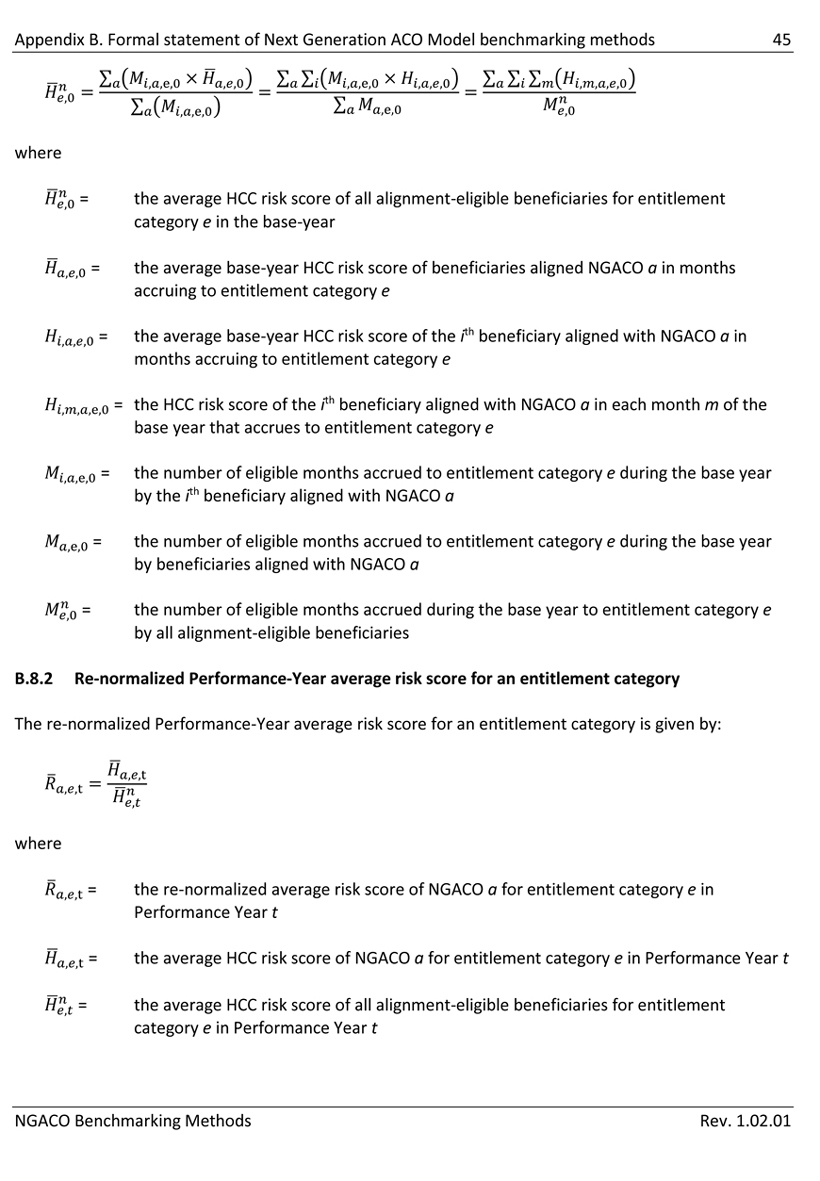
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 45 where = the average HCC risk score of all alignment-eligible beneficiaries for entitlement category e in the base-year = the average base-year HCC risk score of beneficiaries aligned NGACO a in months accruing to entitlement category e = the average base-year HCC risk score of the ith beneficiary aligned with NGACO a in months accruing to entitlement category e = the HCC risk score of the ith beneficiary aligned with NGACO a in each month m of the base year that accrues to entitlement category e = the number of eligible months accrued to entitlement category e during the base year by the ith beneficiary aligned with NGACO a = the number of eligible months accrued to entitlement category e during the base year by beneficiaries aligned with NGACO a = the number of eligible months accrued during the base year to entitlement category e by all alignment-eligible beneficiaries B.8.2 Re-normalized Performance-Year average risk score for an entitlement category The re-normalized Performance-Year average risk score for an entitlement category is given by: where = the re-normalized average risk score of NGACO a for entitlement category e in Performance Year t = the average HCC risk score of NGACO a for entitlement category e in Performance Year t = the average HCC risk score of all alignment-eligible beneficiaries for entitlement category e in Performance Year t NGACO Benchmarking Methods Rev. 1.02.01
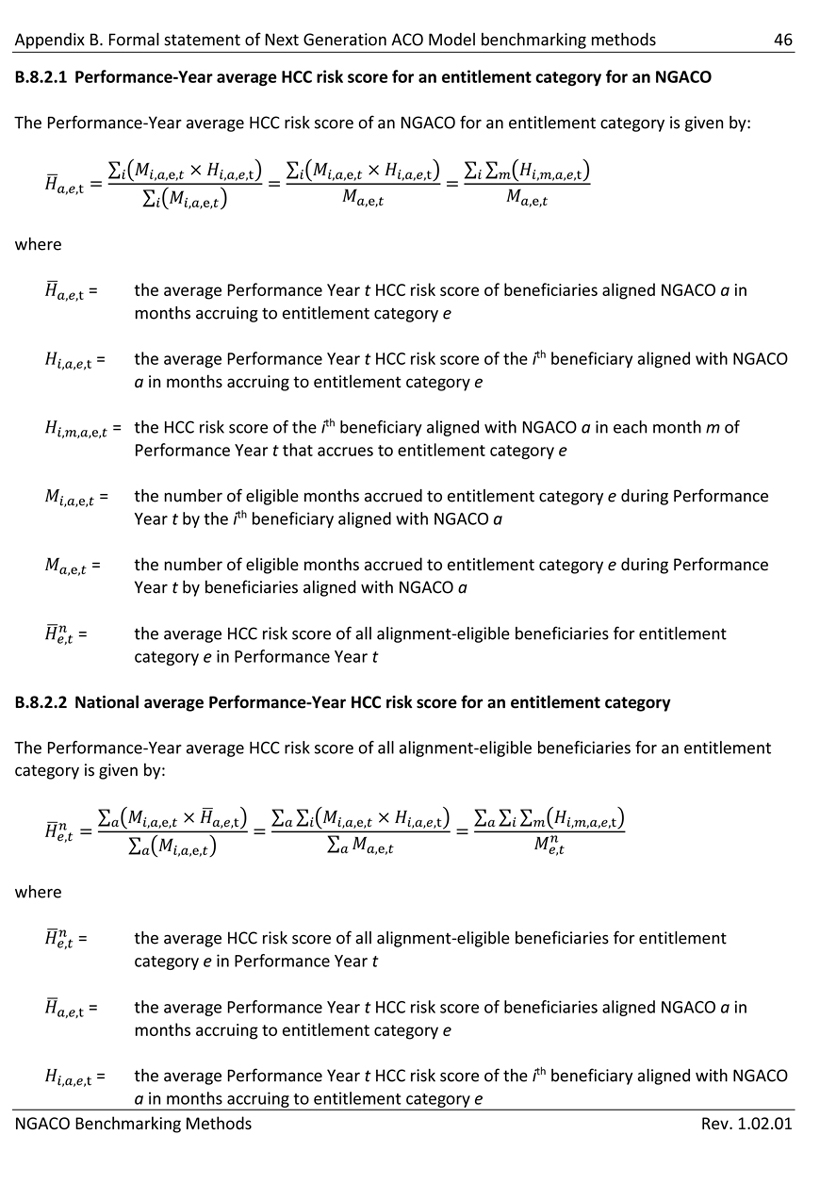
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 46 B.8.2.1 Performance-Year average HCC risk score for an entitlement category for an NGACO The Performance-Year average HCC risk score of an NGACO for an entitlement category is given by: where = the average Performance Year t HCC risk score of beneficiaries aligned NGACO a in months accruing to entitlement category e = the average Performance Year t HCC risk score of the ith beneficiary aligned with NGACO a in months accruing to entitlement category e = the HCC risk score of the ith beneficiary aligned with NGACO a in each month m of Performance Year t that accrues to entitlement category e = the number of eligible months accrued to entitlement category e during Performance Year t by the ith beneficiary aligned with NGACO a = the number of eligible months accrued to entitlement category e during Performance Year t by beneficiaries aligned with NGACO a = the average HCC risk score of all alignment-eligible beneficiaries for entitlement category e in Performance Year t B.8.2.2 National average Performance-Year HCC risk score for an entitlement category The Performance-Year average HCC risk score of all alignment-eligible beneficiaries for an entitlement category is given by: where = the average HCC risk score of all alignment-eligible beneficiaries for entitlement category e in Performance Year t = the average Performance Year t HCC risk score of beneficiaries aligned NGACO a in months accruing to entitlement category e = the average Performance Year t HCC risk score of the ith beneficiary aligned with NGACO a in months accruing to entitlement category e NGACO Benchmarking Methods Rev. 1.02.01
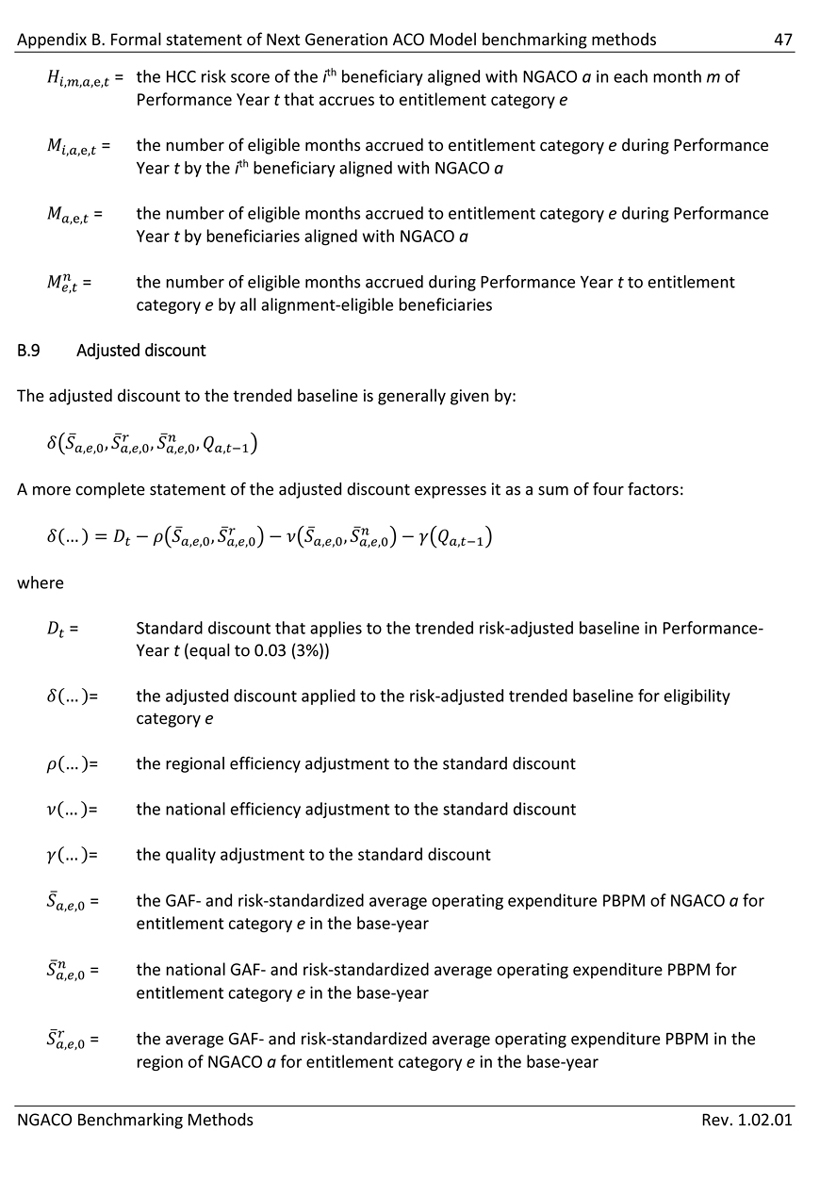
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 47 = the HCC risk score of the ith beneficiary aligned with NGACO a in each month m of Performance Year t that accrues to entitlement category e = the number of eligible months accrued to entitlement category e during Performance Year t by the ith beneficiary aligned with NGACO a = the number of eligible months accrued to entitlement category e during Performance Year t by beneficiaries aligned with NGACO a = the number of eligible months accrued during Performance Year t to entitlement category e by all alignment-eligible beneficiaries B.9 Adjusted discount The adjusted discount to the trended baseline is generally given by: A more complete statement of the adjusted discount expresses it as a sum of four factors: where = Standard discount that applies to the trended risk-adjusted baseline in Performance- Year t (equal to 0.03 (3%)) = the adjusted discount applied to the risk-adjusted trended baseline for eligibility category e = the regional efficiency adjustment to the standard discount = the national efficiency adjustment to the standard discount = the quality adjustment to the standard discount = the GAF- and risk-standardized average operating expenditure PBPM of NGACO a for entitlement category e in the base-year = the national GAF- and risk-standardized average operating expenditure PBPM for entitlement category e in the base-year = the average GAF- and risk-standardized average operating expenditure PBPM in the region of NGACO a for entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
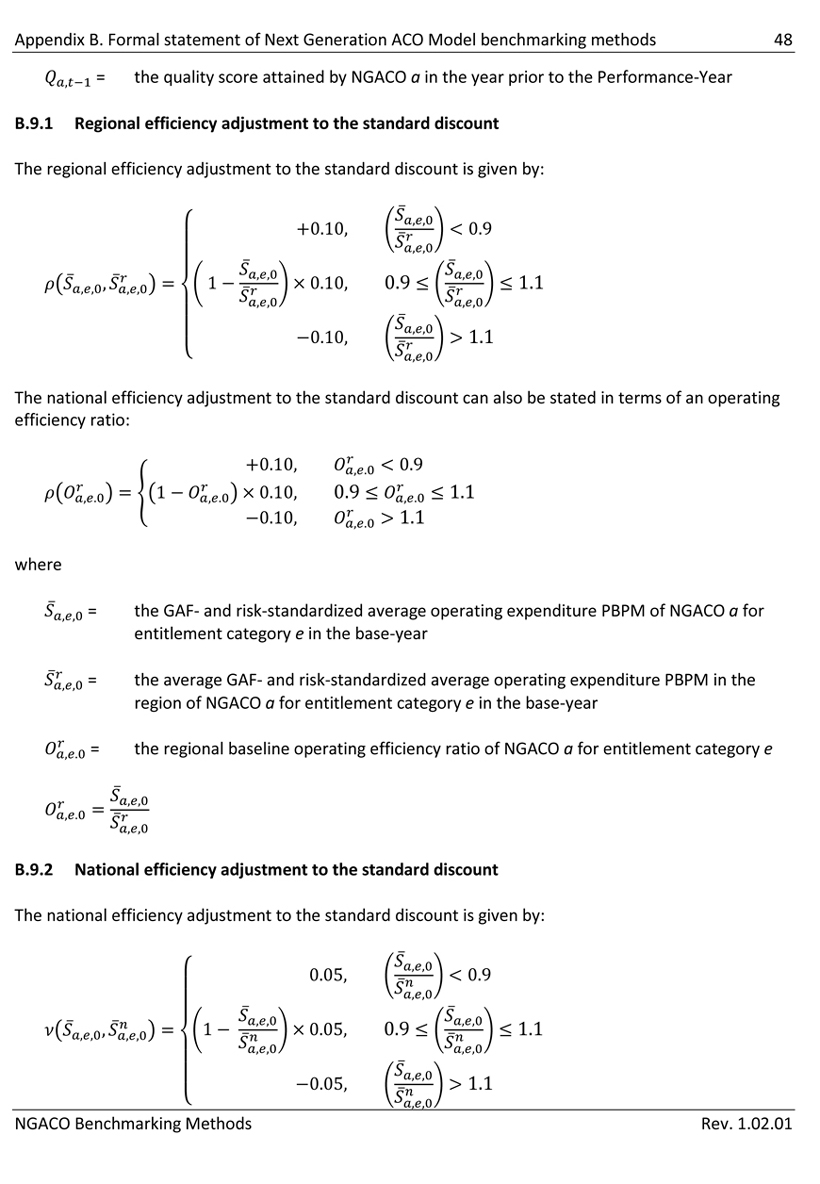
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 48 = the quality score attained by NGACO a in the year prior to the Performance-Year B.9.1 Regional efficiency adjustment to the standard discount The regional efficiency adjustment to the standard discount is given by: The national efficiency adjustment to the standard discount can also be stated in terms of an operating efficiency ratio: where = the GAF- and risk-standardized average operating expenditure PBPM of NGACO a for entitlement category e in the base-year = the average GAF- and risk-standardized average operating expenditure PBPM in the region of NGACO a for entitlement category e in the base-year = the regional baseline operating efficiency ratio of NGACO a for entitlement category e B.9.2 National efficiency adjustment to the standard discount The national efficiency adjustment to the standard discount is given by: NGACO Benchmarking Methods Rev. 1.02.01
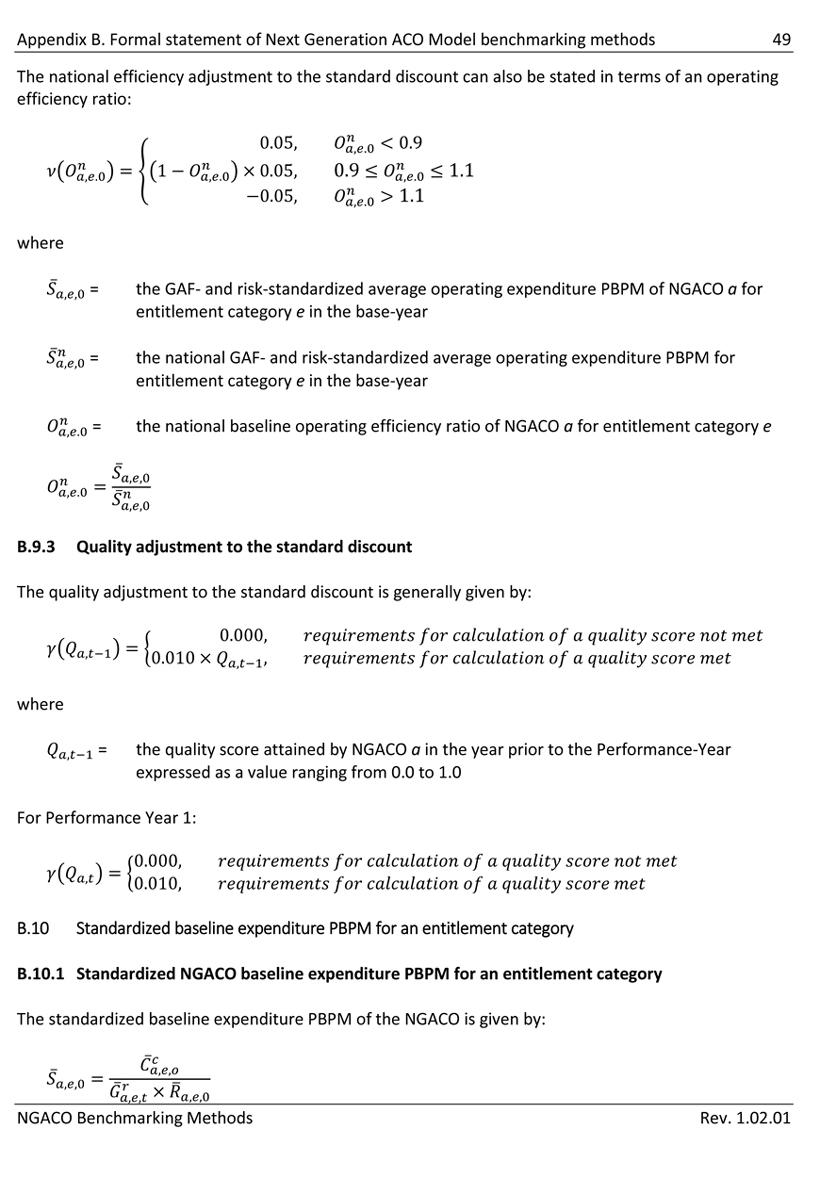
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 49 The national efficiency adjustment to the standard discount can also be stated in terms of an operating efficiency ratio: where = the GAF- and risk-standardized average operating expenditure PBPM of NGACO a for entitlement category e in the base-year = the national GAF- and risk-standardized average operating expenditure PBPM for entitlement category e in the base-year = the national baseline operating efficiency ratio of NGACO a for entitlement category e B.9.3 Quality adjustment to the standard discount The quality adjustment to the standard discount is generally given by: where = the quality score attained by NGACO a in the year prior to the Performance-Year expressed as a value ranging from 0.0 to 1.0 For Performance Year 1: B.10 Standardized baseline expenditure PBPM for an entitlement category B.10.1 Standardized NGACO baseline expenditure PBPM for an entitlement category The standardized baseline expenditure PBPM of the NGACO is given by: NGACO Benchmarking Methods Rev. 1.02.01
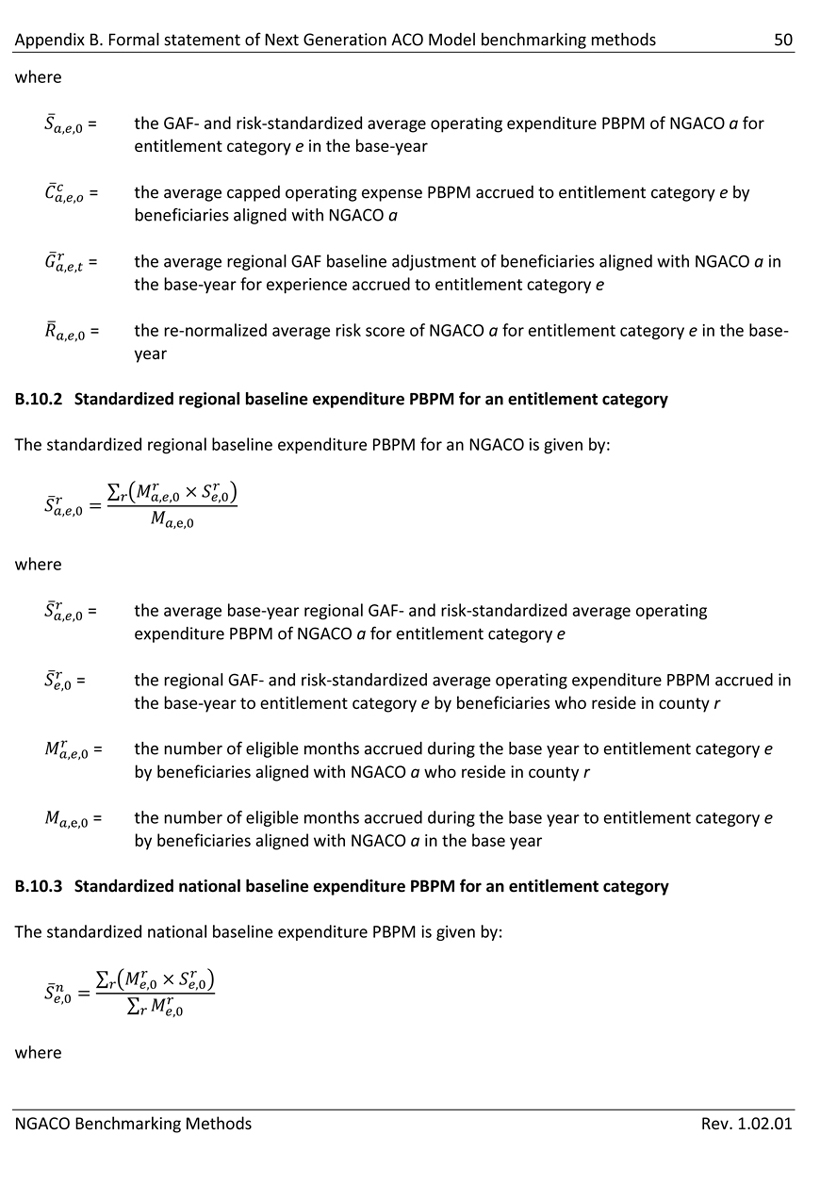
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 50 where = the GAF- and risk-standardized average operating expenditure PBPM of NGACO a for entitlement category e in the base-year = the average capped operating expense PBPM accrued to entitlement category e by beneficiaries aligned with NGACO a = the average regional GAF baseline adjustment of beneficiaries aligned with NGACO a in the base-year for experience accrued to entitlement category e = the re-normalized average risk score of NGACO a for entitlement category e in the base- year B.10.2 Standardized regional baseline expenditure PBPM for an entitlement category The standardized regional baseline expenditure PBPM for an NGACO is given by: where = the average base-year regional GAF- and risk-standardized average operating expenditure PBPM of NGACO a for entitlement category e = the regional GAF- and risk-standardized average operating expenditure PBPM accrued in the base-year to entitlement category e by beneficiaries who reside in county r = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a who reside in county r = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a in the base year B.10.3 Standardized national baseline expenditure PBPM for an entitlement category The standardized national baseline expenditure PBPM is given by: where NGACO Benchmarking Methods Rev. 1.02.01
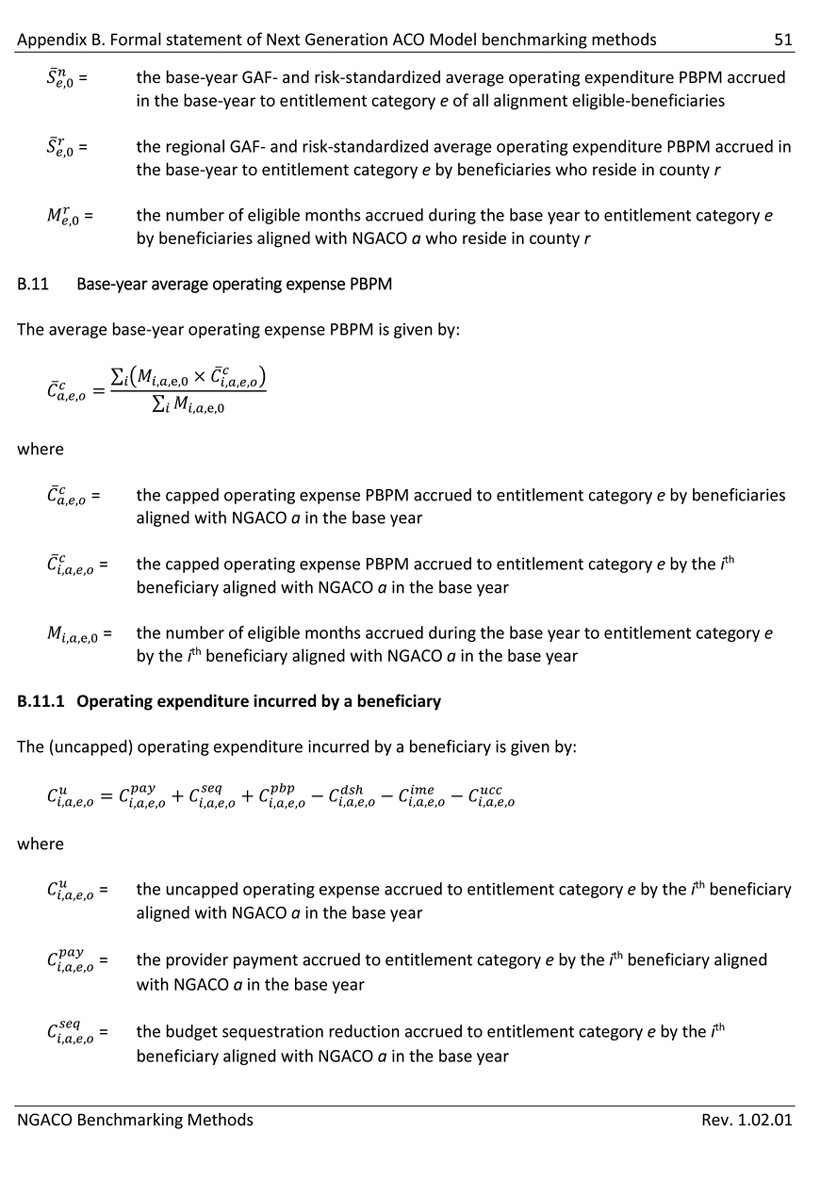
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 51 = the base-year GAF- and risk-standardized average operating expenditure PBPM accrued in the base-year to entitlement category e of all alignment eligible-beneficiaries = the regional GAF- and risk-standardized average operating expenditure PBPM accrued in the base-year to entitlement category e by beneficiaries who reside in county r = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a who reside in county r B.11 Base-year average operating expense PBPM The average base-year operating expense PBPM is given by: where = the capped operating expense PBPM accrued to entitlement category e by beneficiaries aligned with NGACO a in the base year = the capped operating expense PBPM accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the number of eligible months accrued during the base year to entitlement category e by the ith beneficiary aligned with NGACO a in the base year B.11.1 Operating expenditure incurred by a beneficiary The (uncapped) operating expenditure incurred by a beneficiary is given by: where = the uncapped operating expense accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the provider payment accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the budget sequestration reduction accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year NGACO Benchmarking Methods Rev. 1.02.01
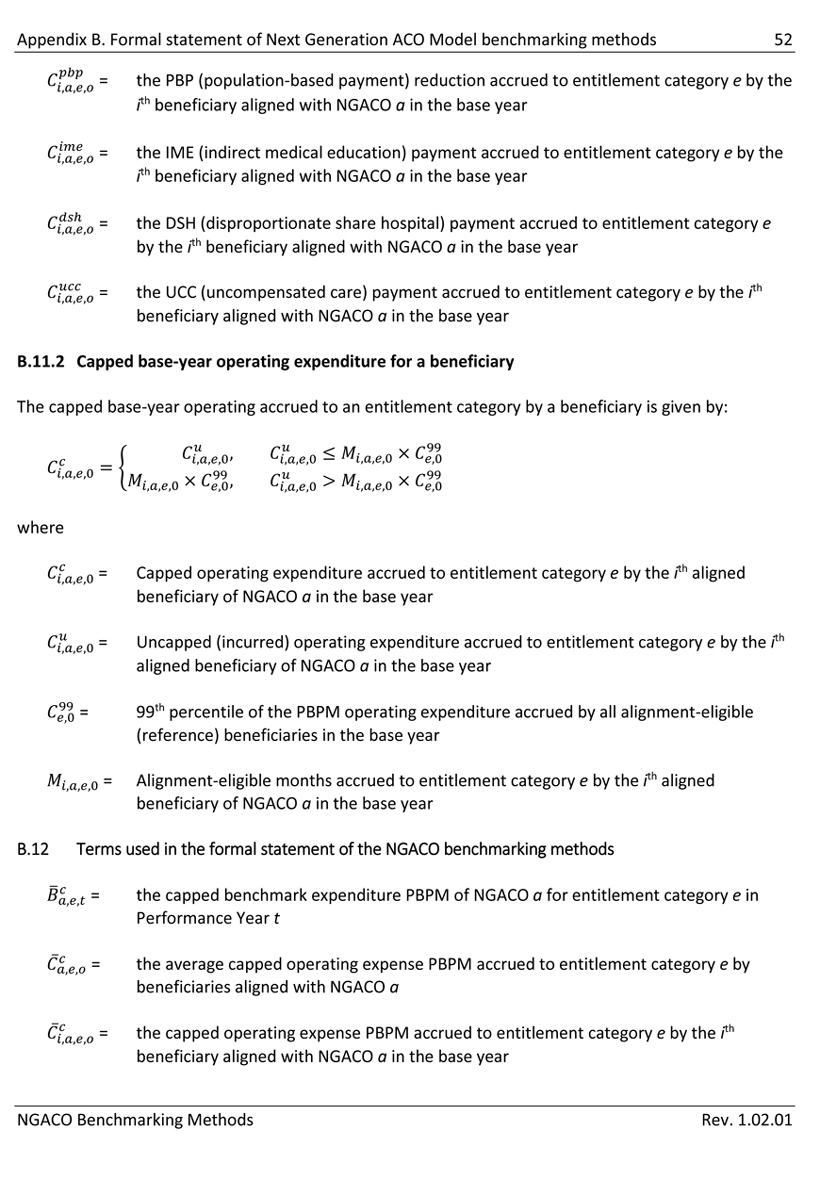
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 52 = the PBP (population-based payment) reduction accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the IME (indirect medical education) payment accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the DSH (disproportionate share hospital) payment accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the UCC (uncompensated care) payment accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year B.11.2 Capped base-year operating expenditure for a beneficiary The capped base-year operating accrued to an entitlement category by a beneficiary is given by: where = Capped operating expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year = Uncapped (incurred) operating expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year = 99th percentile of the PBPM operating expenditure accrued by all alignment-eligible (reference) beneficiaries in the base year = Alignment-eligible months accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year B.12 Terms used in the formal statement of the NGACO benchmarking methods = the capped benchmark expenditure PBPM of NGACO a for entitlement category e in Performance Year t = the average capped operating expense PBPM accrued to entitlement category e by beneficiaries aligned with NGACO a = the capped operating expense PBPM accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year NGACO Benchmarking Methods Rev. 1.02.01
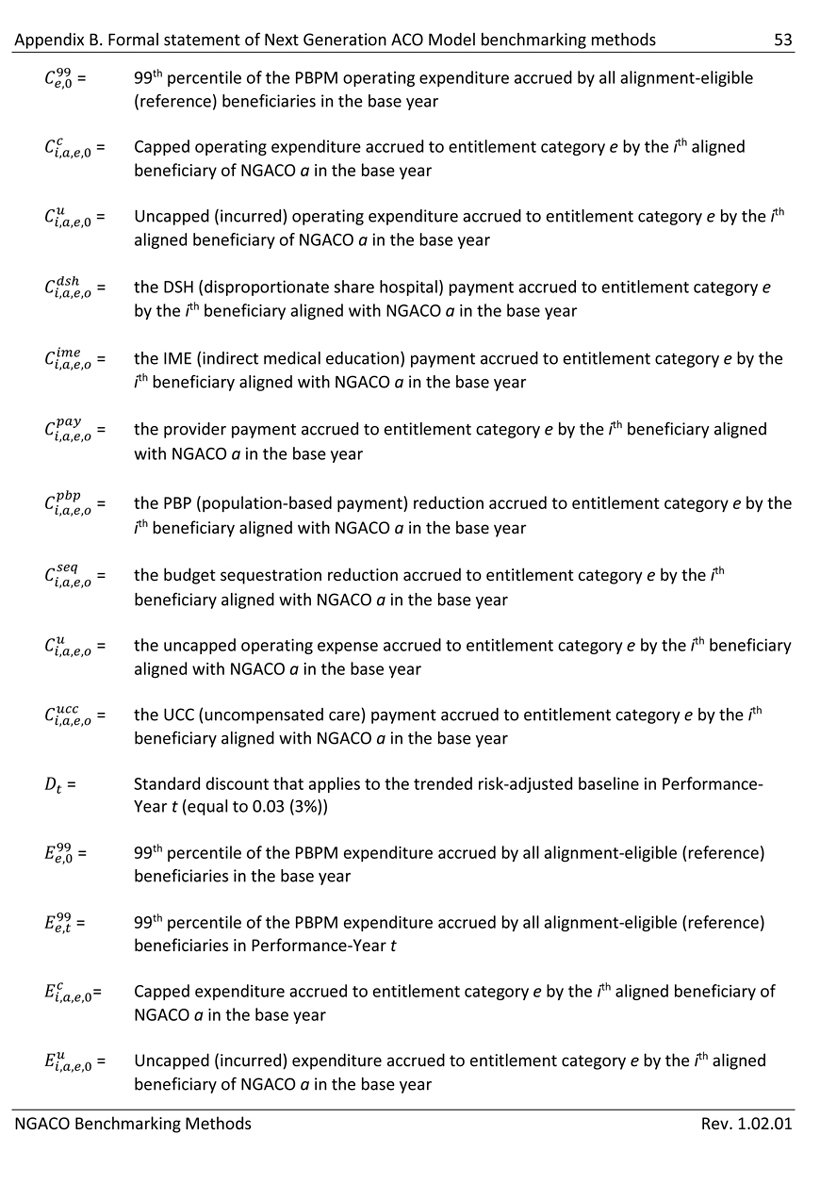
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 53 = 99th percentile of the PBPM operating expenditure accrued by all alignment-eligible (reference) beneficiaries in the base year = Capped operating expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year = Uncapped (incurred) operating expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year = the DSH (disproportionate share hospital) payment accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the IME (indirect medical education) payment accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the provider payment accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the PBP (population-based payment) reduction accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the budget sequestration reduction accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the uncapped operating expense accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the UCC (uncompensated care) payment accrued to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = Standard discount that applies to the trended risk-adjusted baseline in Performance- Year t (equal to 0.03 (3%)) = 99th percentile of the PBPM expenditure accrued by all alignment-eligible (reference) beneficiaries in the base year = 99th percentile of the PBPM expenditure accrued by all alignment-eligible (reference) beneficiaries in Performance-Year t = Capped expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year = Uncapped (incurred) expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in the base year NGACO Benchmarking Methods Rev. 1.02.01
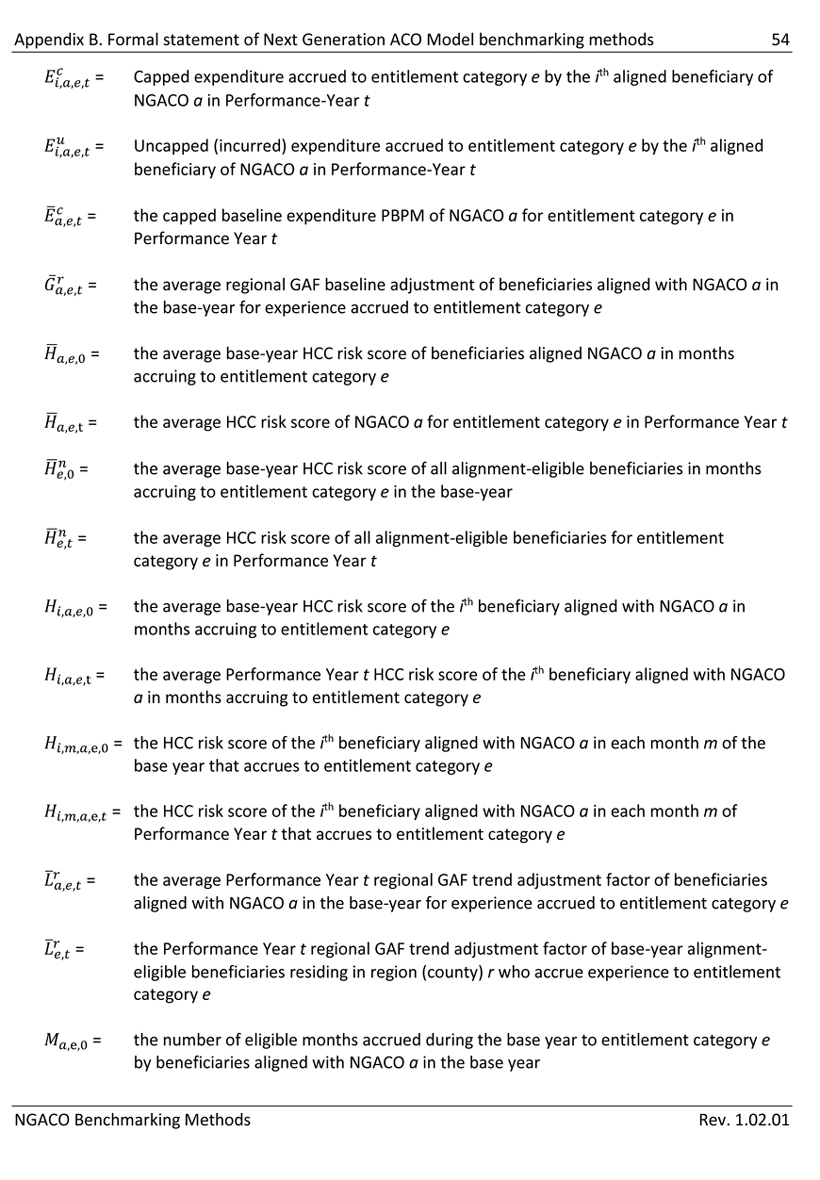
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 54 = Capped expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in Performance-Year t = Uncapped (incurred) expenditure accrued to entitlement category e by the ith aligned beneficiary of NGACO a in Performance-Year t = the capped baseline expenditure PBPM of NGACO a for entitlement category e in Performance Year t = the average regional GAF baseline adjustment of beneficiaries aligned with NGACO a in the base-year for experience accrued to entitlement category e = the average base-year HCC risk score of beneficiaries aligned NGACO a in months accruing to entitlement category e = the average HCC risk score of NGACO a for entitlement category e in Performance Year t = the average base-year HCC risk score of all alignment-eligible beneficiaries in months accruing to entitlement category e in the base-year = the average HCC risk score of all alignment-eligible beneficiaries for entitlement category e in Performance Year t = the average base-year HCC risk score of the ith beneficiary aligned with NGACO a in months accruing to entitlement category e = the average Performance Year t HCC risk score of the ith beneficiary aligned with NGACO a in months accruing to entitlement category e = the HCC risk score of the ith beneficiary aligned with NGACO a in each month m of the base year that accrues to entitlement category e = the HCC risk score of the ith beneficiary aligned with NGACO a in each month m of Performance Year t that accrues to entitlement category e = the average Performance Year t regional GAF trend adjustment factor of beneficiaries aligned with NGACO a in the base-year for experience accrued to entitlement category e = the Performance Year t regional GAF trend adjustment factor of base-year alignment- eligible beneficiaries residing in region (county) r who accrue experience to entitlement category e = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a in the base year NGACO Benchmarking Methods Rev. 1.02.01
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 55 = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a in the base year = the number of eligible months accrued during Performance Year t to entitlement category e by beneficiaries aligned with NGACO a = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a who reside in county r = the number of eligible months accrued during the base year to entitlement category e by all alignment-eligible beneficiaries = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a who reside in county r = the number of eligible months accrued during Performance Year t to entitlement category e by all alignment-eligible beneficiaries = the number of eligible months accrued during the base year to entitlement category e by the ith beneficiary aligned with NGACO a in the base year = the number of eligible months accrued to entitlement category e during Performance Year t by the ith beneficiary aligned with NGACO a = Alignment-eligible months accrued to entitlement category e by the ith aligned beneficiary of NGACO a in Performance-Year t = the national baseline operating efficiency ratio of NGACO a for entitlement category e = the regional baseline operating efficiency ratio of NGACO a for entitlement category e = the quality score attained by NGACO a in the year prior to the Performance-Year = the quality score attained by NGACO a in the 2nd year prior to the Performance-Year = the re-normalized average risk score of NGACO a for entitlement category e in the base- year = the re-normalized average risk score of NGACO a for entitlement category e in Performance Year t = the GAF- and risk-standardized average expenditure PBPM of NGACO a for entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
Appendix B. Formal statement of Next Generation ACO Model benchmarking methods 56 = the national GAF- and risk-standardized average expenditure PBPM for entitlement category e in the base-year = the average base-year regional GAF- and risk-standardized average operating expenditure PBPM of NGACO a for entitlement category e = the base-year GAF- and risk-standardized average operating expenditure PBPM accrued in the base-year to entitlement category e of all alignment eligible-beneficiaries = the regional GAF- and risk-standardized average operating expenditure PBPM accrued in the base-year to entitlement category e by beneficiaries who reside in county r = the national projected trend for entitlement category e in Performance Year t = the capped aggregate benchmark expenditure of NGACO a in Performance Year t = Capped aggregate benchmark expenditure of NGACO a in Performance-Year t = Capped aggregate expenditure incurred of all beneficiaries aligned with NGACO a in the base year = Capped aggregate expenditure incurred of all beneficiaries aligned with NGACO a in Performance-Year t = Aggregate savings (loss) incurred by NGACO a in Performance-Year t = the quality adjustment to the standard discount = the adjusted discount applied to the risk-adjusted trended baseline for eligibility category e = the risk adjustment to the trended baseline = the national efficiency adjustment to the standard discount = the regional efficiency adjustment to the standard discount NGACO Benchmarking Methods Rev. 1.02.01
| Appendix C. Technical description of the GAF trend adjustment | 57 |
Appendix C. Technical description of the GAF trend adjustment
Provider payments under most Medicare fee-for-service (FFS) payment systems reflect an adjustment for the cost-of-doing business in the local geographic area in which the provider is located.15 These geographic adjustment factors (GAFs) are updated annually. The purpose of the GAF trend adjustment in the NGACO Model is to prevent the benchmark from being unfairly understated (or overstated) because of differences between the GAFs that Medicare used to calculate provider payments in the base-year (CY2014) and the Performance-Year.
| C.1 | Overview of the GAF trend adjustment |
The GAF trend adjustment factor is a county-level adjustment. The GAF trend adjustment factor for a county is an estimate of the impact of the Performance Year Medicare GAFs on the base-year provider payments for services provided to reference beneficiaries residing in the county. That is, the GAF trend adjustment is an estimate of the amount by which the base-year expenditure of residents of a county would have increased or decreased if the Performance-Year GAFs had been used to calculate provider payments.
The GAF trend adjustment factor for a county will be the ratio of:
| 3. | The base year expenditure16 incurred by residents of a county adjusted to reflect the impact on provider payments of the geographic pricing factors that Medicare will use in the Performance Year; to, |
| 4. | The actual expenditure incurred by residents of a county, which reflects the geographic pricing factors that Medicare used to calculate provider payments in the base year. |
The GAF-trend adjustment factor will be calculated prospectively for alignment-eligible beneficiaries in each county in the base year and will have no impact on the national FFS trend.17
The GAF trend-adjustment for an ACO will be the person-month weighted average of county GAF-trend adjustment factors, where the weights are the ACO aligned beneficiary person months residing in each county.
15 Examples of these Geographic Adjustment Factors (GAFs) are the Medicare area wage index (AWI) and the geographic practice cost index (GPCI).
16 The GAF adjustment is the ratio of: (1) the aggregate normalized or budget-neutral GAF-adjusted provider payment; to (2) the aggregate unadjusted provider payment. It is not necessary to convert the aggregate provider payment to a PBPM amount.
17 The GAF-trend adjustment will be calculated on a budget-neutral basis so that the regional trend adjustments neither increase nor decrease the total expenditure of the reference population nationally. That is the adjusted claim amount for the reference population will equal the incurred claim amount.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
Appendix C. Technical description of the GAF trend adjustment 58 C.1.1 GAF-adjustable claims All claims will be included in the calculation of the GAF trend-trend adjustment. Only the following classes of claims will be adjusted to reflect the impact of the Performance-Year GAFs on base-year expenditures: 1. Claims paid under the Inpatient Prospective Payment System (IPPS); 2. Claims paid under the Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS); 3. Claims paid under the Long-term Care Hospital Prospective Payment System (LTCH PPS); 4. Claims paid under the Skilled Nursing Facility Prospective Payment System (SNF PPS); 5. Claims paid under the Home Health Prospective Payment System (HH PPS); 6. Claims paid under the Hospice Per-diem Payment System (Hospice PDPS); 7. Claims paid under the Hospital Outpatient Prospective Payment System (OPPS); 8. Claims paid under the ESRD Prospective Payment System (ESRD PPS); and, 9. Claims paid under the Physician Fee Schedule (PFS). For claims that do not belong to these classes, the “GAF-adjusted” payment amount will be equal to the incurred (actual) payment amount. C.1.2 Attribution of expenditures to counties The GAF trend-adjusted base-year expenditure for a county is an estimate of the expenditure that would have been incurred in the base-year for claims that are subject to the GAF trend-adjustment and for which the GAF trend-adjustment can be calculated by beneficiaries residing in the county in January of the base-year18 if provider payment had been calculated using the GAFs that were used in the Performance-Year. C.2 Regional GAF trend adjustment factor for an NGACO An NGACO’s regional GAF trend adjustment to the national trend for an entitlement category is given by: ,, ,,0 , = ,,0 ,,e,0,e,0 where = the average Performance Year t regional GAF trend adjustment factor of beneficiaries aligned with NGACO a in the base-year for experience accrued to entitlement category e 18 Expenditures accrue to the county in which the beneficiary resided in January of the base-year. NGACO Benchmarking Methods Rev. 1.02.01
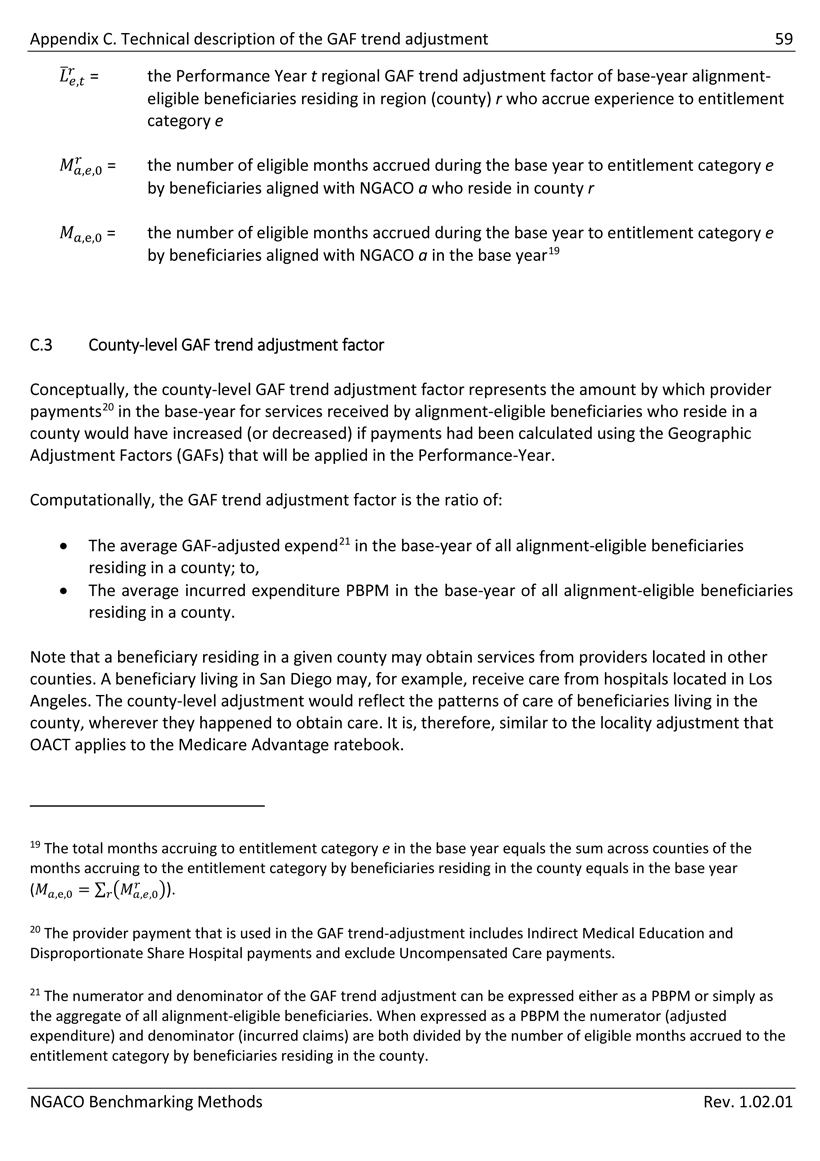
Appendix C. Technical description of the GAF trend adjustment 59 = the Performance Year t regional GAF trend adjustment factor of base-year alignment- eligible beneficiaries residing in region (county) r who accrue experience to entitlement category e = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a who reside in county r ,e,0 = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a in the base year19 C.3 County-level GAF trend adjustment factor Conceptually, the county-level GAF trend adjustment factor represents the amount by which provider payments20 in the base-year for services received by alignment-eligible beneficiaries who reside in a county would have increased (or decreased) if payments had been calculated using the Geographic Adjustment Factors (GAFs) that will be applied in the Performance-Year. Computationally, the GAF trend adjustment factor is the ratio of: • The average GAF-adjusted expend21 in the base-year of all alignment-eligible beneficiaries residing in a county; to, • The average incurred expenditure PBPM in the base-year of all alignment-eligible beneficiaries residing in a county. Note that a beneficiary residing in a given county may obtain services from providers located in other counties. A beneficiary living in San Diego may, for example, receive care from hospitals located in Los Angeles. The county-level adjustment would reflect the patterns of care of beneficiaries living in the county, wherever they happened to obtain care. It is, therefore, similar to the locality adjustment that OACT applies to the Medicare Advantage ratebook. 19 The total months accruing to entitlement category e in the base year equals the sum across counties of the months accruing to the entitlement category by beneficiaries residing in the county equals in the base year (,e,0 = ). 20 The provider payment that is used in the GAF trend-adjustment includes Indirect Medical Education and Disproportionate Share Hospital payments and exclude Uncompensated Care payments. 21 The numerator and denominator of the GAF trend adjustment can be expressed either as a PBPM or simply as the aggregate of all alignment-eligible beneficiaries. When expressed as a PBPM the numerator (adjusted expenditure) and denominator (incurred claims) are both divided by the number of eligible months accrued to the entitlement category by beneficiaries residing in the county. NGACO Benchmarking Methods Rev. 1.02.01
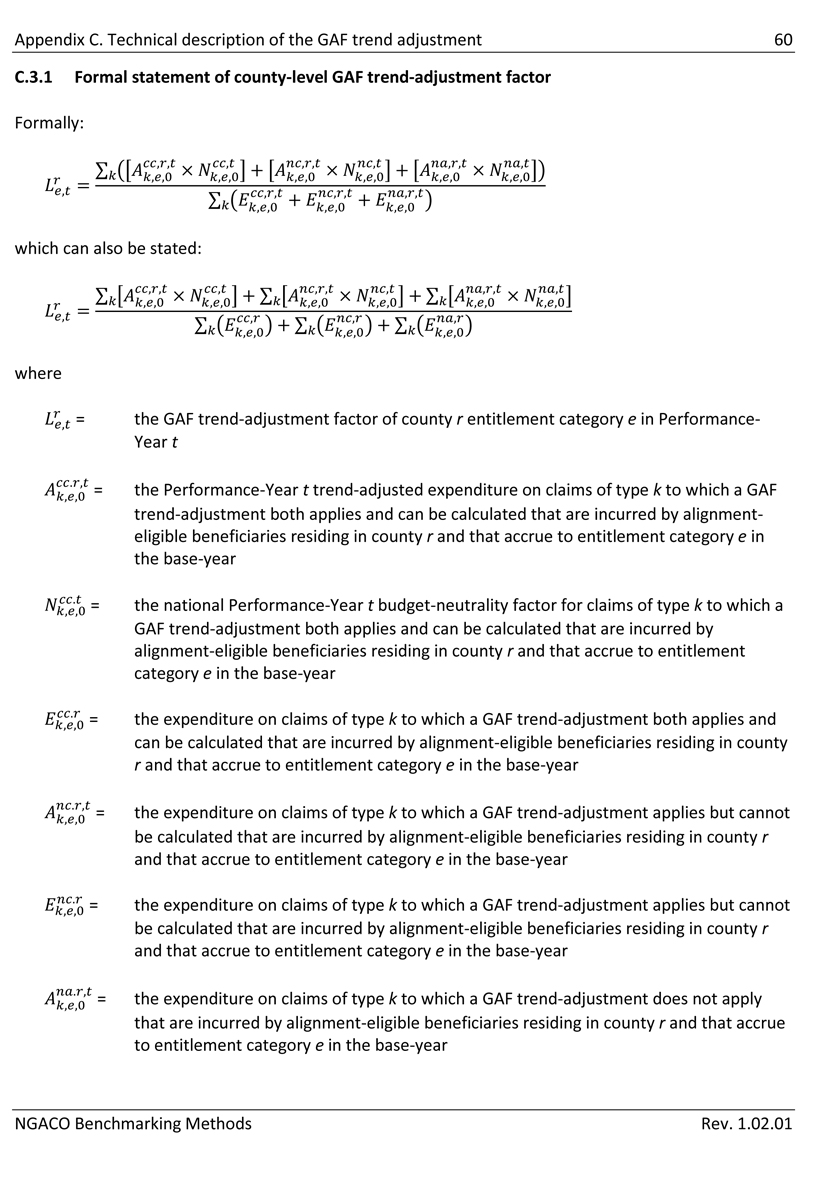
Appendix C. Technical description of the GAF trend adjustment 60 C.3.1 Formal statement of county-level GAF trend-adjustment factor Formally: which can also be stated: where = the GAF trend-adjustment factor of county r entitlement category e in Performance- Year t = the Performance-Year t trend-adjusted expenditure on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by alignment- eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the national Performance-Year t budget-neutrality factor for claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the expenditure on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the expenditure on claims of type k to which a GAF trend-adjustment applies but cannot be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the expenditure on claims of type k to which a GAF trend-adjustment applies but cannot be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the expenditure on claims of type k to which a GAF trend-adjustment does not apply that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
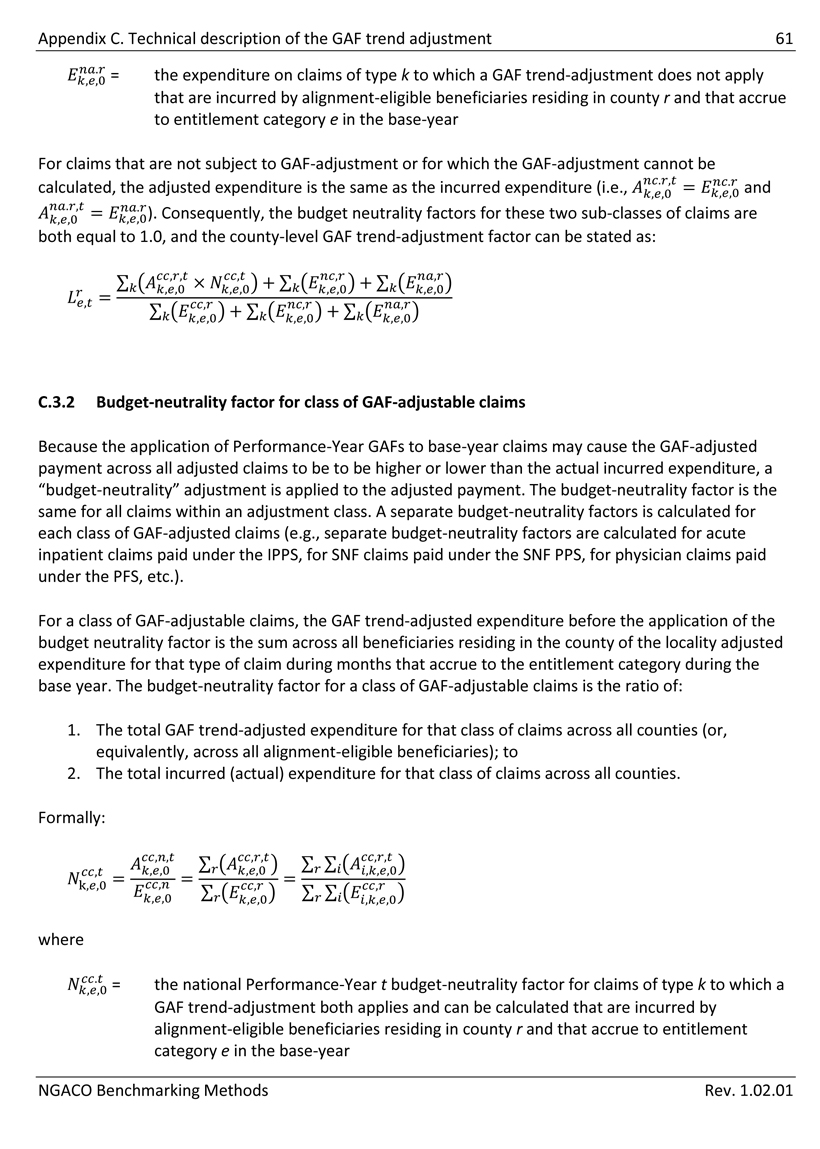
Appendix C. Technical description of the GAF trend adjustment 61 = the expenditure on claims of type k to which a GAF trend-adjustment does not apply that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year For claims that are not subject to GAF-adjustment or for which the GAF-adjustment cannot be calculated, the adjusted expenditure is the same as the incurred expenditure (i.e., =). Consequently, the budget neutrality factors for these two sub-classes of claims are both equal to 1.0, and the county-level GAF trend-adjustment factor can be stated as: C.3.2 Budget-neutrality factor for class of GAF-adjustable claims Because the application of Performance-Year GAFs to base-year claims may cause the GAF-adjusted payment across all adjusted claims to be to be higher or lower than the actual incurred expenditure, a “budget-neutrality” adjustment is applied to the adjusted payment. The budget-neutrality factor is the same for all claims within an adjustment class. A separate budget-neutrality factors is calculated for each class of GAF-adjusted claims (e.g., separate budget-neutrality factors are calculated for acute inpatient claims paid under the IPPS, for SNF claims paid under the SNF PPS, for physician claims paid under the PFS, etc.). For a class of GAF-adjustable claims, the GAF trend-adjusted expenditure before the application of the budget neutrality factor is the sum across all beneficiaries residing in the county of the locality adjusted expenditure for that type of claim during months that accrue to the entitlement category during the base year. The budget-neutrality factor for a class of GAF-adjustable claims is the ratio of: 1. The total GAF trend-adjusted expenditure for that class of claims across all counties (or, equivalently, across all alignment-eligible beneficiaries); to 2. The total incurred (actual) expenditure for that class of claims across all counties. Formally: where = the national Performance-Year t budget-neutrality factor for claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
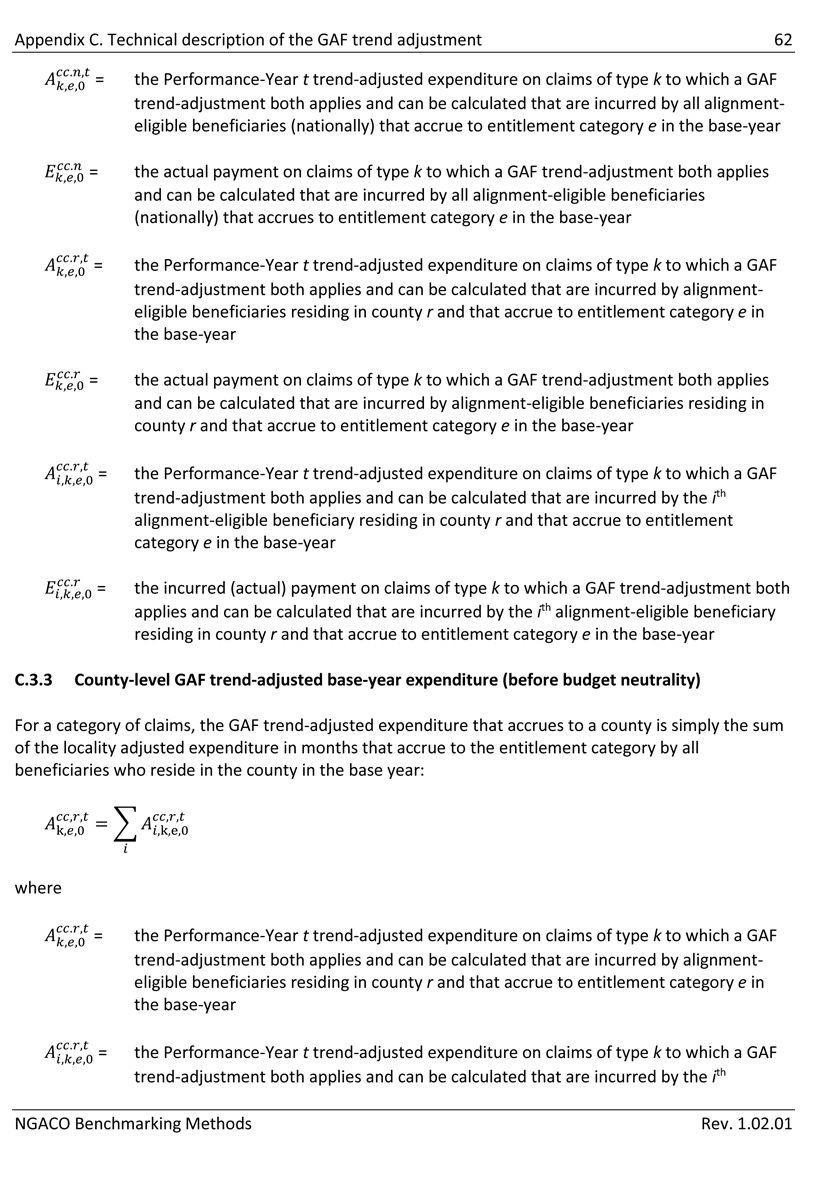
Appendix C. Technical description of the GAF trend adjustment 62 = the Performance-Year t trend-adjusted expenditure on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by all alignment- eligible beneficiaries (nationally) that accrue to entitlement category e in the base-year = the actual payment on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by all alignment-eligible beneficiaries (nationally) that accrues to entitlement category e in the base-year = the Performance-Year t trend-adjusted expenditure on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by alignment- eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the actual payment on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the Performance-Year t trend-adjusted expenditure on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by the ith alignment-eligible beneficiary residing in county r and that accrue to entitlement category e in the base-year = the incurred (actual) payment on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by the ith alignment-eligible beneficiary residing in county r and that accrue to entitlement category e in the base-year C.3.3 County-level GAF trend-adjusted base-year expenditure (before budget neutrality) For a category of claims, the GAF trend-adjusted expenditure that accrues to a county is simply the sum of the locality adjusted expenditure in months that accrue to the entitlement category by all beneficiaries who reside in the county in the base year: ,k,e,0 where = the Performance-Year t trend-adjusted expenditure on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by alignment- eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the Performance-Year t trend-adjusted expenditure on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by the ith NGACO Benchmarking Methods Rev. 1.02.01
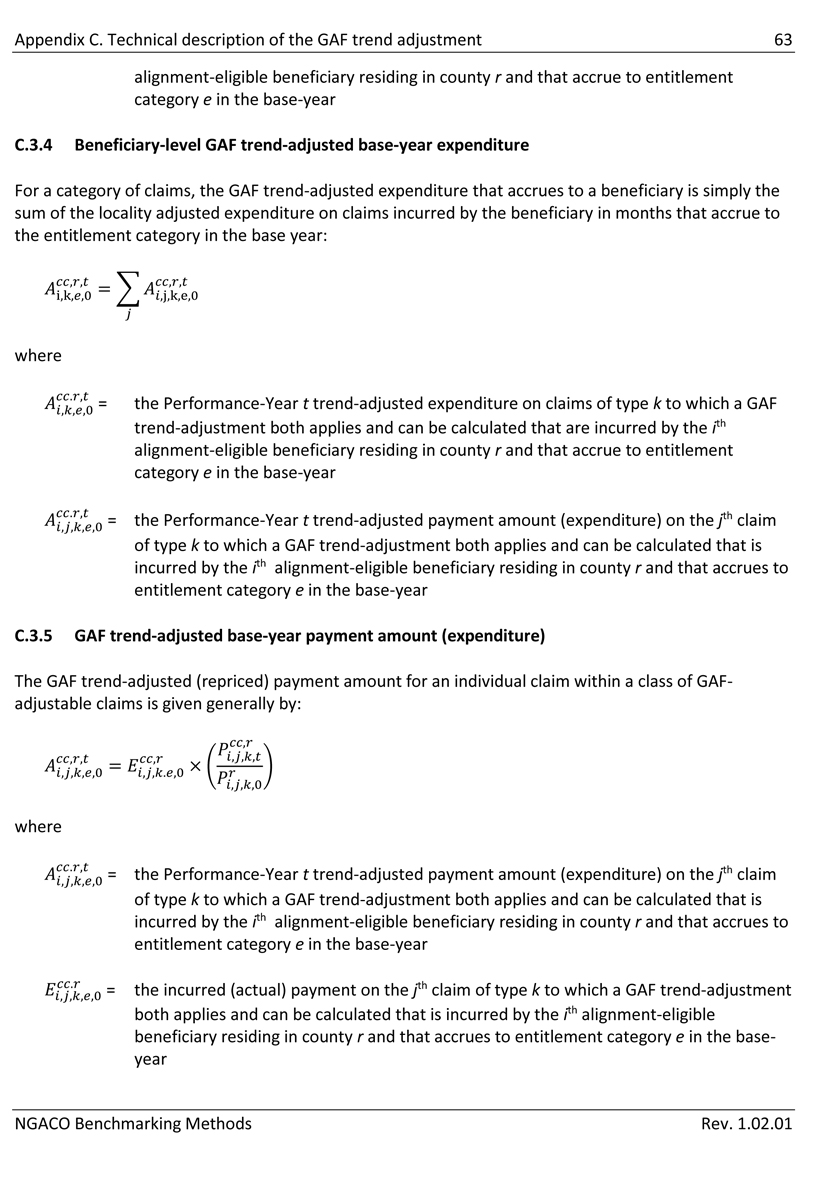
Appendix C. Technical description of the GAF trend adjustment 63 alignment-eligible beneficiary residing in county r and that accrue to entitlement category e in the base-year C.3.4 Beneficiary-level GAF trend-adjusted base-year expenditure For a category of claims, the GAF trend-adjusted expenditure that accrues to a beneficiary is simply the sum of the locality adjusted expenditure on claims incurred by the beneficiary in months that accrue to the entitlement category in the base year: i,k, ,j,k,e,0 where = the Performance-Year t trend-adjusted expenditure on claims of type k to which a GAF trend-adjustment both applies and can be calculated that are incurred by the ith alignment-eligible beneficiary residing in county r and that accrue to entitlement category e in the base-year = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year C.3.5 GAF trend-adjusted base-year payment amount (expenditure) The GAF trend-adjusted (repriced) payment amount for an individual claim within a class of GAF- adjustable claims is given generally by: where = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base- year NGACO Benchmarking Methods Rev. 1.02.01
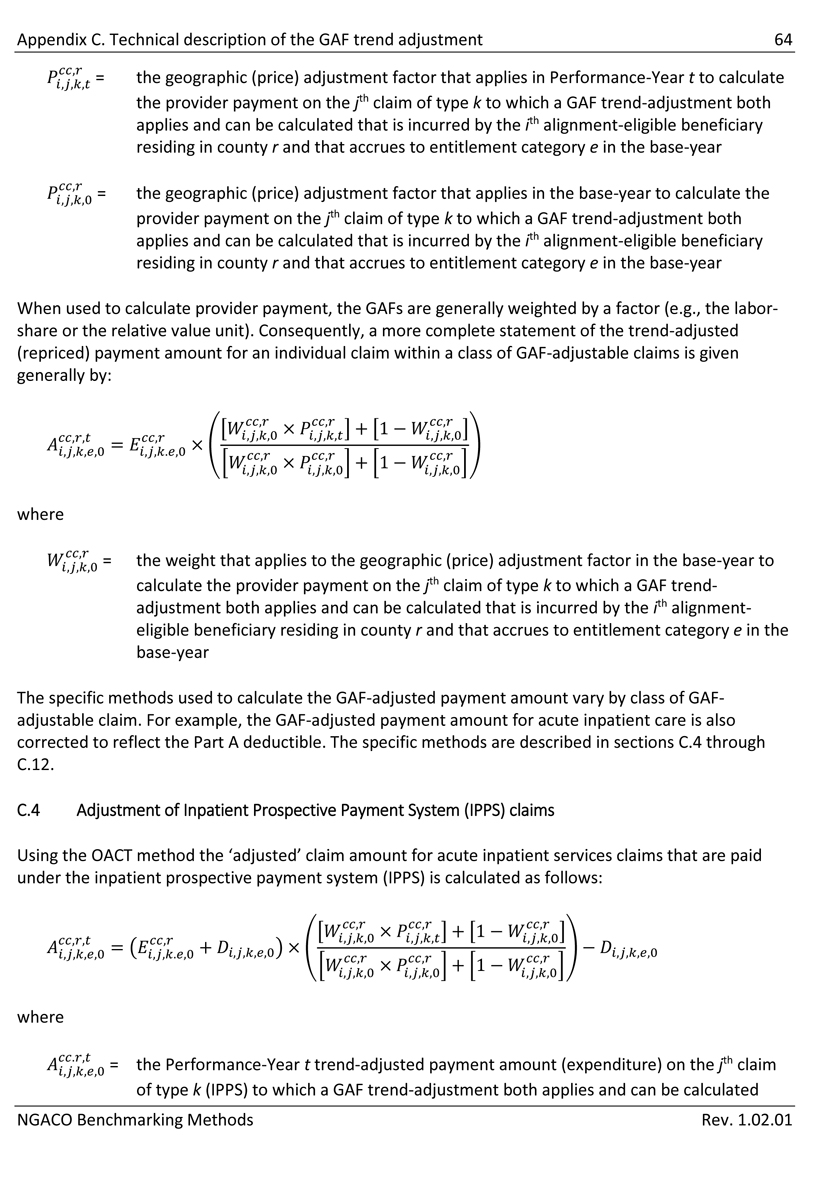
Appendix C. Technical description of the GAF trend adjustment 64 = the geographic (price) adjustment factor that applies in Performance-Year t to calculate the provider payment on the jth claim of type k to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the geographic (price) adjustment factor that applies in the base-year to calculate the provider payment on the jth claim of type k to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year When used to calculate provider payment, the GAFs are generally weighted by a factor (e.g., the labor- share or the relative value unit). Consequently, a more complete statement of the trend-adjusted (repriced) payment amount for an individual claim within a class of GAF-adjustable claims is given generally by: where = the weight that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The specific methods used to calculate the GAF-adjusted payment amount vary by class of GAF- adjustable claim. For example, the GAF-adjusted payment amount for acute inpatient care is also corrected to reflect the Part A deductible. The specific methods are described in sections C.4 through C.12. C.4 Adjustment of Inpatient Prospective Payment System (IPPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (IPPS) is calculated as follows: where = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k (IPPS) to which a GAF trend-adjustment both applies and can be calculated NGACO Benchmarking Methods Rev. 1.02.01
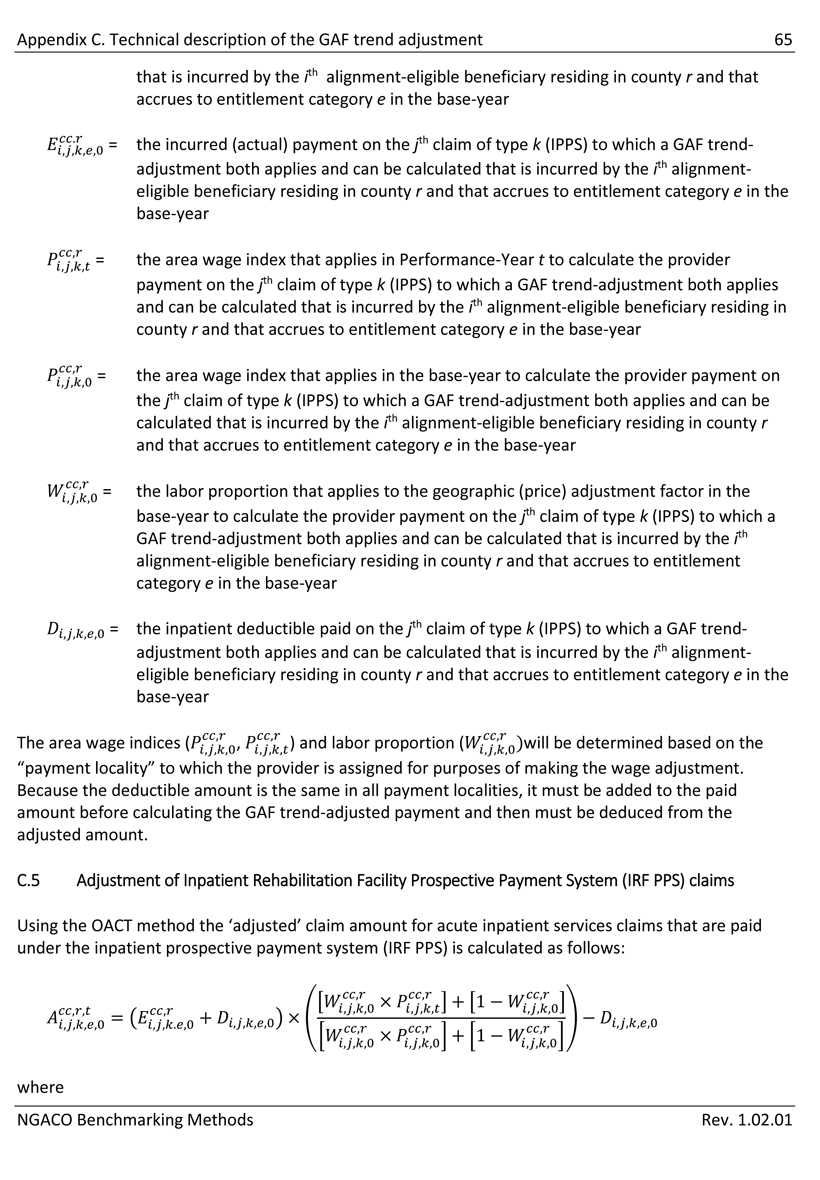
Appendix C. Technical description of the GAF trend adjustment 65 that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (IPPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (IPPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (IPPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (IPPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the inpatient deductible paid on the jth claim of type k (IPPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Because the deductible amount is the same in all payment localities, it must be added to the paid amount before calculating the GAF trend-adjusted payment and then must be deduced from the adjusted amount. C.5 Adjustment of Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (IRF PPS) is calculated as follows: where NGACO Benchmarking Methods Rev. 1.02.01
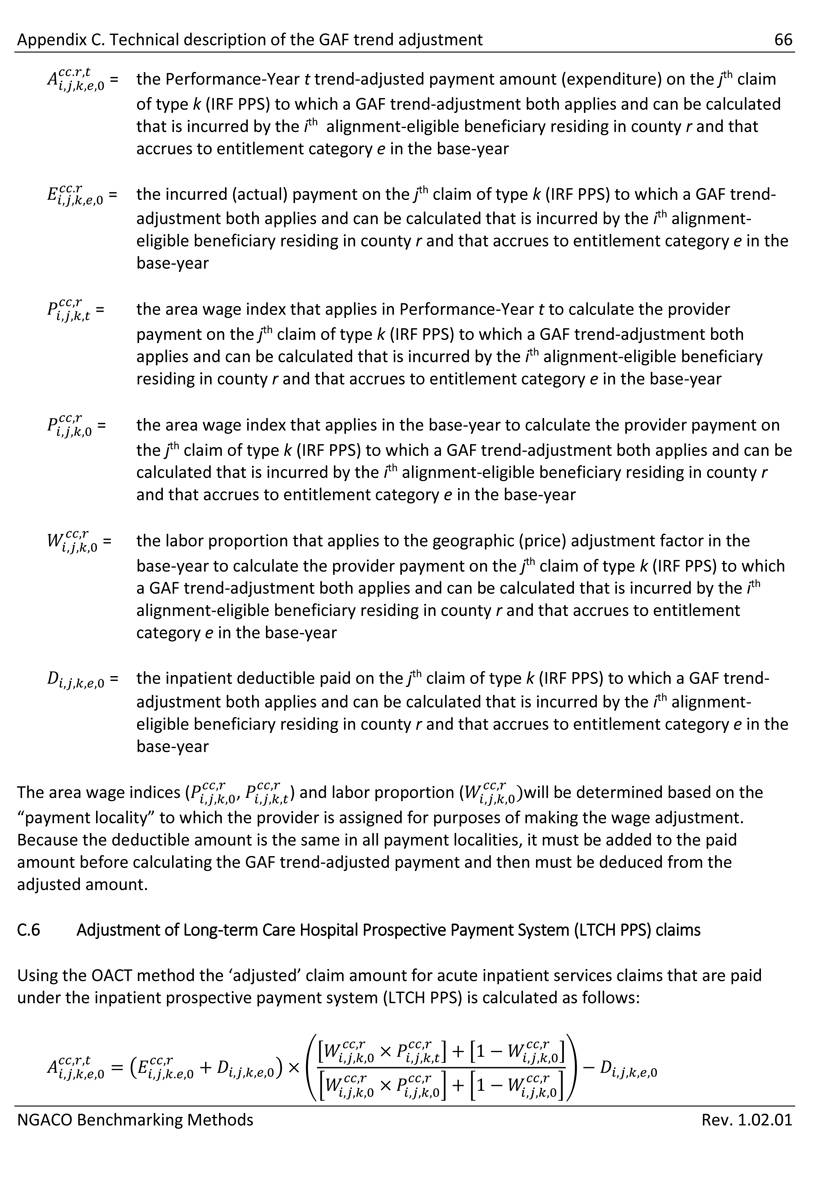
Appendix C. Technical description of the GAF trend adjustment 66 = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k (IRF PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (IRF PPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (IRF PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (IRF PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (IRF PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the inpatient deductible paid on the jth claim of type k (IRF PPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Because the deductible amount is the same in all payment localities, it must be added to the paid amount before calculating the GAF trend-adjusted payment and then must be deduced from the adjusted amount. C.6 Adjustment of Long-term Care Hospital Prospective Payment System (LTCH PPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (LTCH PPS) is calculated as follows: where NGACO Benchmarking Methods Rev. 1.02.01
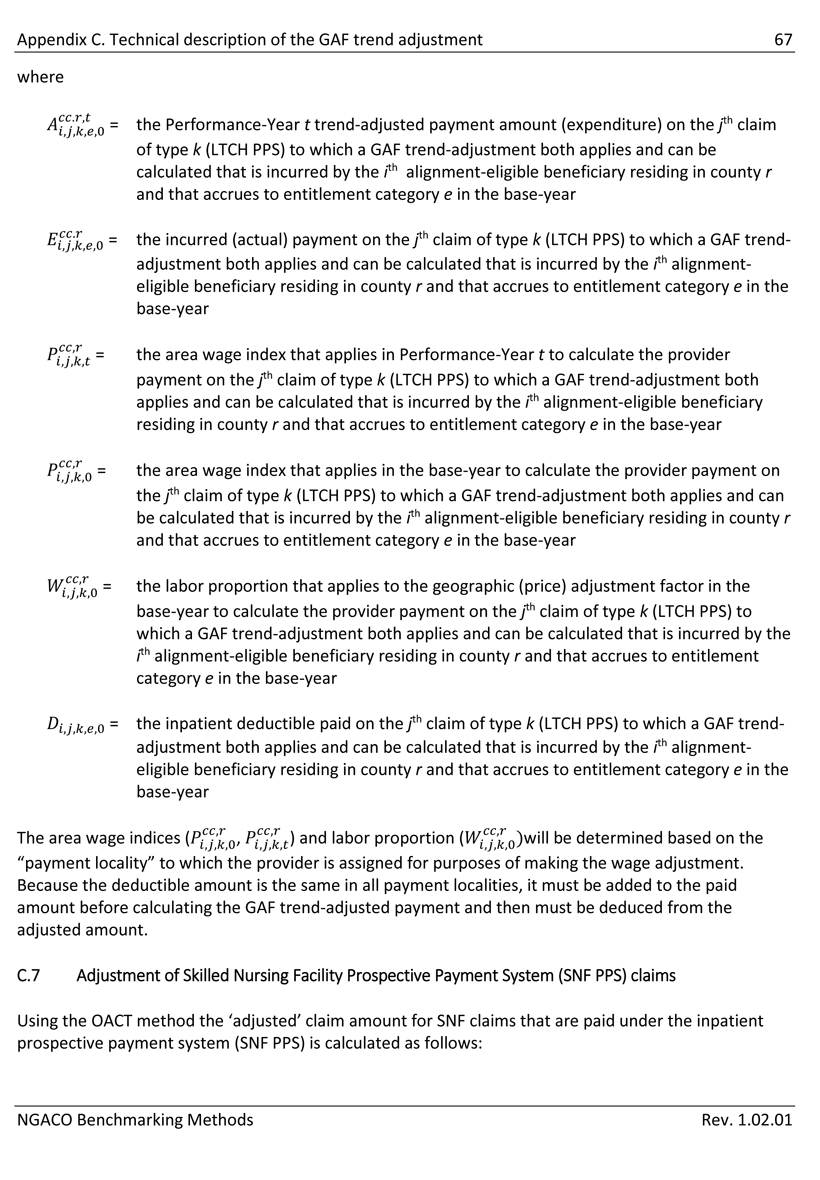
Appendix C. Technical description of the GAF trend adjustment 67 where = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k (LTCH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (LTCH PPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (LTCH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (LTCH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (LTCH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the inpatient deductible paid on the jth claim of type k (LTCH PPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Because the deductible amount is the same in all payment localities, it must be added to the paid amount before calculating the GAF trend-adjusted payment and then must be deduced from the adjusted amount. C.7 Adjustment of Skilled Nursing Facility Prospective Payment System (SNF PPS) claims Using the OACT method the ‘adjusted’ claim amount for SNF claims that are paid under the inpatient prospective payment system (SNF PPS) is calculated as follows: NGACO Benchmarking Methods Rev. 1.02.01
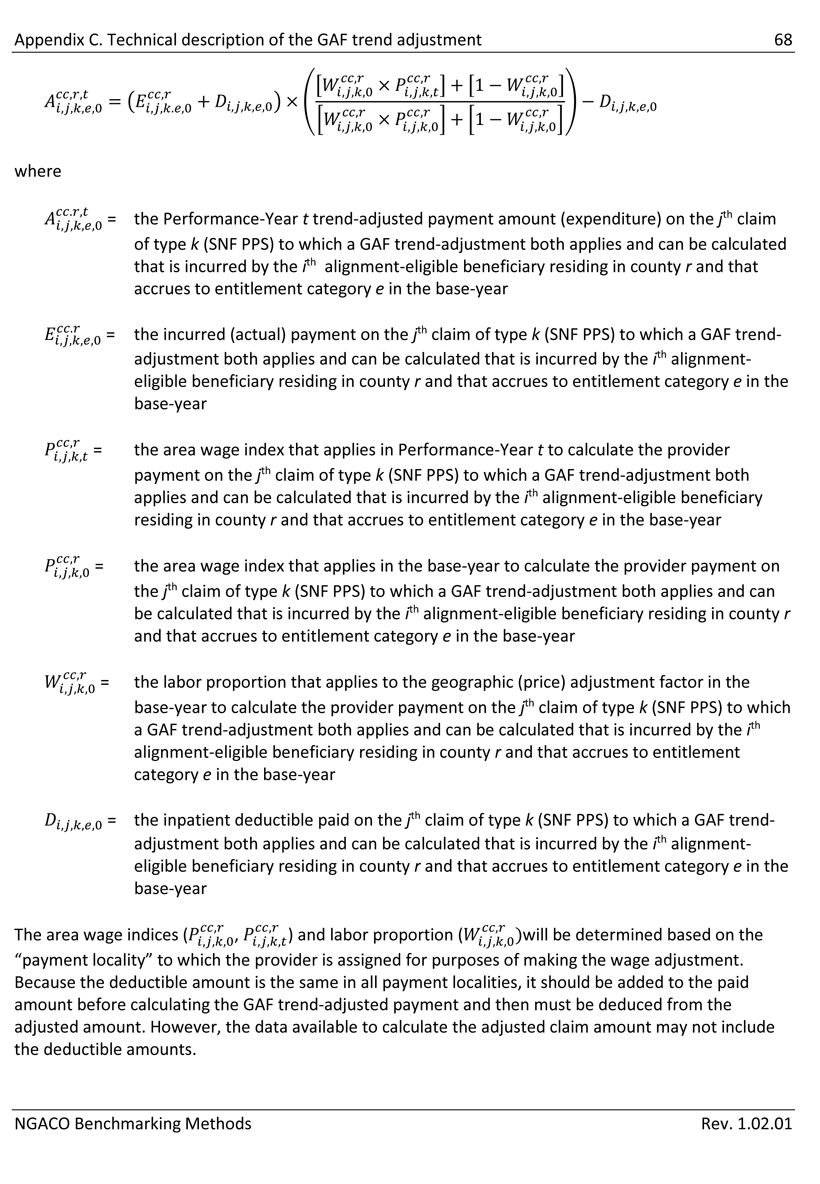
Appendix C. Technical description of the GAF trend adjustment 68 where = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k (SNF PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (SNF PPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (SNF PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (SNF PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (SNF PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the inpatient deductible paid on the jth claim of type k (SNF PPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Because the deductible amount is the same in all payment localities, it should be added to the paid amount before calculating the GAF trend-adjusted payment and then must be deduced from the adjusted amount. However, the data available to calculate the adjusted claim amount may not include the deductible amounts. NGACO Benchmarking Methods Rev. 1.02.01
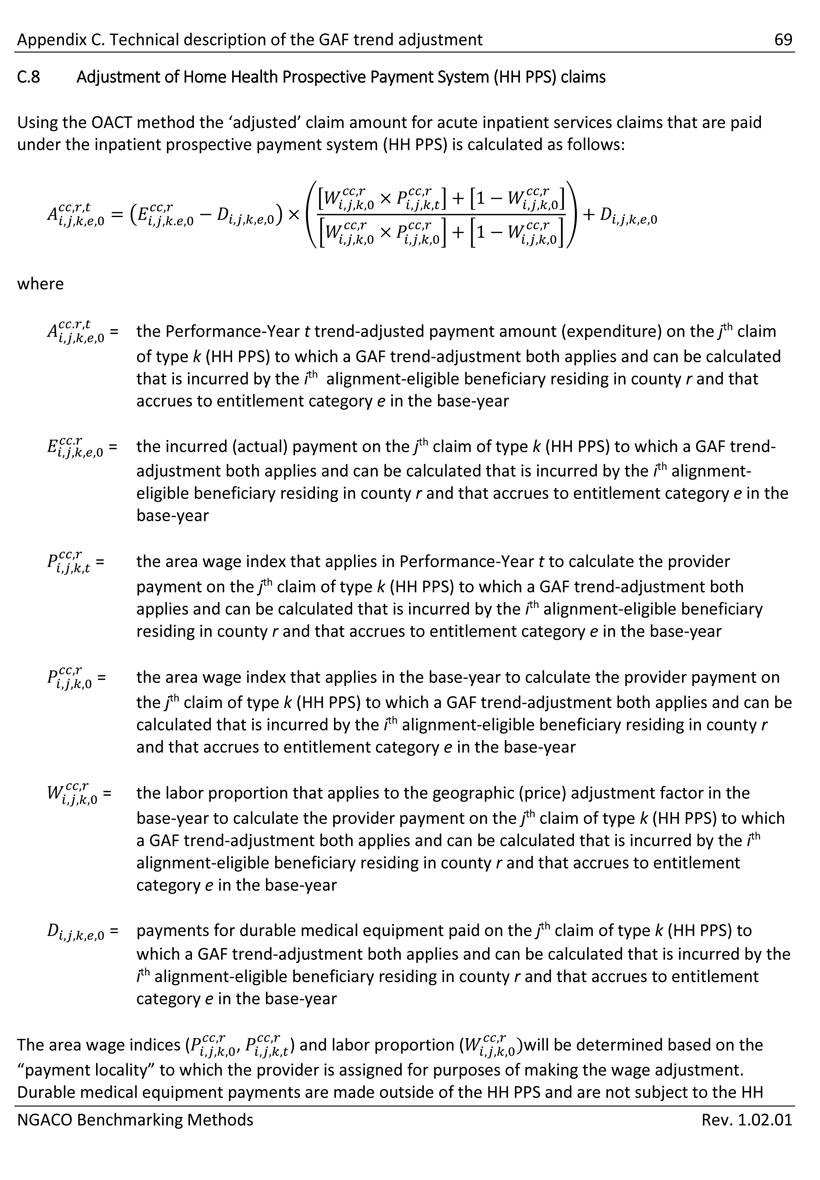
Appendix C. Technical description of the GAF trend adjustment 69 C.8 Adjustment of Home Health Prospective Payment System (HH PPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (HH PPS) is calculated as follows: where = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k (HH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (HH PPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (HH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (HH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (HH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = payments for durable medical equipment paid on the jth claim of type k (HH PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Durable medical equipment payments are made outside of the HH PPS and are not subject to the HH NGACO Benchmarking Methods Rev. 1.02.01
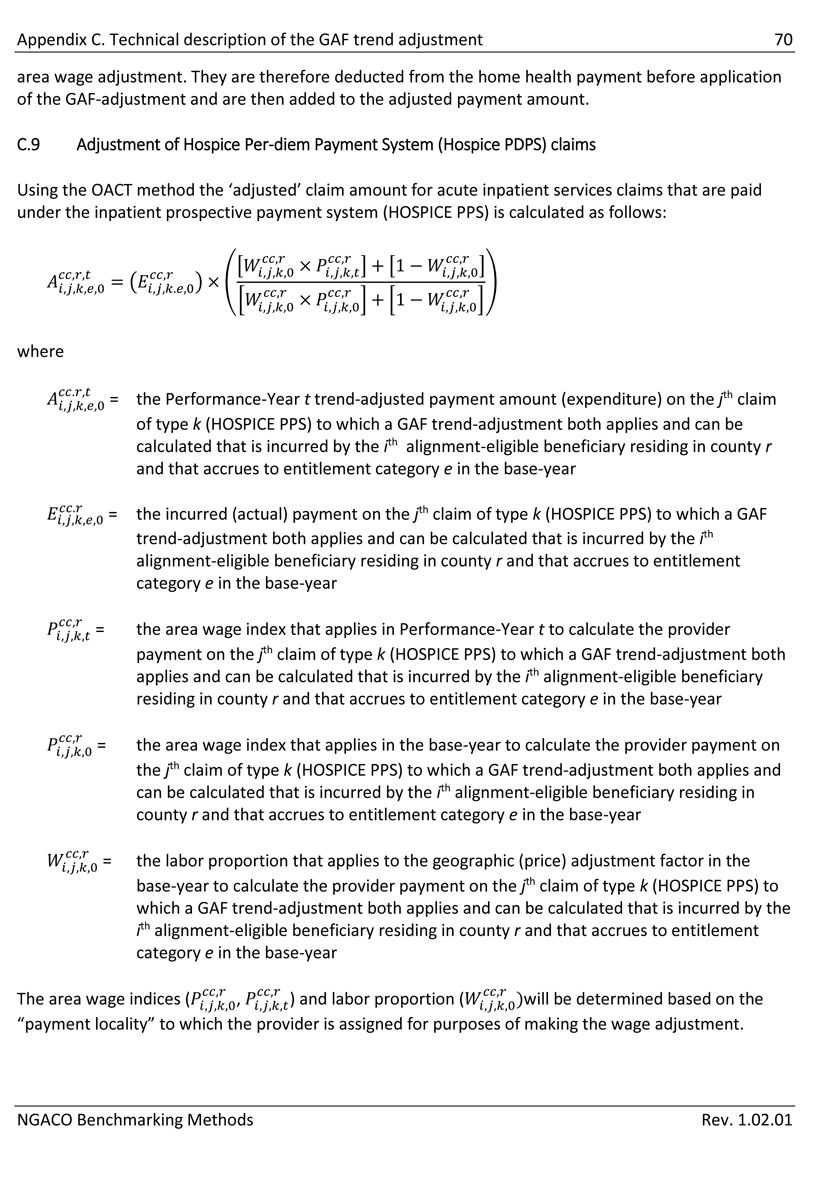
Appendix C. Technical description of the GAF trend adjustment 70 area wage adjustment. They are therefore deducted from the home health payment before application of the GAF-adjustment and are then added to the adjusted payment amount. C.9 Adjustment of Hospice Per-diem Payment System (Hospice PDPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (HOSPICE PPS) is calculated as follows: where = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k (HOSPICE PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (HOSPICE PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (HOSPICE PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (HOSPICE PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (HOSPICE PPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. NGACO Benchmarking Methods Rev. 1.02.01
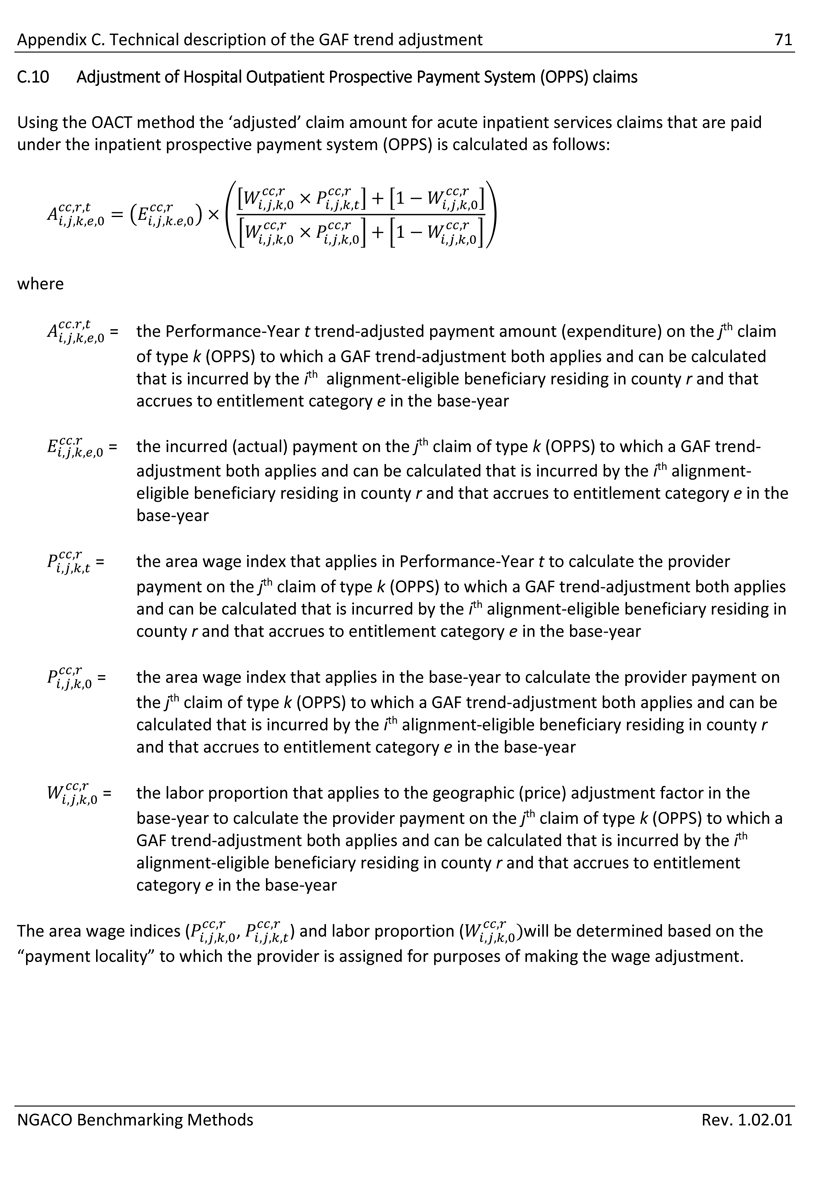
Appendix C. Technical description of the GAF trend adjustment 71 C.10 Adjustment of Hospital Outpatient Prospective Payment System (OPPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (OPPS) is calculated as follows: where = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k (OPPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (OPPS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (OPPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (OPPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (OPPS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. NGACO Benchmarking Methods Rev. 1.02.01
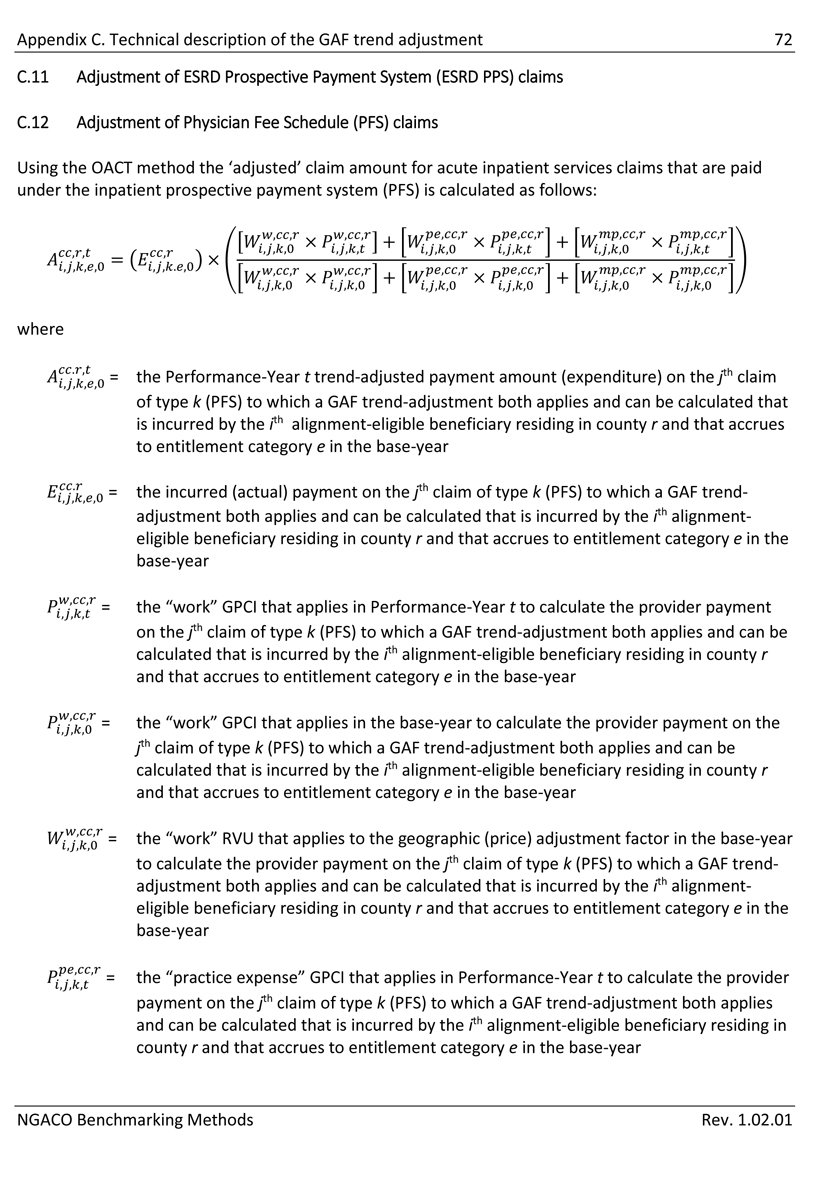
Appendix C. Technical description of the GAF trend adjustment 72 C.11 Adjustment of ESRD Prospective Payment System (ESRD PPS) claims C.12 Adjustment of Physician Fee Schedule (PFS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (PFS) is calculated as follows: where = the Performance-Year t trend-adjusted payment amount (expenditure) on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (PFS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “work” GPCI that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “work” GPCI that applies in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “work” RVU that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “practice expense” GPCI that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
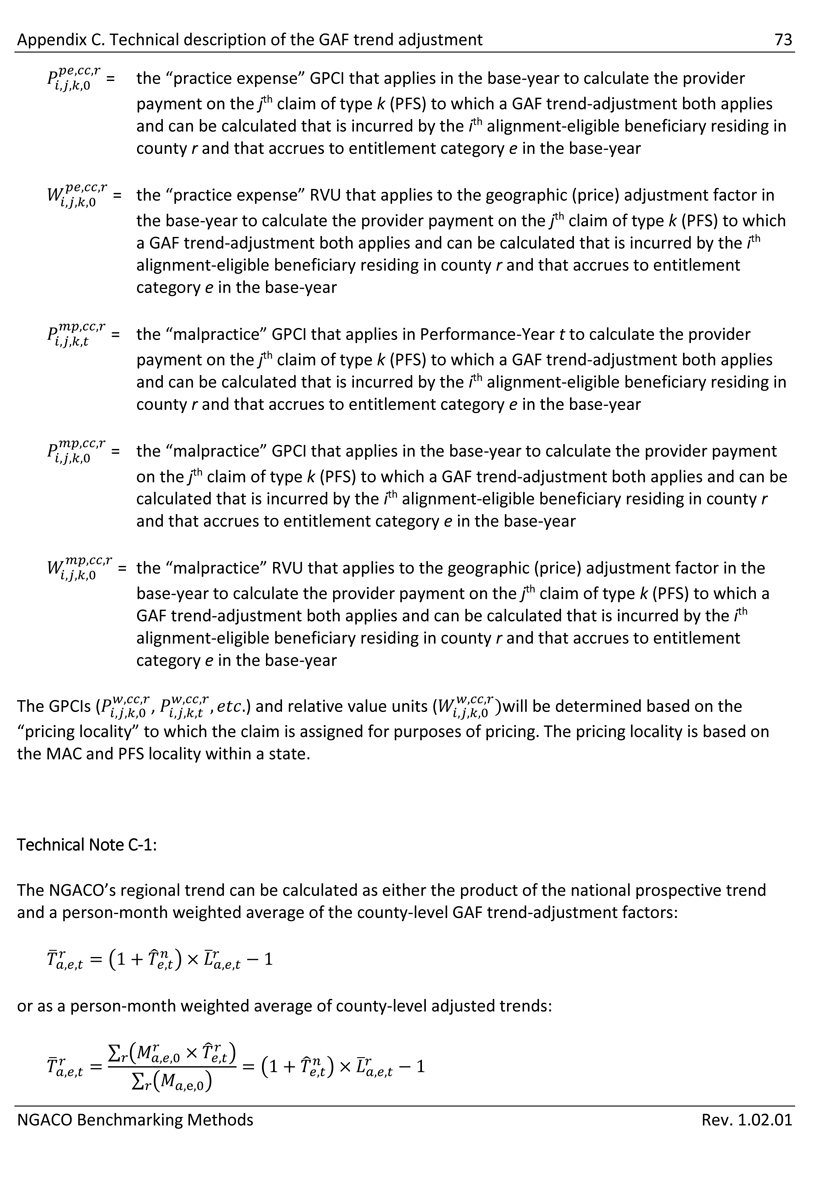
Appendix C. Technical description of the GAF trend adjustment 73 = the “practice expense” GPCI that applies in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “practice expense” RVU that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “malpractice” GPCI that applies in Performance-Year t to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “malpractice” GPCI that applies in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “malpractice” RVU that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF trend-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year) and relative value units ()will be determined based on the The GPCIs ( “pricing locality” to which the claim is assigned for purposes of pricing. The pricing locality is based on the MAC and PFS locality within a state. Technical Note C-1: The NGACO’s regional trend can be calculated as either the product of the national prospective trend and a person-month weighted average of the county-level GAF trend-adjustment factors: or as a person-month weighted average of county-level adjusted trends: NGACO Benchmarking Methods Rev. 1.02.01
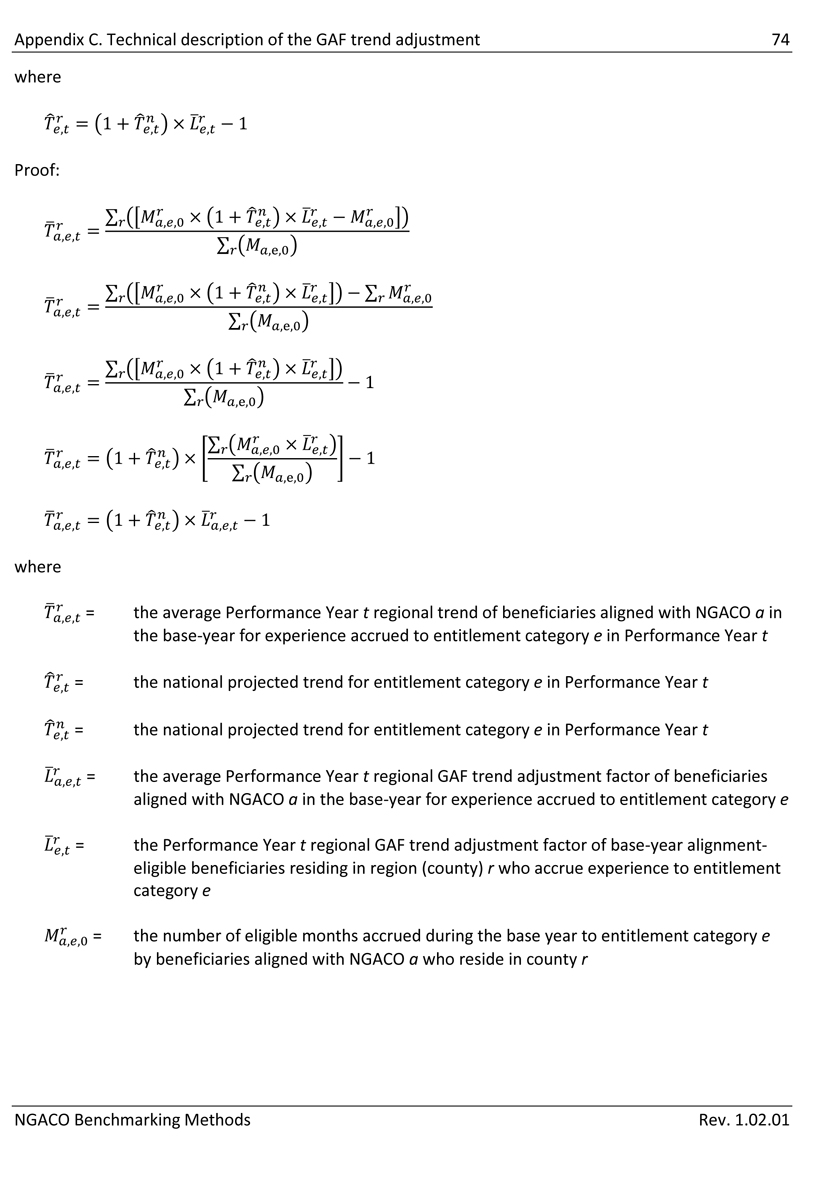
Appendix C. Technical description of the GAF trend adjustment 74 where Proof: where = the average Performance Year t regional trend of beneficiaries aligned with NGACO a in the base-year for experience accrued to entitlement category e in Performance Year t = the national projected trend for entitlement category e in Performance Year t = the national projected trend for entitlement category e in Performance Year t = the average Performance Year t regional GAF trend adjustment factor of beneficiaries aligned with NGACO a in the base-year for experience accrued to entitlement category e = the Performance Year t regional GAF trend adjustment factor of base-year alignment- eligible beneficiaries residing in region (county) r who accrue experience to entitlement category e = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a who reside in county r NGACO Benchmarking Methods Rev. 1.02.01
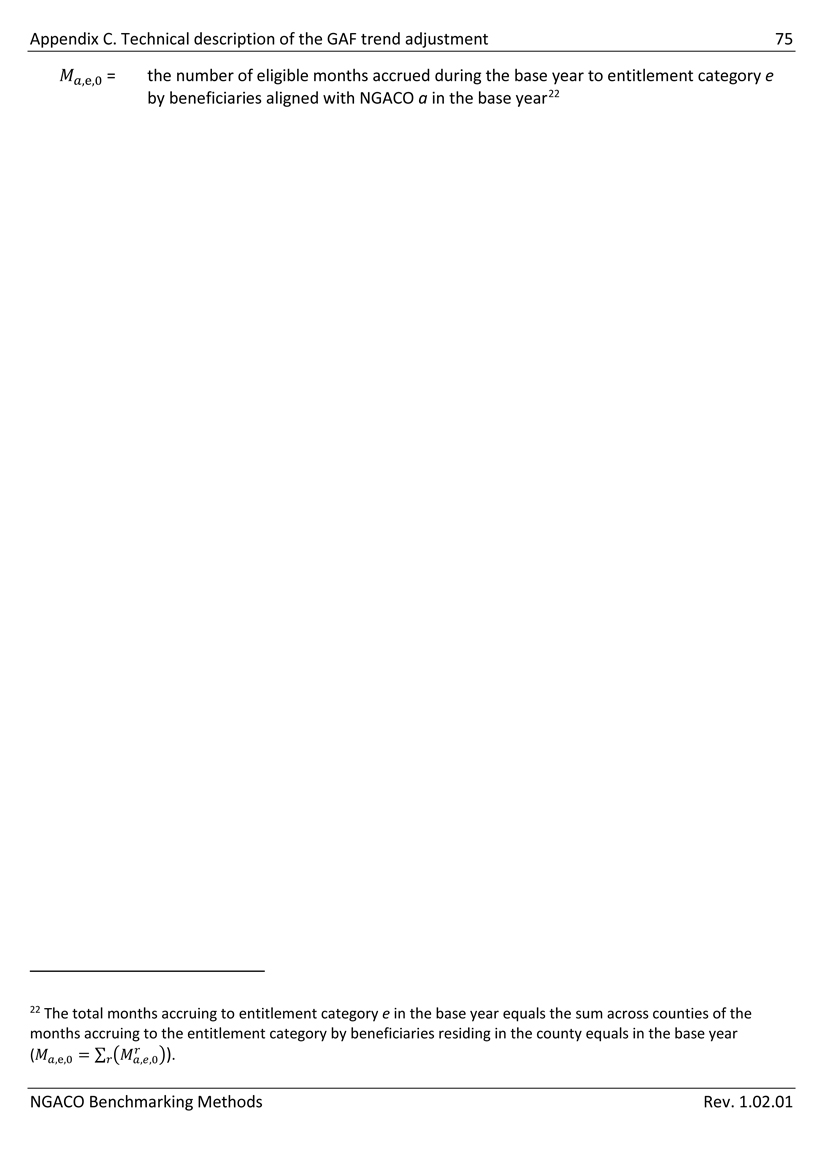
Appendix C. Technical description of the GAF trend adjustment 75 = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a in the base year22 22 The total months accruing to entitlement category e in the base year equals the sum across counties of the months accruing to the entitlement category by beneficiaries residing in the county equals in the base year (NGACO Benchmarking Methods Rev. 1.02.01
| Appendix D. Technical description of the GAF baseline-adjustment | 76 |
Appendix D. Technical description of the GAF baseline-adjustment
Provider payments under most Medicare fee-for-service (FFS) payment systems reflect an adjustment for the cost-of-doing business in the local geographic area in which the provider is located.23 These geographic adjustment factors can cause differences of up to ±10% or more in the payments that are made for the same services in different regions. The purpose of the GAF baseline adjustment in the NGACO Model is to prevent the efficiency adjustment (particularly the national efficiency adjustment) to the standard discount, and therefore the benchmark, from being unfairly understated (or overstated) because of differences between the GAFs that Medicare used to calculate provider payments in the base-year (CY2014).
| D.1 | Overview of the GAF baseline-adjustment |
The GAF baseline-adjustment factor is a county-level adjustment. The GAF baseline-adjustment factor for a county is an estimate of the impact of the base-year Medicare GAFs on the base-year provider payments for services provided to reference beneficiaries residing in the county. That is, the GAF baseline-adjustment is an estimate of the amount by which the base-year expenditure of residents of a county was increased or decreased relative to the national average based solely on the base-year GAFs that were used to calculate provider payments.
The GAF baseline-adjustment factor for a county will be the ratio of:
| 1. | The base-year expenditure24 incurred by residents of a county adjusted to remove the impact on provider payments of the geographic pricing factors that Medicare used in the base-year; to, |
| 2. | The actual expenditure incurred by residents of a county, which reflects the geographic pricing factors that Medicare used to calculate provider payments in the base year. |
The GAF baseline-adjustment factor will be calculated prospectively for alignment-eligible beneficiaries in each county in the base year and will have no impact on the national baseline reference-population expenditure.25
23 Examples of these Geographic Adjustment Factors (GAFs) are the Medicare area wage index (AWI) and the geographic practice cost index (GPCI).
24 The GAF adjustment is the ratio of: (1) the aggregate normalized or budget-neutral GAF-adjusted provider payment; to (2) the aggregate unadjusted provider payment. It is not necessary to convert the aggregate provider payment to a PBPM amount.
25 The GAF-trend adjustment will be calculated on a budget-neutral basis so that the regional GAF baseline- adjustments neither increase nor decrease the total expenditure of the reference population nationally. That is the baseline GAF-adjusted claim amount for the reference population will equal the incurred claim amount.
| NGACO Benchmarking Methods | Rev. 1.02.01 |
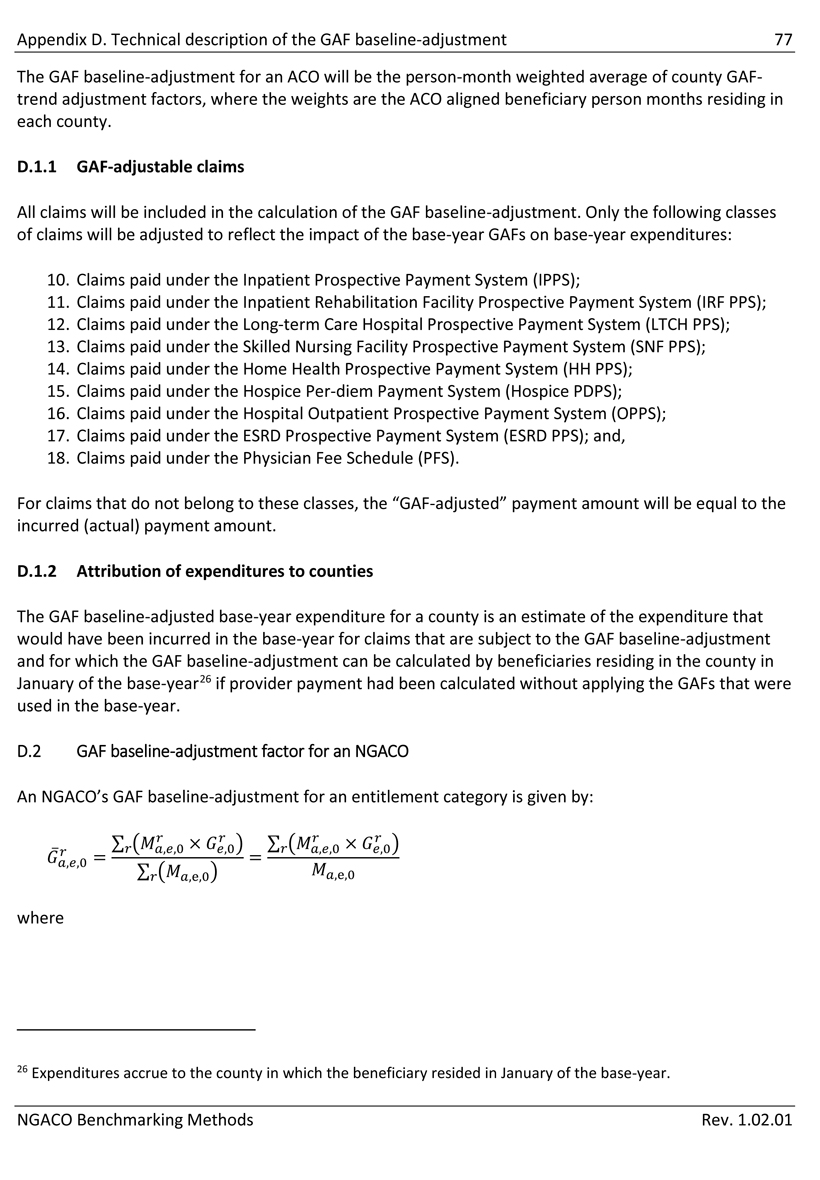
Appendix D. Technical description of the GAF baseline-adjustment 77 The GAF baseline-adjustment for an ACO will be the person-month weighted average of county GAF- trend adjustment factors, where the weights are the ACO aligned beneficiary person months residing in each county. D.1.1 GAF-adjustable claims All claims will be included in the calculation of the GAF baseline-adjustment. Only the following classes of claims will be adjusted to reflect the impact of the base-year GAFs on base-year expenditures: 10. Claims paid under the Inpatient Prospective Payment System (IPPS); 11. Claims paid under the Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS); 12. Claims paid under the Long-term Care Hospital Prospective Payment System (LTCH PPS); 13. Claims paid under the Skilled Nursing Facility Prospective Payment System (SNF PPS); 14. Claims paid under the Home Health Prospective Payment System (HH PPS); 15. Claims paid under the Hospice Per-diem Payment System (Hospice PDPS); 16. Claims paid under the Hospital Outpatient Prospective Payment System (OPPS); 17. Claims paid under the ESRD Prospective Payment System (ESRD PPS); and, 18. Claims paid under the Physician Fee Schedule (PFS). For claims that do not belong to these classes, the “GAF-adjusted” payment amount will be equal to the incurred (actual) payment amount. D.1.2 Attribution of expenditures to counties The GAF baseline-adjusted base-year expenditure for a county is an estimate of the expenditure that would have been incurred in the base-year for claims that are subject to the GAF baseline-adjustment and for which the GAF baseline-adjustment can be calculated by beneficiaries residing in the county in January of the base-year26 if provider payment had been calculated without applying the GAFs that were used in the base-year. D.2 GAF baseline-adjustment factor for an NGACO An NGACO’s GAF baseline-adjustment for an entitlement category is given by: where 26 Expenditures accrue to the county in which the beneficiary resided in January of the base-year. NGACO Benchmarking Methods Rev. 1.02.01
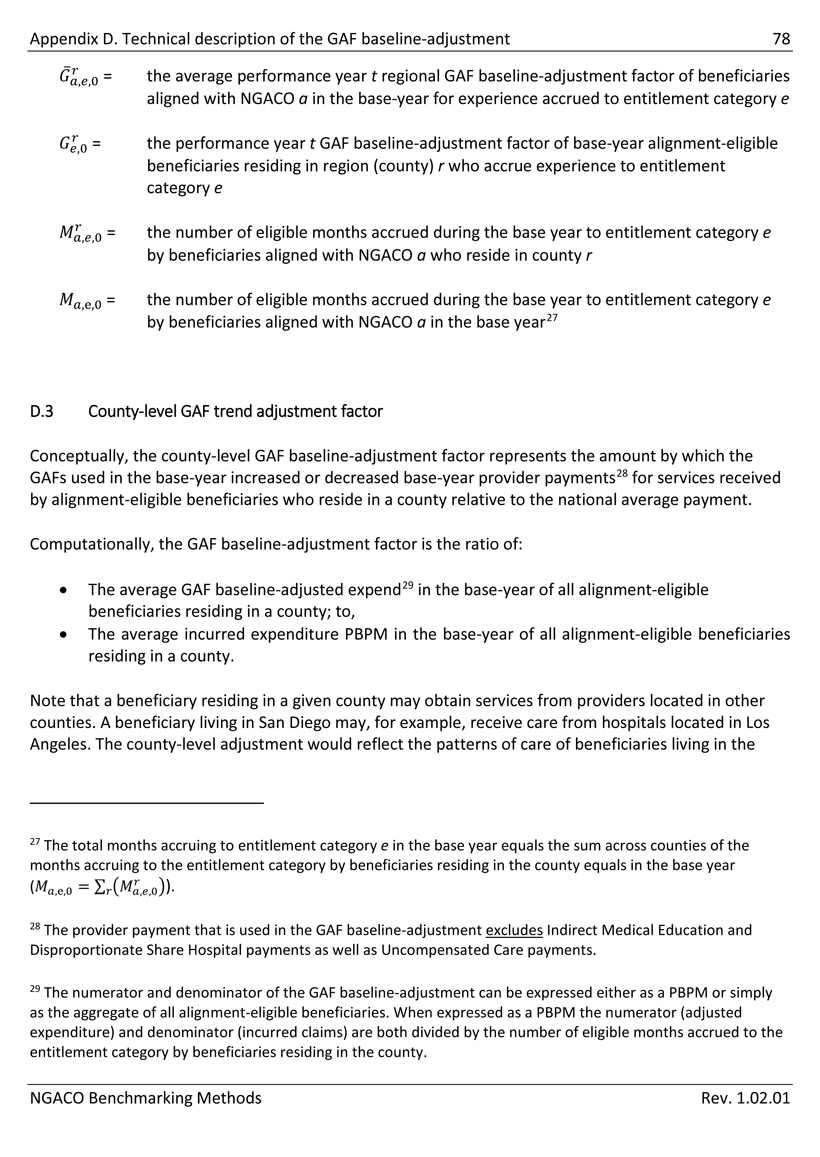
Appendix D. Technical description of the GAF baseline-adjustment 78 = the average performance year t regional GAF baseline-adjustment factor of beneficiaries aligned with NGACO a in the base-year for experience accrued to entitlement category e = the performance year t GAF baseline-adjustment factor of base-year alignment-eligible beneficiaries residing in region (county) r who accrue experience to entitlement category e = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a who reside in county r = the number of eligible months accrued during the base year to entitlement category e by beneficiaries aligned with NGACO a in the base year27 D.3 County-level GAF trend adjustment factor Conceptually, the county-level GAF baseline-adjustment factor represents the amount by which the GAFs used in the base-year increased or decreased base-year provider payments28 for services received by alignment-eligible beneficiaries who reside in a county relative to the national average payment. Computationally, the GAF baseline-adjustment factor is the ratio of: • The average GAF baseline-adjusted expend29 in the base-year of all alignment-eligible beneficiaries residing in a county; to, • The average incurred expenditure PBPM in the base-year of all alignment-eligible beneficiaries residing in a county. Note that a beneficiary residing in a given county may obtain services from providers located in other counties. A beneficiary living in San Diego may, for example, receive care from hospitals located in Los Angeles. The county-level adjustment would reflect the patterns of care of beneficiaries living in the 27 The total months accruing to entitlement category e in the base year equals the sum across counties of the months accruing to the entitlement category by beneficiaries residing in the county equals in the base year (). 28 The provider payment that is used in the GAF baseline-adjustment excludes Indirect Medical Education and Disproportionate Share Hospital payments as well as Uncompensated Care payments. 29 The numerator and denominator of the GAF baseline-adjustment can be expressed either as a PBPM or simply as the aggregate of all alignment-eligible beneficiaries. When expressed as a PBPM the numerator (adjusted expenditure) and denominator (incurred claims) are both divided by the number of eligible months accrued to the entitlement category by beneficiaries residing in the county. NGACO Benchmarking Methods Rev. 1.02.01
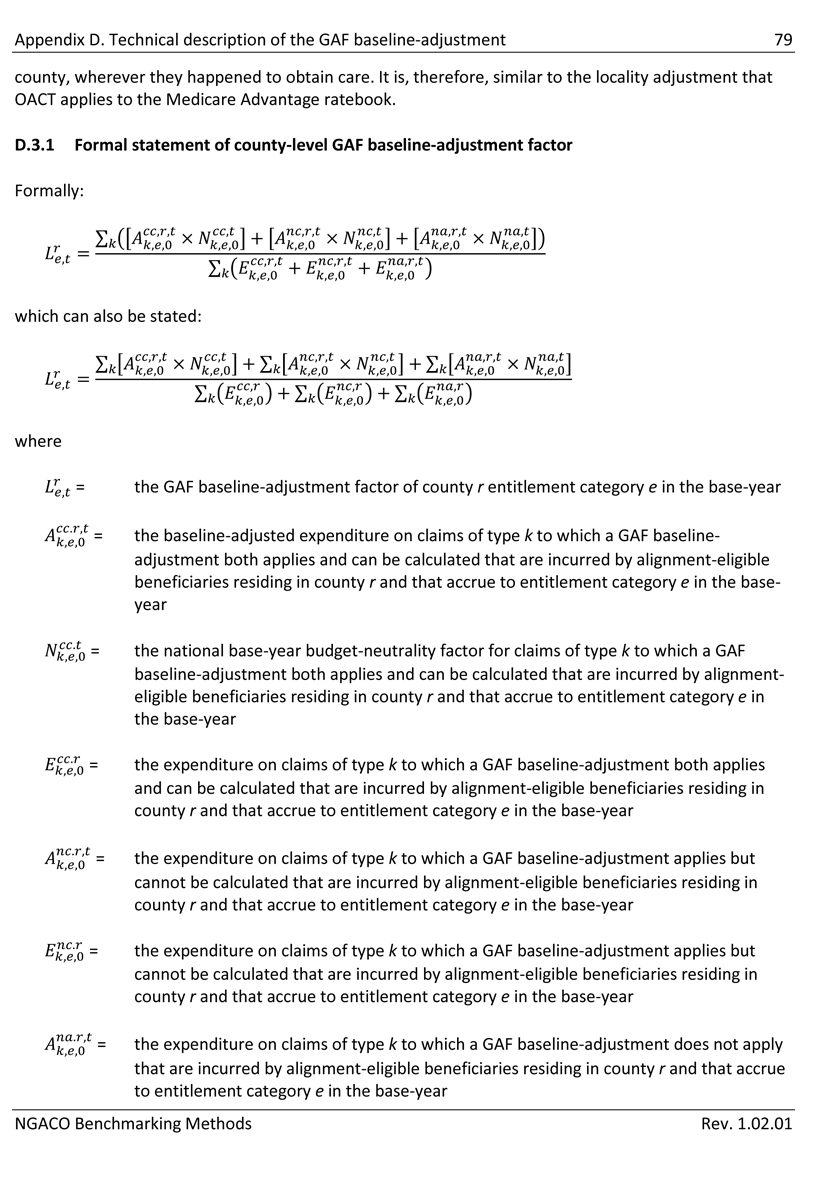
Appendix D. Technical description of the GAF baseline-adjustment 79 county, wherever they happened to obtain care. It is, therefore, similar to the locality adjustment that OACT applies to the Medicare Advantage ratebook. D.3.1 Formal statement of county-level GAF baseline-adjustment factor Formally: which can also be stated: where = the GAF baseline-adjustment factor of county r entitlement category e in the base-year = the baseline-adjusted expenditure on claims of type k to which a GAF baseline- adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base- year = the national base-year budget-neutrality factor for claims of type k to which a GAF baseline-adjustment both applies and can be calculated that are incurred by alignment- eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the expenditure on claims of type k to which a GAF baseline-adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the expenditure on claims of type k to which a GAF baseline-adjustment applies but cannot be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the expenditure on claims of type k to which a GAF baseline-adjustment applies but cannot be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the expenditure on claims of type k to which a GAF baseline-adjustment does not apply that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
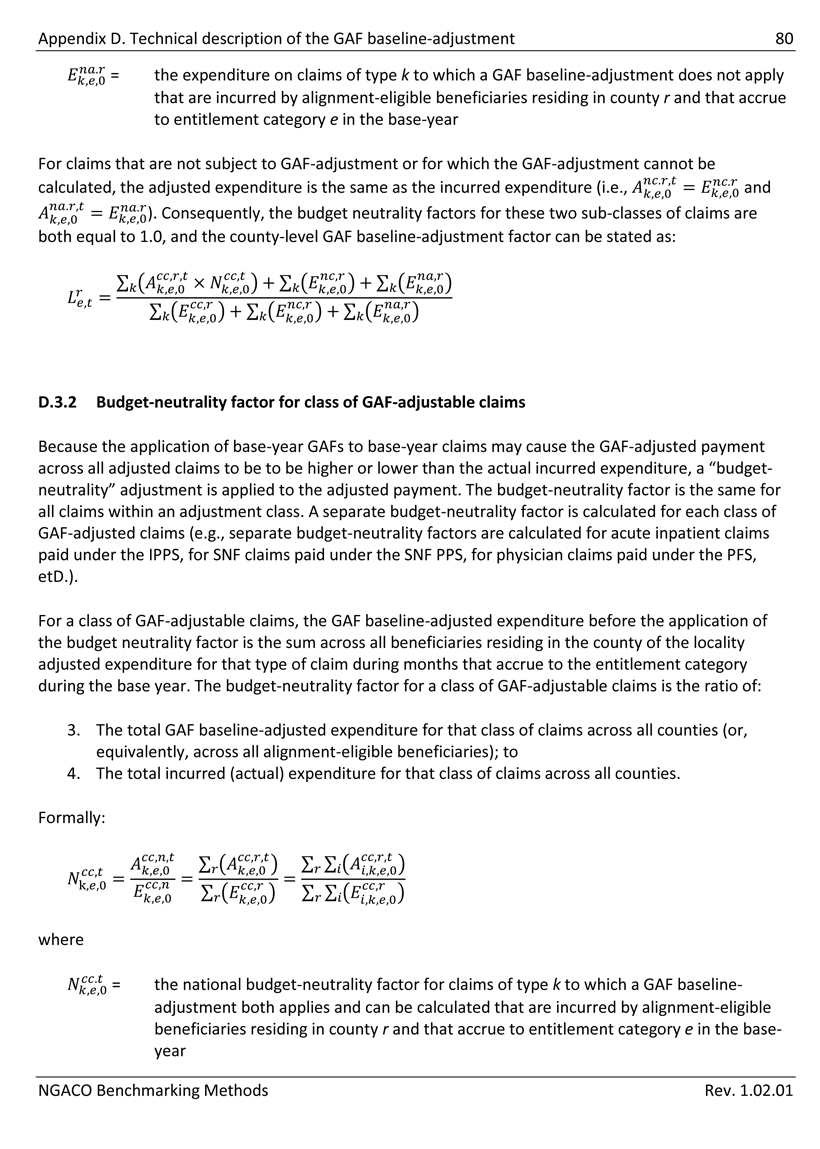
Appendix D. Technical description of the GAF baseline-adjustment 80 = the expenditure on claims of type k to which a GAF baseline-adjustment does not apply that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year For claims that are not subject to GAF-adjustment or for which the GAF-adjustment cannot be calculated, the adjusted expenditure is the same as the incurred expenditure (i.e.,). Consequently, the budget neutrality factors for these two sub-classes of claims are both equal to 1.0, and the county-level GAF baseline-adjustment factor can be stated as: D.3.2 Budget-neutrality factor for class of GAF-adjustable claims Because the application of base-year GAFs to base-year claims may cause the GAF-adjusted payment across all adjusted claims to be to be higher or lower than the actual incurred expenditure, a “budget- neutrality” adjustment is applied to the adjusted payment. The budget-neutrality factor is the same for all claims within an adjustment class. A separate budget-neutrality factor is calculated for each class of GAF-adjusted claims (e.g., separate budget-neutrality factors are calculated for acute inpatient claims paid under the IPPS, for SNF claims paid under the SNF PPS, for physician claims paid under the PFS, etD.). For a class of GAF-adjustable claims, the GAF baseline-adjusted expenditure before the application of the budget neutrality factor is the sum across all beneficiaries residing in the county of the locality adjusted expenditure for that type of claim during months that accrue to the entitlement category during the base year. The budget-neutrality factor for a class of GAF-adjustable claims is the ratio of: 3. The total GAF baseline-adjusted expenditure for that class of claims across all counties (or, equivalently, across all alignment-eligible beneficiaries); to 4. The total incurred (actual) expenditure for that class of claims across all counties. Formally: where = the national budget-neutrality factor for claims of type k to which a GAF baseline- adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base- year NGACO Benchmarking Methods Rev. 1.02.01
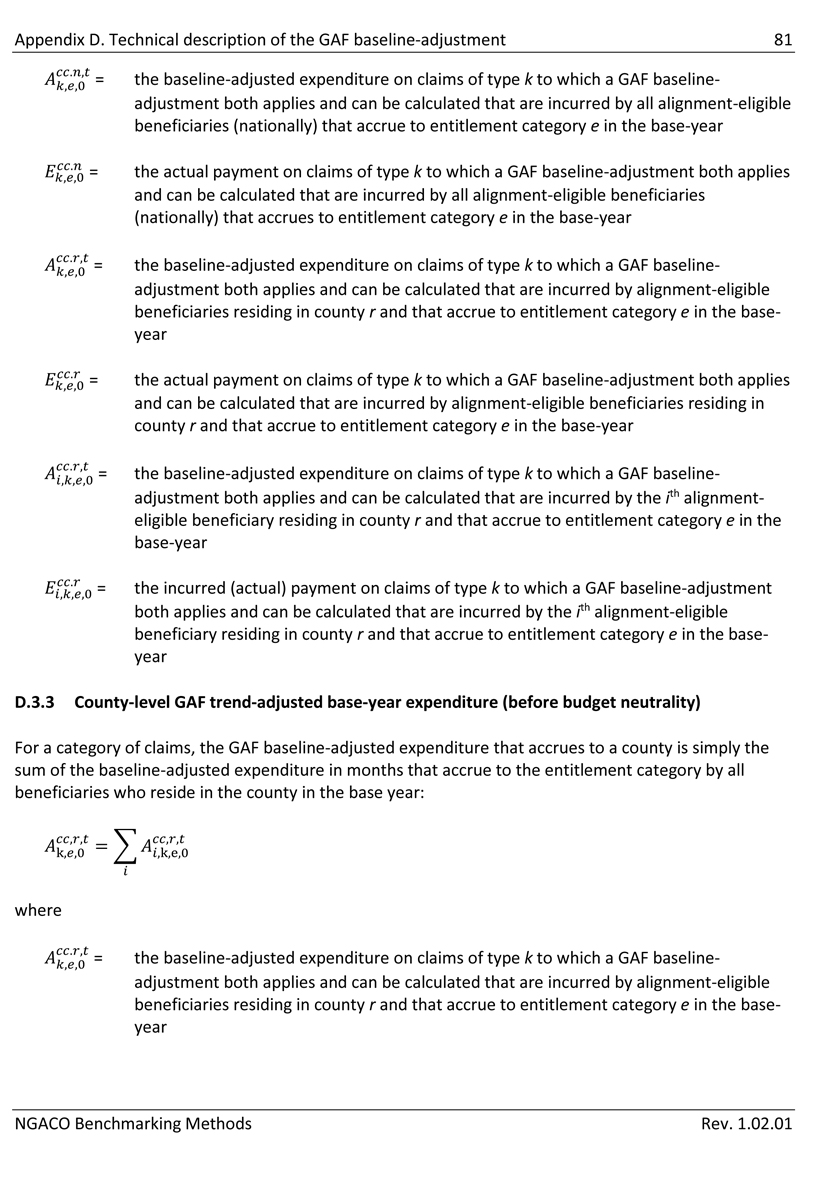
Appendix D. Technical description of the GAF baseline-adjustment 81 = the baseline-adjusted expenditure on claims of type k to which a GAF baseline- adjustment both applies and can be calculated that are incurred by all alignment-eligible beneficiaries (nationally) that accrue to entitlement category e in the base-year = the actual payment on claims of type k to which a GAF baseline-adjustment both applies and can be calculated that are incurred by all alignment-eligible beneficiaries (nationally) that accrues to entitlement category e in the base-year = the baseline-adjusted expenditure on claims of type k to which a GAF baseline- adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base- year = the actual payment on claims of type k to which a GAF baseline-adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base-year = the baseline-adjusted expenditure on claims of type k to which a GAF baseline- adjustment both applies and can be calculated that are incurred by the ith alignment- eligible beneficiary residing in county r and that accrue to entitlement category e in the base-year = the incurred (actual) payment on claims of type k to which a GAF baseline-adjustment both applies and can be calculated that are incurred by the ith alignment-eligible beneficiary residing in county r and that accrue to entitlement category e in the base- year D.3.3 County-level GAF trend-adjusted base-year expenditure (before budget neutrality) For a category of claims, the GAF baseline-adjusted expenditure that accrues to a county is simply the sum of the baseline-adjusted expenditure in months that accrue to the entitlement category by all beneficiaries who reside in the county in the base year: where = the baseline-adjusted expenditure on claims of type k to which a GAF baseline- adjustment both applies and can be calculated that are incurred by alignment-eligible beneficiaries residing in county r and that accrue to entitlement category e in the base- year NGACO Benchmarking Methods Rev. 1.02.01
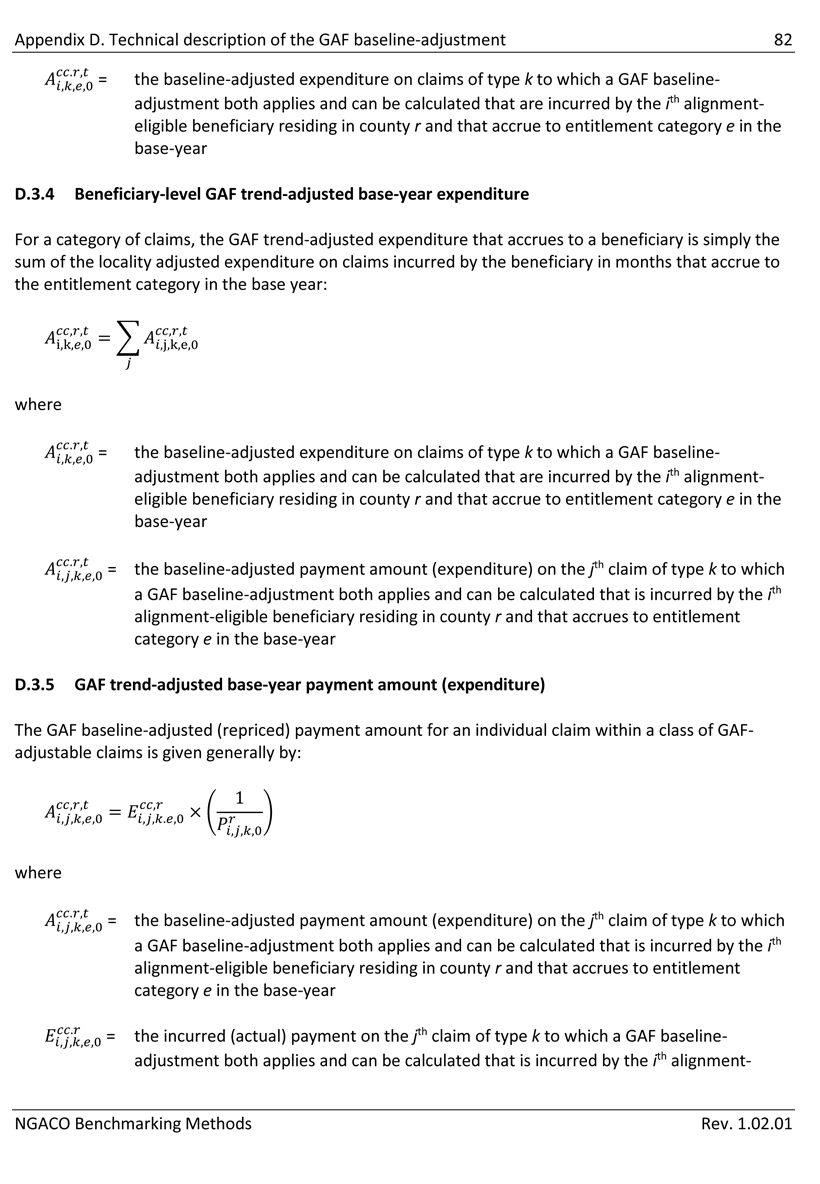
Appendix D. Technical description of the GAF baseline-adjustment 82 = the baseline-adjusted expenditure on claims of type k to which a GAF baseline- adjustment both applies and can be calculated that are incurred by the ith alignment- eligible beneficiary residing in county r and that accrue to entitlement category e in the base-year D.3.4 Beneficiary-level GAF trend-adjusted base-year expenditure For a category of claims, the GAF trend-adjusted expenditure that accrues to a beneficiary is simply the sum of the locality adjusted expenditure on claims incurred by the beneficiary in months that accrue to the entitlement category in the base year: where = the baseline-adjusted expenditure on claims of type k to which a GAF baseline- adjustment both applies and can be calculated that are incurred by the ith alignment- eligible beneficiary residing in county r and that accrue to entitlement category e in the base-year = the baseline-adjusted payment amount (expenditure) on the jth claim of type k to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year D.3.5 GAF trend-adjusted base-year payment amount (expenditure) The GAF baseline-adjusted (repriced) payment amount for an individual claim within a class of GAF- adjustable claims is given generally by: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k to which a GAF baseline- adjustment both applies and can be calculated that is incurred by the ith alignment- NGACO Benchmarking Methods Rev. 1.02.01
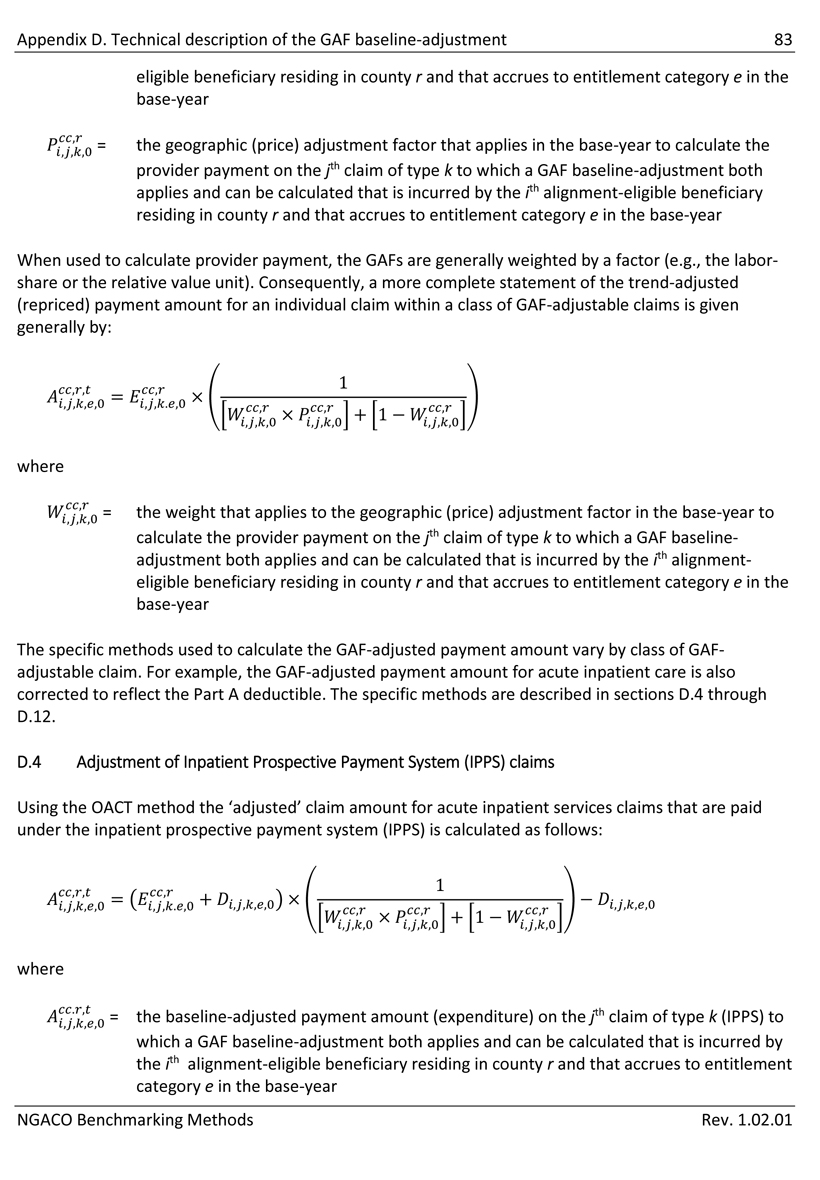
Appendix D. Technical description of the GAF baseline-adjustment 83 eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the geographic (price) adjustment factor that applies in the base-year to calculate the provider payment on the jth claim of type k to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year When used to calculate provider payment, the GAFs are generally weighted by a factor (e.g., the labor- share or the relative value unit). Consequently, a more complete statement of the trend-adjusted (repriced) payment amount for an individual claim within a class of GAF-adjustable claims is given generally by: where = the weight that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k to which a GAF baseline- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The specific methods used to calculate the GAF-adjusted payment amount vary by class of GAF- adjustable claim. For example, the GAF-adjusted payment amount for acute inpatient care is also corrected to reflect the Part A deductible. The specific methods are described in sections D.4 through D.12. D.4 Adjustment of Inpatient Prospective Payment System (IPPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (IPPS) is calculated as follows: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k (IPPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
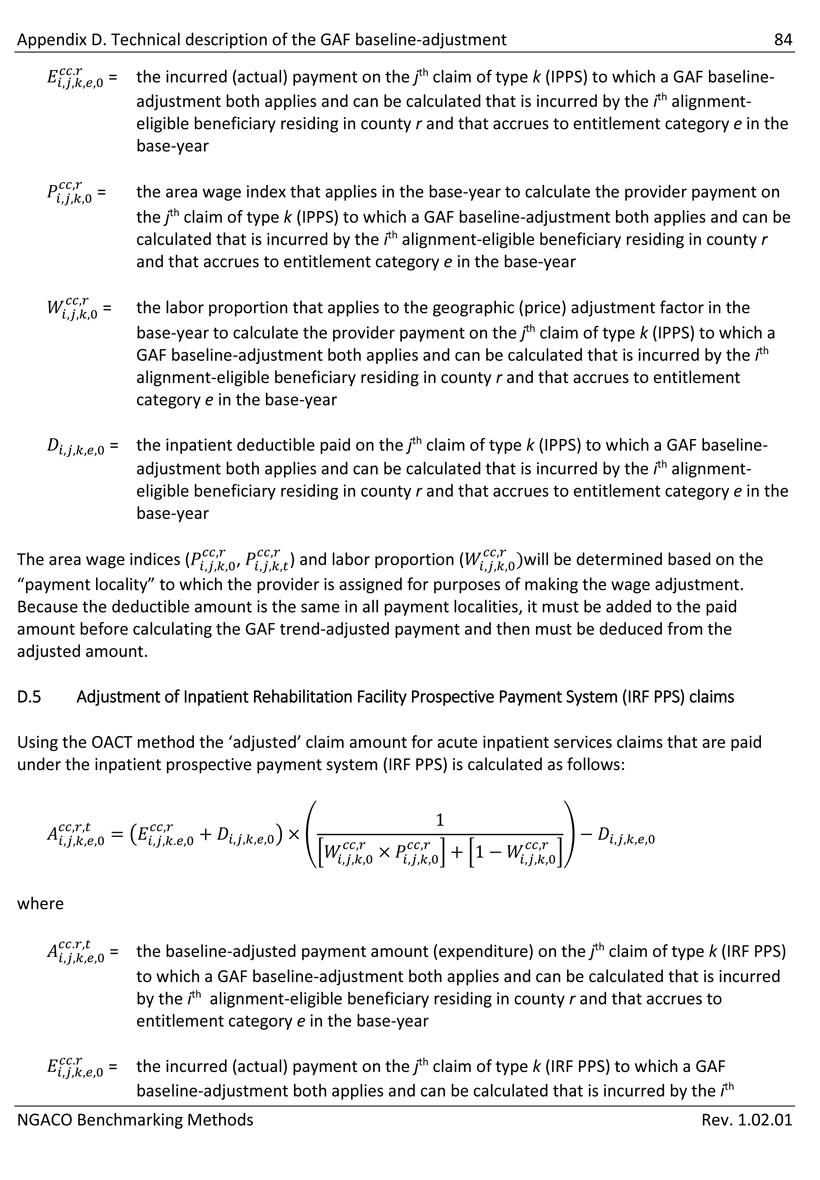
Appendix D. Technical description of the GAF baseline-adjustment 84 = the incurred (actual) payment on the jth claim of type k (IPPS) to which a GAF baseline- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (IPPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (IPPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the inpatient deductible paid on the jth claim of type k (IPPS) to which a GAF baseline- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Because the deductible amount is the same in all payment localities, it must be added to the paid amount before calculating the GAF trend-adjusted payment and then must be deduced from the adjusted amount. D.5 Adjustment of Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (IRF PPS) is calculated as follows: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k (IRF PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (IRF PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith NGACO Benchmarking Methods Rev. 1.02.01
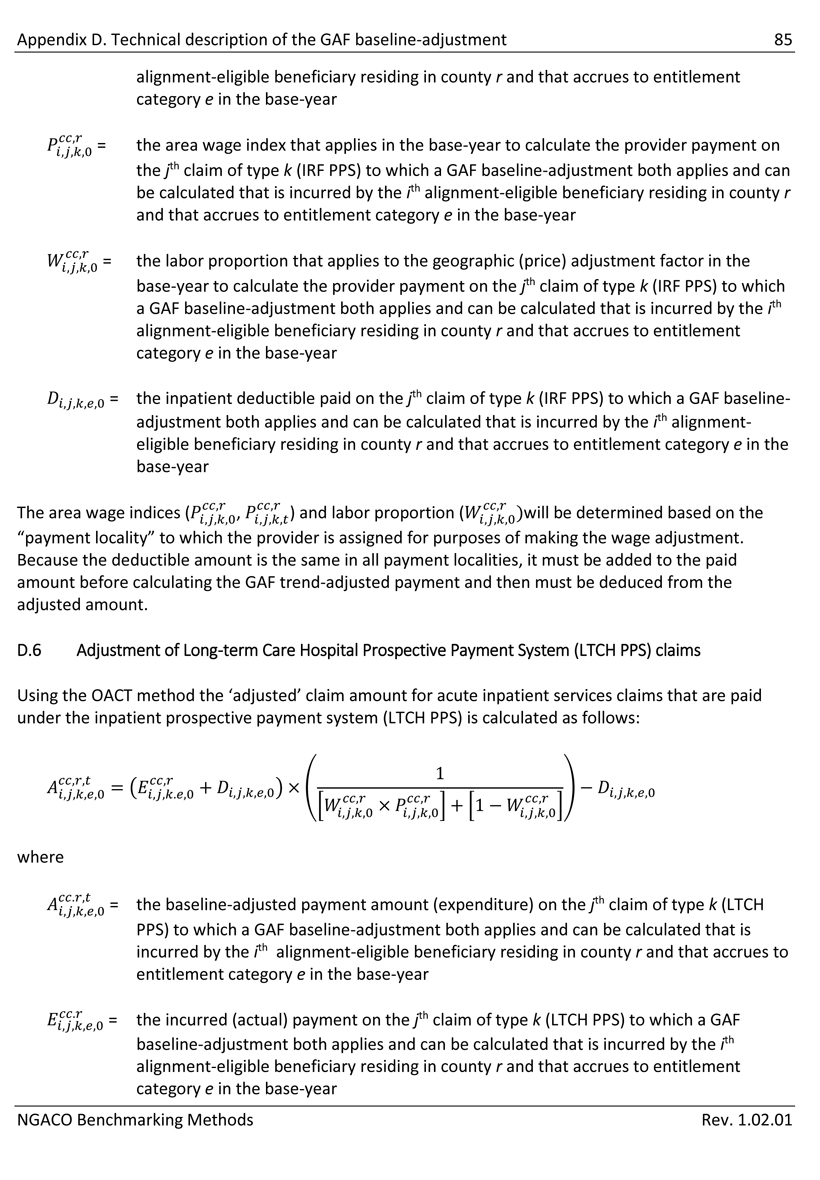
Appendix D. Technical description of the GAF baseline-adjustment 85 alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (IRF PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (IRF PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the inpatient deductible paid on the jth claim of type k (IRF PPS) to which a GAF baseline- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Because the deductible amount is the same in all payment localities, it must be added to the paid amount before calculating the GAF trend-adjusted payment and then must be deduced from the adjusted amount. D.6 Adjustment of Long-term Care Hospital Prospective Payment System (LTCH PPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (LTCH PPS) is calculated as follows: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k (LTCH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (LTCH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
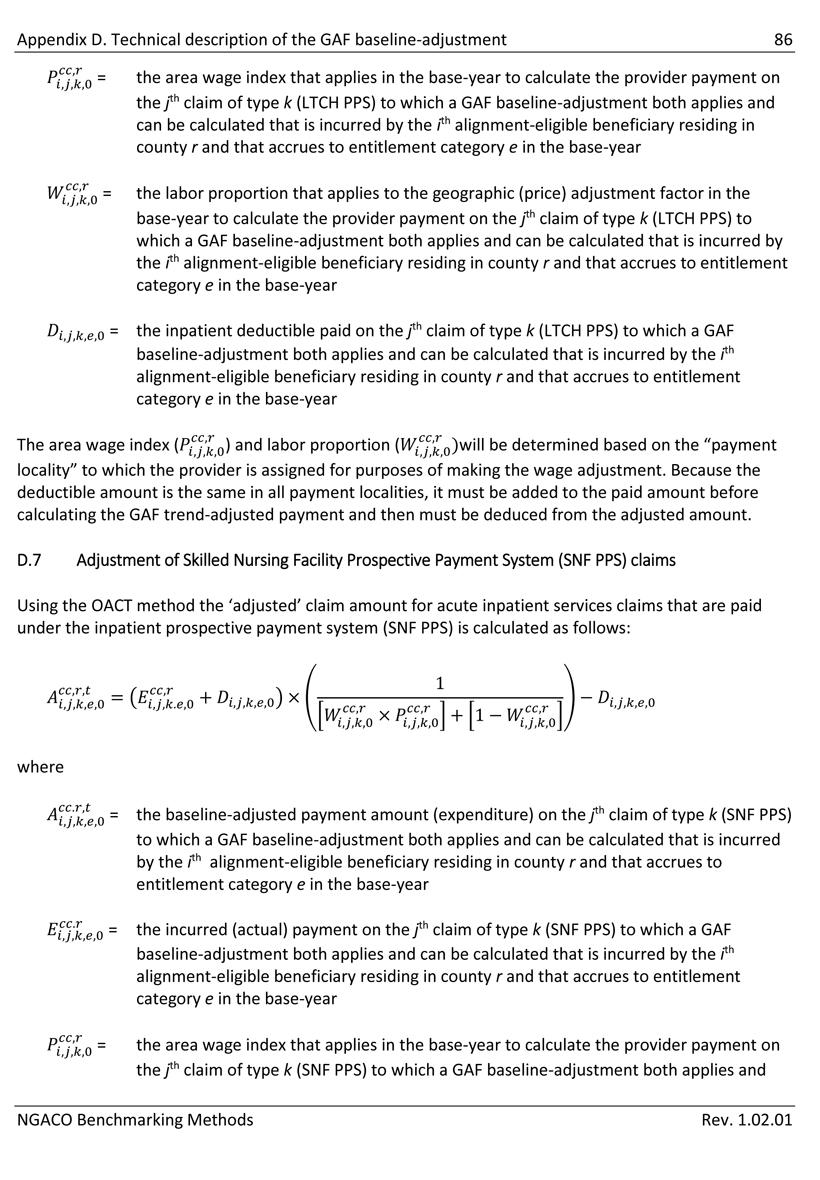
Appendix D. Technical description of the GAF baseline-adjustment 86 = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (LTCH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (LTCH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the inpatient deductible paid on the jth claim of type k (LTCH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage index () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Because the deductible amount is the same in all payment localities, it must be added to the paid amount before calculating the GAF trend-adjusted payment and then must be deduced from the adjusted amount. D.7 Adjustment of Skilled Nursing Facility Prospective Payment System (SNF PPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (SNF PPS) is calculated as follows: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k (SNF PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (SNF PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (SNF PPS) to which a GAF baseline-adjustment both applies and NGACO Benchmarking Methods Rev. 1.02.01
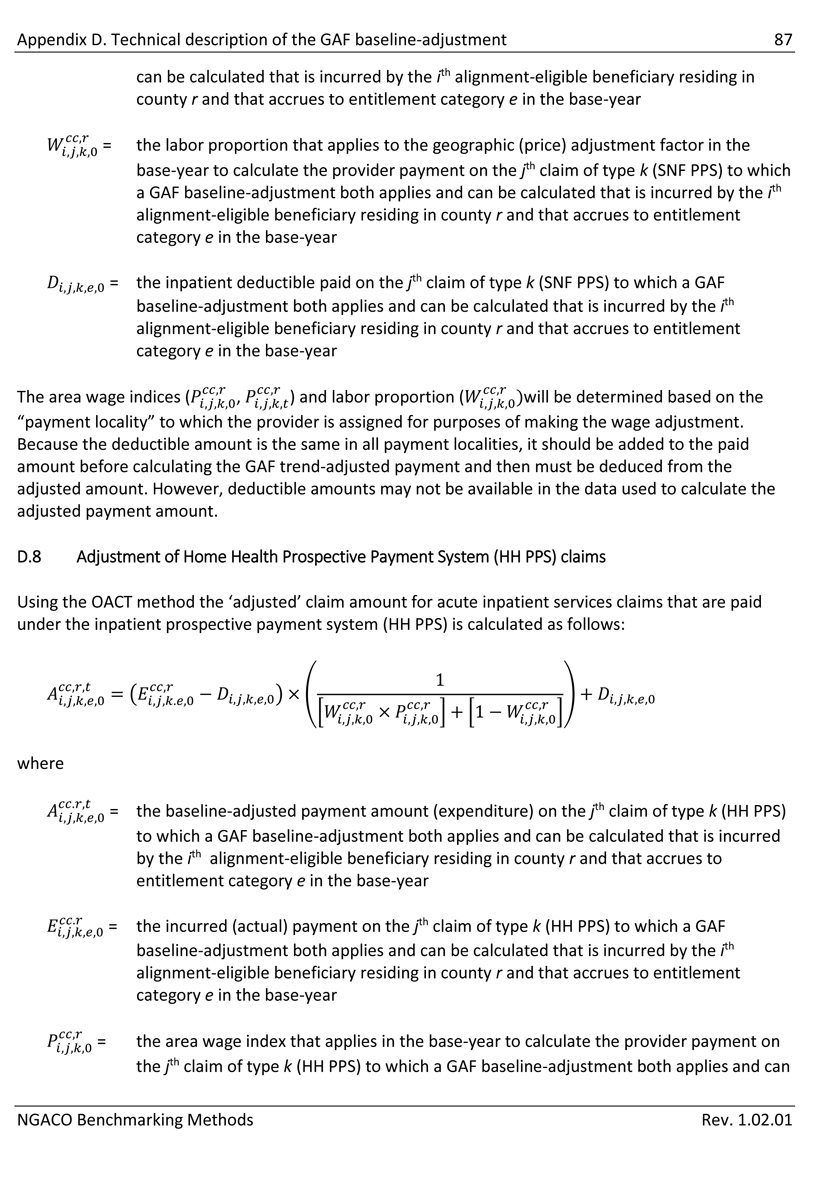
Appendix D. Technical description of the GAF baseline-adjustment 87 can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (SNF PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the inpatient deductible paid on the jth claim of type k (SNF PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Because the deductible amount is the same in all payment localities, it should be added to the paid amount before calculating the GAF trend-adjusted payment and then must be deduced from the adjusted amount. However, deductible amounts may not be available in the data used to calculate the adjusted payment amount. D.8 Adjustment of Home Health Prospective Payment System (HH PPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (HH PPS) is calculated as follows: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k (HH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (HH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (HH PPS) to which a GAF baseline-adjustment both applies and can NGACO Benchmarking Methods Rev. 1.02.01
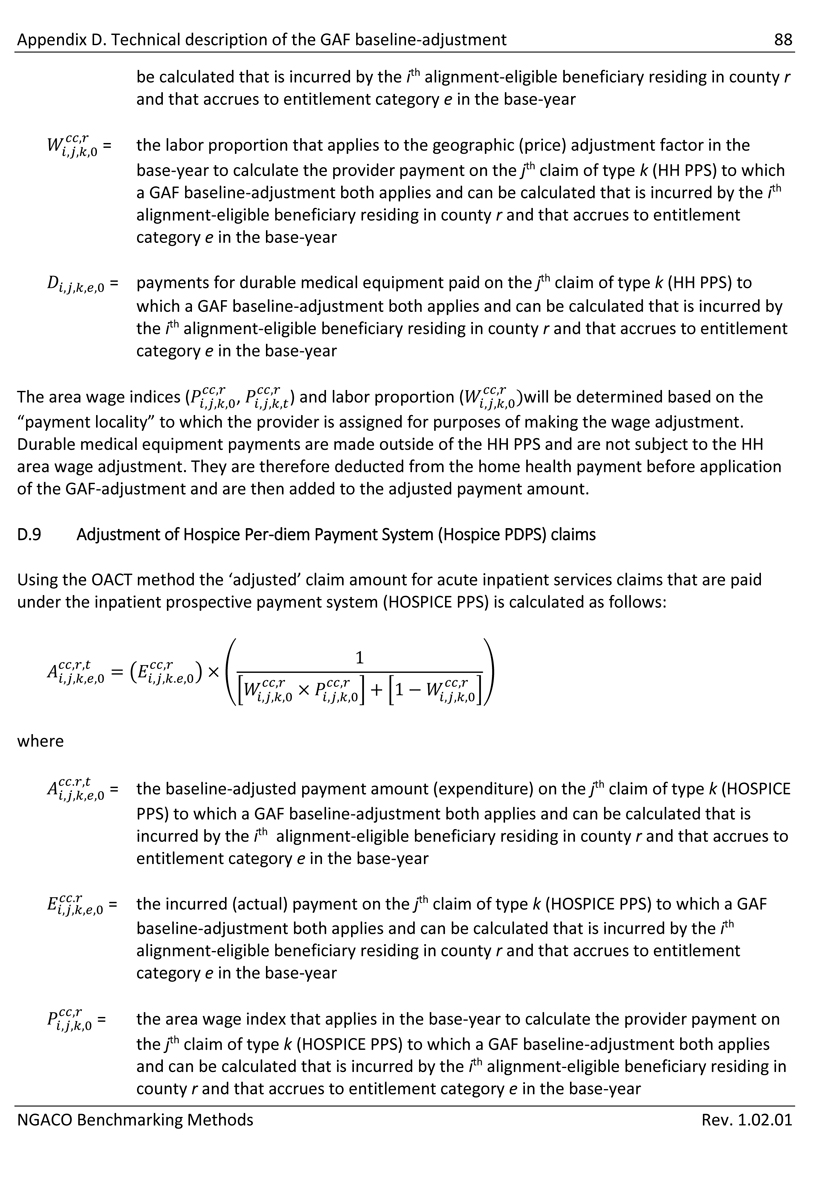
Appendix D. Technical description of the GAF baseline-adjustment 88 be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (HH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year ,0 = payments for durable medical equipment paid on the jth claim of type k (HH PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. Durable medical equipment payments are made outside of the HH PPS and are not subject to the HH area wage adjustment. They are therefore deducted from the home health payment before application of the GAF-adjustment and are then added to the adjusted payment amount. D.9 Adjustment of Hospice Per-diem Payment System (Hospice PDPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (HOSPICE PPS) is calculated as follows: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k (HOSPICE PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (HOSPICE PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (HOSPICE PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
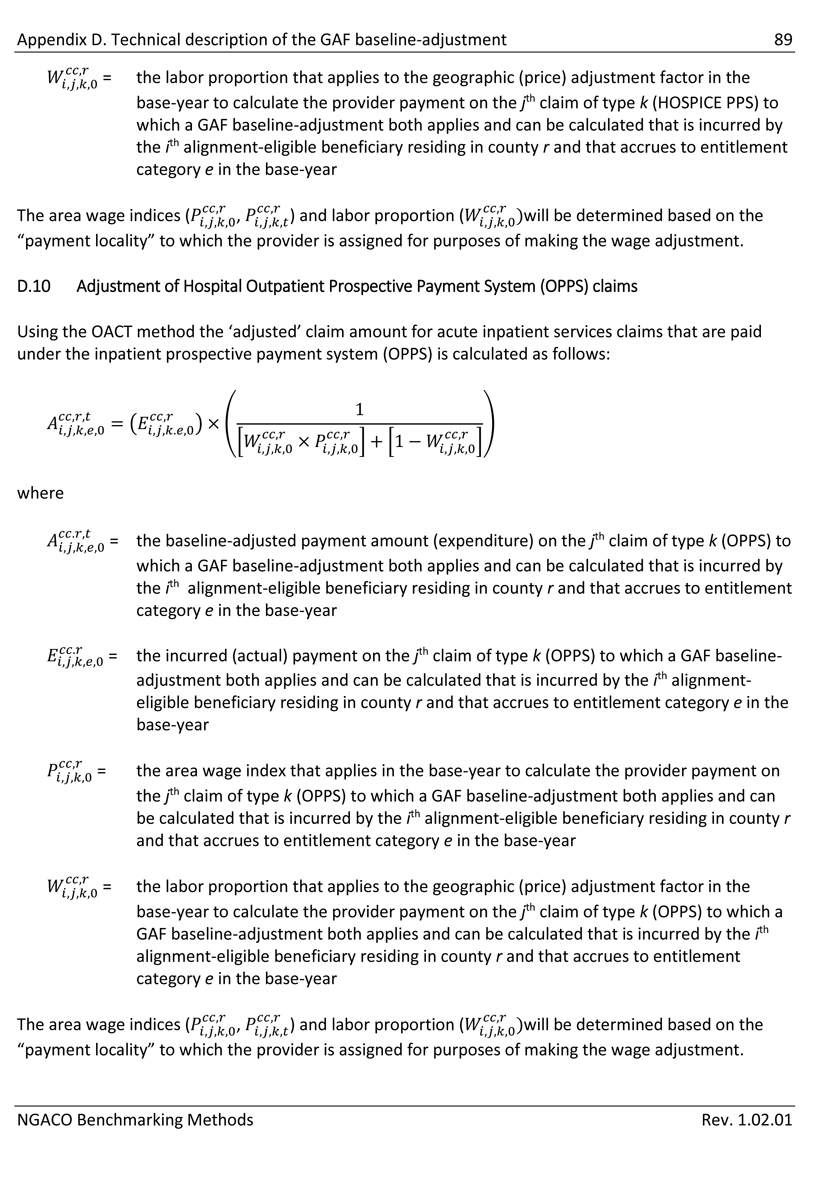
Appendix D. Technical description of the GAF baseline-adjustment 89 = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (HOSPICE PPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. D.10 Adjustment of Hospital Outpatient Prospective Payment System (OPPS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (OPPS) is calculated as follows: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k (OPPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (OPPS) to which a GAF baseline- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the area wage index that applies in the base-year to calculate the provider payment on the jth claim of type k (OPPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the labor proportion that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (OPPS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year The area wage indices () and labor proportion ()will be determined based on the “payment locality” to which the provider is assigned for purposes of making the wage adjustment. NGACO Benchmarking Methods Rev. 1.02.01
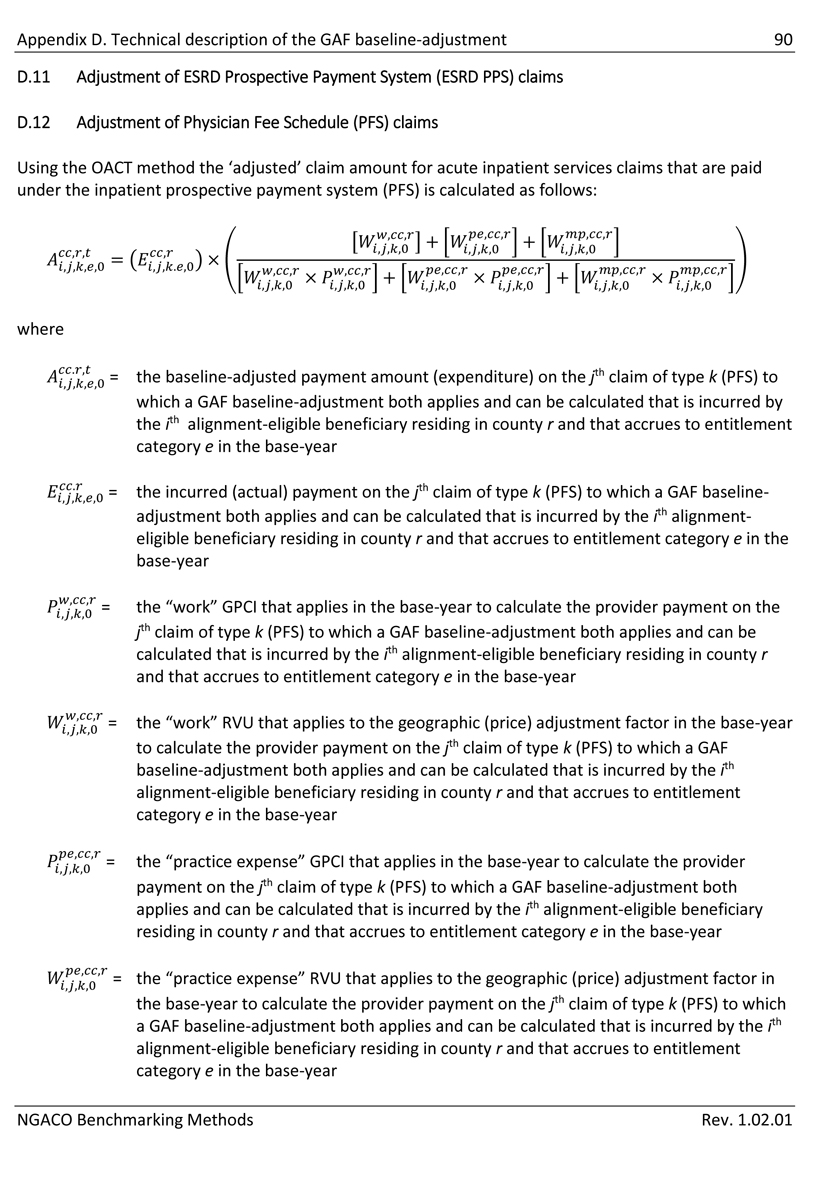
Appendix D. Technical description of the GAF baseline-adjustment 90 D.11 Adjustment of ESRD Prospective Payment System (ESRD PPS) claims D.12 Adjustment of Physician Fee Schedule (PFS) claims Using the OACT method the ‘adjusted’ claim amount for acute inpatient services claims that are paid under the inpatient prospective payment system (PFS) is calculated as follows: where = the baseline-adjusted payment amount (expenditure) on the jth claim of type k (PFS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the incurred (actual) payment on the jth claim of type k (PFS) to which a GAF baseline- adjustment both applies and can be calculated that is incurred by the ith alignment- eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “work” GPCI that applies in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “work” RVU that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “practice expense” GPCI that applies in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “practice expense” RVU that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year NGACO Benchmarking Methods Rev. 1.02.01
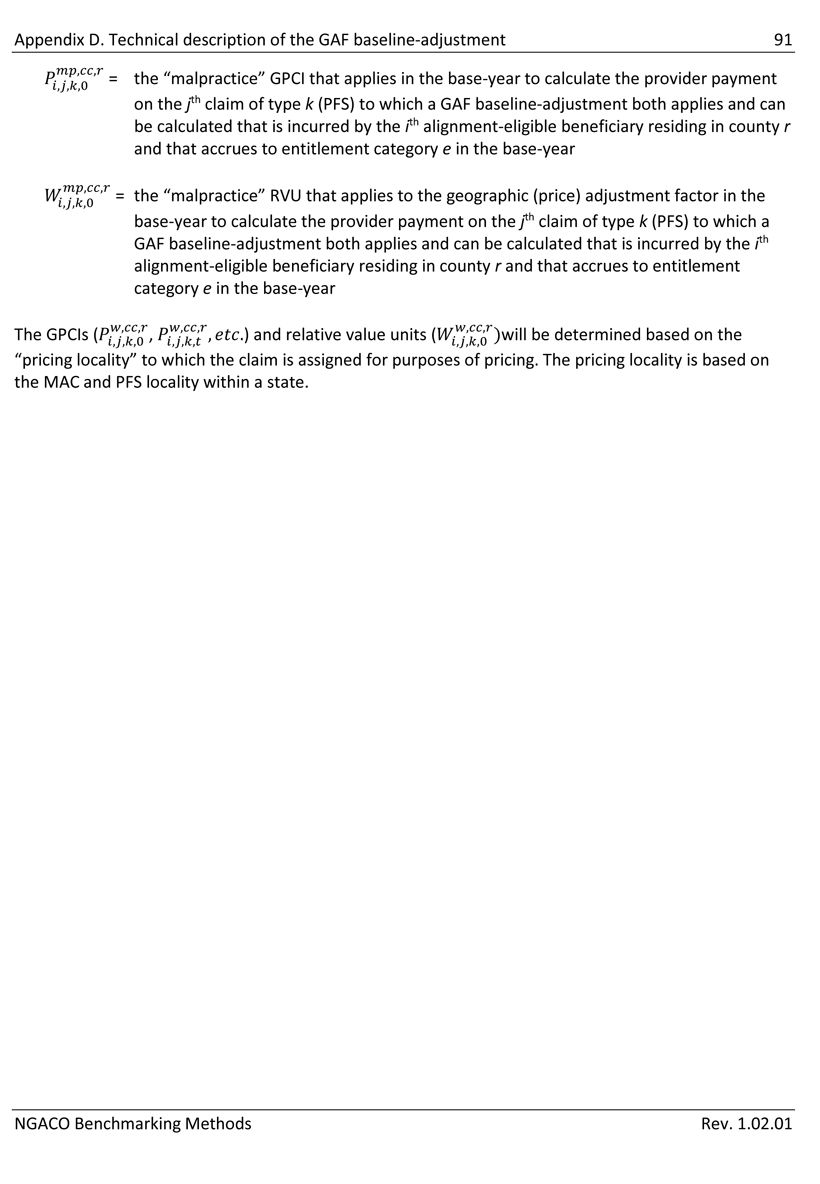
Appendix D. Technical description of the GAF baseline-adjustment 91 = the “malpractice” GPCI that applies in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year = the “malpractice” RVU that applies to the geographic (price) adjustment factor in the base-year to calculate the provider payment on the jth claim of type k (PFS) to which a GAF baseline-adjustment both applies and can be calculated that is incurred by the ith alignment-eligible beneficiary residing in county r and that accrues to entitlement category e in the base-year) and relative value units ()will be determined based on the The GPCIs ( “pricing locality” to which the claim is assigned for purposes of pricing. The pricing locality is based on the MAC and PFS locality within a state. NGACO Benchmarking Methods Rev. 1.02.01
Next Generation ACO Model Participation Agreement
Appendix C
Voluntary Alignment
| I. | General |
| A. | This Appendix C will apply only if the ACO selects participation in Voluntary Alignment pursuant to Section X of the Agreement. |
| B. | If the ACO selects participation in Voluntary Alignment, CMS shall conduct beneficiary alignment in accordance with Appendix B, except that CMS shall also align to the ACO any Medicare beneficiary eligible for voluntary alignment under Section V of this Appendix C. |
| II. | Voluntary Alignment Forms |
| A. | The ACO shall submit the following to CMS for approval by a time and in a manner specified by CMS: |
| 1. | A preliminary list identifying the Medicare Beneficiaries whom the ACO will contact regarding voluntary alignment; and |
| 2. | The criteria used by the ACO to identify such Medicare beneficiaries. |
| B. | CMS will conduct a sample audit to verify that the beneficiaries on the preliminary list satisfy the voluntary alignment eligibility requirement under Section V.A of this Appendix C. |
| C. | CMS will determine which beneficiaries on the preliminary list the ACO may contact regarding voluntary alignment and return to the ACO the final list (“Voluntary Alignment Beneficiary List”) identifying the Medicare beneficiaries that the ACO may contact regarding voluntary alignment. |
| D. | During a period starting on or after a date determined by CMS, the ACO shall provide a form (“Voluntary Alignment Form”) and instructions to all Medicare beneficiaries that are included on the Voluntary Alignment Beneficiary List. |
| E. | CMS shall determine the content of the Voluntary Alignment Forms and instructions. CMS shall provide templates for both the Voluntary Alignment Forms and instructions to the ACO. |
| F. | The ACO shall make no changes to the template forms and instructions, except for making necessary changes solely for the purpose of formatting for electronic distribution and/or receipt of submissions and for the insertion of the following information where indicated on such forms: |
| 1 |
| 1. | The name of the Medicare beneficiary’s main doctor, main provider, and/or the main place the beneficiary receives care; |
| 2. | The logo of the ACO or Next Generation Participant; |
| 3. | Information about unique care coordination and preventive services offered by the ACO as included in the beneficiary notification or as approved by CMS in accordance with Section V.E of the Agreement; |
| 4. | The ACO’s contact information for answering Medicare beneficiaries’ questions; |
| 5. | Instructions for how the Medicare beneficiary can submit the Voluntary Alignment Form to the ACO; and |
| 6. | Such other fields on the Voluntary Alignment form that CMS may identify. |
| G. | The ACO may choose to provide Voluntary Alignment Forms at the point of care only in the offices of Next Generation Participants. The ACO shall notify CMS by a date specified by CMS if the ACO elects to provide Voluntary Alignment Forms at the point of care. |
| H. | Form Requests |
| 1. | The ACO shall permit any Medicare beneficiary who is a patient of a Next Generation Participant to receive a Voluntary Alignment Form upon request. The ACO shall permit a beneficiary to request a form in person at the office of such Next Generation Participant or by calling the ACO. |
| 2. | The ACO shall permit any Medicare beneficiary who has received a Voluntary Alignment Form to request another Voluntary Alignment Form that identifies a different Next Generation Participant as the beneficiary's main doctor, main provider, or main place of care or otherwise reverses his or her voluntary alignment or that identifies a physician or other individual or entity that is not a Next Generation Participant as his or her main doctor, main provider, or main place of care or otherwise reverses his or her voluntary alignment. The ACO shall permit such requests to be made by calling the ACO. |
| 2 |
| 3. | The ACO shall permit any Medicare beneficiary that has received a Voluntary Alignment Form to request another form that allows signature by an appointed representative. Instructions on how to make this request will be included on the Voluntary Alignment Form. The ACO shall permit such requests to be made by calling the ACO. |
| I. | Maintenance of Records |
The ACO shall maintain, in accordance with Section XVIII.B of the Agreement, copies of all Voluntary Alignment Forms sent to Medicare beneficiaries (including copies of any letters sent with such forms), and, as applicable, original executed Voluntary Alignment Forms, envelopes in which Voluntary Alignment Forms were returned to the ACO, written documentation of any oral communications with a beneficiary regarding the potential or actual reversal of a Voluntary Alignment Form, all electronic data and files associated with the distribution and submission of Voluntary Alignment Forms, and all other documents, records, including beneficiary communications, regarding voluntary alignment.
| III. | Beneficiary-Next Generation Participant Communications |
| A. | The ACO, Next Generation Participants and other individuals or entities performing functions or services related to ACO Activities, may directly communicate orally with Medicare beneficiaries regarding voluntary alignment and the Voluntary Alignment Forms. |
| B. | The ACO shall require personnel at the offices of Next Generation Participants to instruct Medicare beneficiaries to call the ACO for questions about how to make changes to a Voluntary Alignment Form. |
| C. | The ACO may instruct Next Generation Participants to answer questions from beneficiaries regarding the Voluntary Alignment Form, but must prohibit them from completing the form on behalf of any beneficiary. |
| IV. | Voluntary Alignment Process |
| A. | By a date specified by CMS, the ACO shall submit to CMS a list (“Voluntary Alignment List”). The Voluntary Alignment List must contain the following: |
| 1. | The name and other required identifying information of each Medicare Beneficiary who returned one or more valid Voluntary Alignment Forms to the ACO or a Next Generation Participant (For purposes of this Appendix, a Voluntary Alignment Form is valid only if it has been signed and dated by the Medicare beneficiary or his or her appointed representative, was received by the ACO on or before the date on which the ACO submits its Voluntary Alignment List to CMS); |
| 3 |
| 2. | For each valid Voluntary Alignment Form submitted by a beneficiary, the date on which the beneficiary executed the Voluntary Alignment Form, and the identity of the Next Generation Participant that the beneficiary has identified as his or her main doctor, main provider, or main place of care; and |
| 3. | A certification by an executive of the ACO that, to the best of his or her knowledge, information, and belief, the information contained on the Voluntary Alignment List is true, accurate, and complete and identifies only those Medicare beneficiaries who have submitted a valid Voluntary Alignment Form to the ACO. |
| B. | CMS will use the Voluntary Alignment List submitted by the ACO to conduct alignment of Medicare beneficiaries for the subsequent Performance Year. |
| 1. | CMS will align Medicare beneficiaries that were included on the ACO’s Voluntary Alignment List to the ACO in accordance with the criteria set forth in Section V of this Appendix. |
| 2. | If a Medicare beneficiary returns more than one Voluntary Alignment Form to an ACO or returns such forms to multiple ACOs, CMS will honor the Voluntary Alignment Form with the latest execution date. |
| C. | CMS will audit the ACO’s Voluntary Alignment List for accuracy in accordance with Section XVII of this Agreement. |
| D. | For each Performance Year in which the ACO participates in voluntary alignment, CMS may survey Next Generation Beneficiaries as a part of the voluntary alignment audit process. |
| V. | Voluntary Alignment Eligibility Criteria |
CMS shall align a Medicare beneficiary to the ACO for a Performance Year if the following conditions are satisfied:
| A. | The Medicare beneficiary has at least one paid claim for a Qualified Evaluation and Management service, as defined in Appendix B of this Agreement, furnished by a Next Generation Participant on or after a date specified by CMS. |
| B. | On or before a deadline specified by CMS, the Pioneer ACO received a valid Voluntary Alignment Form from the Medicare beneficiary identifying a Next Generation Participant as his or her main doctor, main provider, or main place of care. |
| C. | The Medicare beneficiary has not, on or before such deadline specified by CMS, subsequently identified a physician or other individual or entity that is not a Next Generation Participant as his or her main doctor, main provider, or main place of care or otherwise reversed his or her voluntary alignment. |
| 4 |
| D. | At the time the ACO’s beneficiary alignment is conducted, the Medicare beneficiary meets the eligibility criteria set forth in Appendix B of this Agreement. |
| E. | At the time CMS conducts beneficiary alignment, CMS has not aligned the Medicare beneficiary to another model or demonstration including, but not limited to, the Independence at Home Demonstration, the Multi-payer Advanced Primary Care Practice Demonstration (MAPCP), or the Duals Demonstrations. |
| VI. | Transitioning Voluntary Alignment Decisions from Other ACO Initiatives |
If an ACO participates in a voluntary alignment process in another ACO initiative during the year prior to the ACO’s first Performance Year in the Next Generation ACO Model, CMS will align Medicare beneficiaries that were included on the ACO’s Voluntary Alignment List (or equivalent record of beneficiary submissions used in the other initiative) for the performance year under the other initiative that corresponds with the ACO’s first Performance Year in the Next Generation ACO Model to the ACO in accordance with the criteria set forth in Section V of this Appendix C.
| 5 |
Next Generation ACO Model Participation Agreement
Appendix D
HIPAA-Covered Disclosure Request Attestation and Data Specification Worksheet
| I. | HIPAA-Covered Disclosure Request Attestation |
The ACO requests the CMS data listed in the Data Specification Worksheet below and makes the following assertions regarding its ability to meet the HIPAA requirements for receiving such data:
The ACO is (select one):
| o | A HIPAA Covered Entity (CE) as defined in 45 CFR § 160.103. |
| o | The business associate (BA) of a HIPAA CE as defined in 45 CFR § 160.103. |
| o | Neither a HIPAA CE nor a BA of a HIPAA CE. |
The ACO is seeking protected health information (PHI), as defined in 45 CFR § 160.103 (select one):
| o | For its own use. |
| o | On behalf of a CE for which the ACO is a BA. |
| o | Other: Please attach a description of the intended purpose (e.g., for “research” purposes, for “public health” purposes, etc.). |
The ACO requests (select one):
| o | For the Medicare beneficiaries that have been aligned to the ACO under the Model using the methodology described in this Agreement: (i) three years of historical data files for the data elements identified in the Data Specification Worksheet; and (ii) monthly claims data files for the duration of the ACO’s participation in the Model for the data elements identified in the Data Specification Worksheet, from the following CMS data files: |
| File | Years(s) | System of Record | ||
| HIGLAS - Payment Data | 2008-2011 | N/A | ||
| NLR - Meaningful Use Data | 2008-2011 | NCH (71 FR 67137 / 11/20/2006) | ||
| RAS - Risk Adjustment Data | 2008-2011 | IDR (71 FR 74915 / 12/13/2006) | ||
| CAHPS - Beneficiary Survey Data | 2008-2011 | IDR (71 FR 74915 / 12/13/2006) | ||
| GPRO - Quality Measurement Data | 2008-2011 | NCH (71 FR 67137 / 11/20/2006) | ||
| NPICS - NPI Crosswalk | 2008-2011 | NPS (63 FR 40297 / 7/28/1998) | ||
| PECOS - Provider Enrollment Data | 2008-2011 | PECOS (71 FR 60536/ 10/13/2006) | ||
| CME - Beneficiary Enrollment Data | 2008-2011 | EDB (73 FR 10249 / 2/26/2008) | ||
| IDR - Parts A, B, and D Claims | 2008-2011 | IDR (71 FR 74915 / 12/13/2006) |
| 1 |
| o | Other: Please attach a detailed description the data requested. |
The ACO intends to use the requested data to carry out (select one):
| o | “Health care operations” that fall within the first and second paragraphs of the definition of that phrase under the HIPAA Privacy Rule (45 CFR § 164.501). |
| o | Other: Please attach a description of the intended purpose (e.g., for “research” purposes, for “public health” purposes, etc.). |
The data requested is (select one):
| o | The "minimum necessary" (as defined at 45 CFR § 164.502) to carry out the health care operations activities described above. |
| o | Other: Please attach a description of how (if applicable) the data requested exceeds what is needed to carry out the work described above. |
| The ACO’s data custodian for the requested data is: | |
| (name) | |
| (phone number) |
| By: | Date: |
| Name of authorized signatory | ||||
| Title |
| 2 |
| II. | Data Specification Worksheet |
| Data Element Source |
Data Element |
Data Element Description |
||
| Part A Claims | Current Claim Unique Identifier |
A unique identification number assigned to the claim. |
||
|
Provider OSCAR Number |
A facility’s Medicare/Medicaid identification number. It is also known as a Medicare/Medicaid Provider Number, or CCN. This number verifies that a provider has been Medicare certified for a particular type of service. | |||
| Beneficiary HIC Number |
A beneficiary identifier. |
|||
| Claim Type Code |
Signifies the type of claim being submitted through the Medicare or Medicaid programs. Claim type codes are: 10=HHA claim 20=Non swing bed SNF claim 30=Swing bed SNF claim |
|||
|
50=Hospice claim 61=Inpatient “Full-Encounter” claim |
||||
| Claim From Date | The first day on the billing statement that covers services rendered to the beneficiary. | |||
| Claim Thru Date | The last day on the billing statement that covers services rendered to the beneficiary. | |||
|
Claim Bill Facility Type Code |
The first digit of the type of bill (TOB1) is used to identify the type of facility that provided care to the beneficiary (e.g., hospital or SNF). Claim Facility Type Codes are: 1=Hospital 2=SNF 3=HHA 4=Religious non-medical (hospital) 5=Religious non-medical (extended care) 6=Intermediate care 7=Clinic or hospital-based renal dialysis facility 8=Specialty facility or Ambulatory Surgical Center (ASC) surgery 9=Reserved |
|||
|
Claim Bill Facility Type Code |
The first digit of the type of bill (TOB1) is used to identify the type of facility that provided care to the beneficiary (e.g., hospital or SNF). Claim Facility Type Codes are: 1=Hospital 2=SNF 3=HHA 4=Religious non-medical (hospital) 5=Religious non-medical (extended care) 6=Intermediate care 7=Clinic or hospital-based renal dialysis facility 8=Specialty facility or Ambulatory Surgical Center (ASC) surgery 9=Reserved |
|||
| Claim Bill Classification Code | The second digit of the type of bill (TOB2) is used to indicate with greater specificity where the service was provided (e.g., a department within a hospital). | |||
| Principal Diagnosis Code | The International Classification of Diseases (ICD)-9/10 diagnosis code identifies the beneficiary’s principal illness or disability. | |||
| Admitting Diagnosis Code | The ICD-9/10 diagnosis code identifies the illness or disability for which the beneficiary was admitted. | |||
| Claim Medicare Non Payment Reason Code |
Indicates the reason payment on an institutional claim is denied. |
|||
| Claim Payment Amount | Amount that Medicare paid on the claim. | |||
| Claim NCH Primary Payer Code | If a payer other than Medicare has primary responsibility for payment of the beneficiary’s health insurance bills, this code indicates the responsible primary payer. | |||
| Federal Information Processing Standards FIPS State Code |
Identifies the state where the facility providing services is located. |
|||
| Beneficiary Patient Status Code | Indicates the patient's discharge status as of the Claim Through Date. For example, it may indicate where a patient was discharged to (e.g., home, another facility) or the circumstances of a discharge (e.g., against medical advice, or patient death). | |||
| Diagnosis Related Group Code | Indicates the diagnostic related group to which a hospital claim belongs for prospective payment purposes. | |||
| Claim Outpatient Service Type Code |
Indicates the type and priority of outpatient service. Claim Outpatient Service Type Codes are: 0=Blank 1=Emergency |
| 3 |
|
2=Urgent 3=Elective 5-8=Reserved 9=Unknown |
||||
| Facility Provider NPI Number | Identifies the facility associated with the claim. Each facility is assigned its own unique NPI. | |||
| Operating Provider NPI Number | Identifies the operating provider associated with the claim. Each provider is assigned its own unique NPI. | |||
| Attending Provider NPI Number | Identifies the attending provider associated with the claim. Each provider is assigned its own unique NPI. | |||
| Other Provider NPI Number | Identifies the other providers associated with the claim. Each provider is assigned its own unique NPI. | |||
| Claim Adjustment Type Code | Claim adjustment types (Original, Adjustment, Deleted, Resubmitted, etc.) | |||
| Claim Effective Date | Date the claim was processed and added to the NCH. Also referred to as the NCH Weekly Processing Date. | |||
| Claim IDR Load Date | When the claim was loaded into the IDR. | |||
| Beneficiary Equitable BIC HICN Number |
This number is an “umbrella” HICN that groups certain HICNs together at the beneficiary level. |
|||
|
Claim Admission Type Code |
Indicates the type and priority of inpatient services. | |||
| Claim Admission Type Codes are: | ||||
| 0=Blank | ||||
| 1=Emergency | ||||
| 2=Urgent | ||||
| 3=Elective | ||||
| 4=Newborn | ||||
| 5=Trauma Center | ||||
| 6-8=Reserved | ||||
| 9=Unknown | ||||
| Claim Admission Source Code | Indicates the source of the beneficiary’s referral for admission or visit (e.g., a physician or another facility). | |||
| Find Admission Source Codes here: http://www.resdac.org/cms-data/variables/Claim-Source-Inpatient- Admission-Code | ||||
|
Claim Bill Frequency Code |
The third digit of the type of bill (TOB3) code. It indicates the sequence of the claim in the beneficiary's current episode of care (e.g., interim or voided). | |||
| Find Claim Frequency Codes here: http://www.resdac.org/cms-data/variables/Claim-Frequency-Code. | ||||
|
Claim Query Code |
Indicates the type of claim record being processed with respect to payment (e.g., debit/credit indicator or interim/final indicator). | |||
| Claim Query Codes are: | ||||
| 0=Credit adjustment | ||||
| 1=Interim bill | ||||
| 2=HHA benefits exhausted | ||||
| 3=Final bill | ||||
| 4=Discharge notice | ||||
| 5=Debit adjustment | ||||
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number |
The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. |
|||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
| Part A Claims Revenue Center Details | Current Claim Unique Identifier | A unique identification number assigned to the claim. | ||
| Claim Line Number | A sequential number that identifies a specific claim line | |||
| Beneficiary HIC Number | A beneficiary identifier. | |||
| Claim Type Code | Signifies the type of claim being submitted through the Medicare or Medicaid programs. | |||
| Claim type codes are: |
| 4 |
| 10=HHA claim | ||||
| 20=Non swing bed SNF claim | ||||
| 30=Swing bed SNF claim | ||||
| 40=Outpatient claim | ||||
| 50=Hospice claim | ||||
| 60=Inpatient claim | ||||
| 61=Inpatient “Full-Encounter” claim | ||||
| Claim Line From Date | The date the service associated with the line item began. | |||
| Claim Line Thru Date | The date the service associated with the line item ended. | |||
| Product Revenue Center Code | The number a provider assigns to the cost center to which a particular charge is billed (e.g., accommodations or supplies). | |||
| Claim Line Institutional Revenue Center Date |
The date that applies to the service associated with the Revenue Center code. |
|||
| HCPCS Code | The HCPCS code representing the procedure, supply, product, and/or service provided to the beneficiary. | |||
| Beneficiary Equitable BIC HICN Number |
This number is an “umbrella” HICN that groups certain HICNs together at the beneficiary level. |
|||
| Provider OSCAR Number | A facility’s Medicare/Medicaid identification number. It is also known as a Medicare/Medicaid Provider Number, or CCN. This number verifies that a provider has been Medicare certified for a particular type of service. | |||
| Claim From Date | The first day on the billing statement that covers services rendered to the beneficiary. | |||
| Claim Thru Date | The last day on the billing statement that covers services rendered to the beneficiary. | |||
| Claim Line Service Unit Quantity |
The number of dosage units of medication that were dispensed in this fill. |
|||
| Claim Line Covered Paid Amount |
The amount Medicare reimbursed the provider for covered services associated with the claim-line. |
|||
| HCPCS First Modifier Code | The first code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| HCPCS Second Modifier Code | The second code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| HCPCS Third Modifier Code | The third code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| HCPCS Fourth Modifier Code | The fourth code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| HCPCS Fifth Modifier Code | The fifth code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number |
The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. |
|||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
| Part A Procedure Codes | Current Claim Unique Identifier | A unique identification number assigned to the claim. | ||
| Beneficiary HIC Number | A beneficiary identifier. | |||
|
Claim Type Code |
Signifies the type of claim being submitted through the Medicare or Medicaid programs. | |||
| Claim type codes are: | ||||
| 10=HHA claim | ||||
| 20=Non swing bed SNF claim | ||||
| 30=Swing bed SNF claim | ||||
| 40=Outpatient claim | ||||
| 50=Hospice claim | ||||
| 60=Inpatient claim |
| 5 |
| 61=Inpatient “Full-Encounter” claim | ||||
| Claim Value Sequence Number | An arbitrary sequential number that uniquely identifies a procedure code record within the claim. | |||
| Procedure Code | The ICD-9/10 code that indicates the procedure performed during the period covered by the claim. | |||
| Procedure Performed Date | The date the indicated procedure was performed. | |||
| Beneficiary Equitable BIC HICN Number | This number is an “umbrella” HICN that groups certain HICNs together at the beneficiary level. | |||
| Provider OSCAR Number | A facility’s Medicare/Medicaid identification number. It is also known as a Medicare/Medicaid Provider Number, or CCN. This number verifies that a provider has been Medicare certified for a particular type of service. | |||
| Claim From Date | The first day on the billing statement that covers services rendered to the beneficiary. | |||
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number | The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. | |||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
| Part A Diagnosis Codes | Current Claim Unique Identifier | A unique identification number assigned to the claim. | ||
| Claim Value Sequence Number | An arbitrary sequential number that uniquely identifies a procedure code record within the claim. | |||
| Claim Product Type Code | Codes classifying the diagnosis category: | |||
| E=Accident diagnosis code | ||||
| 1=First diagnosis E code | ||||
| D=Other diagnosis codes | ||||
| Beneficiary HIC Number | A beneficiary identifier. | |||
| Claim Type Code | Signifies the type of claim being submitted through the Medicare or Medicaid programs. | |||
| Claim type codes are: | ||||
| 10=HHA claim | ||||
| 20=Non swing bed SNF claim | ||||
| 30=Swing bed SNF claim | ||||
| 40=Outpatient claim | ||||
| 50=Hospice claim | ||||
| 60=Inpatient claim | ||||
| 61=Inpatient “Full-Encounter” claim | ||||
| Diagnosis Code | The ICD-9/10 diagnosis code identifying the beneficiary’s illness or disability. | |||
| Beneficiary Equitable BIC HICN Number | This number is an “umbrella” HICN that groups certain HICNs together at the beneficiary level. For example, if a beneficiary’s spouse becomes widowed, the HICN will change, but the Beneficiary Equitable BIC HICN will not. This groups the pre- and post-widow status HICNs together. Note that the ONLY use of this field is to link together claims that all represent the same event, using the natural key. | |||
| Provider OSCAR Number | A facility’s Medicare/Medicaid identification number. It is also known as a Medicare/Medicaid Provider Number, or CCN. This number verifies that a provider has been Medicare certified for a particular type of service. | |||
| Claim From Date | The first day on the billing statement that covers services rendered to the beneficiary. | |||
| Also known as “Statement Covers From Date.” | ||||
| Claim Thru Date | The last day on the billing statement that covers services rendered to the beneficiary. | |||
| Claim Present on Admission Indicator | Indicates whether a patient had the condition listed on the claim line at the time of admission to the facility. Find Present-on-Admission values here: | |||
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number | The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. | |||
| Meta Process Date | The date the CCLF process loaded the historical record in the table |
| 6 |
| Part B Physicians | Current Claim Unique Identifier | A unique identification number assigned to the claim. | ||
| Claim Line Number | A sequential number that identifies a specific claim line | |||
| Beneficiary HIC Number | A beneficiary identifier. | |||
|
Claim Type Code |
Signifies the type of claim being submitted through the Medicare or Medicaid programs. | |||
| Claim type codes are: | ||||
| 10=HHA claim | ||||
| 20=Non swing bed SNF claim | ||||
| 30=Swing bed SNF claim | ||||
| 40=Outpatient claim | ||||
| 50=Hospice claim | ||||
| 60=Inpatient claim | ||||
| 61=Inpatient “Full-Encounter” claim | ||||
| Claim From Date | The first day on the billing statement that covers services rendered to the beneficiary. | |||
| Provider Type Code | Identifies the type of Provider Identifier. | |||
| Rendering Provider FIPS State Code |
Identifies the state that the provider providing the service is located in. |
|||
| Claim Rendering Federal Provider Specialty Code | Indicates the CMS specialty code associated with the provider of services. CMS used this number to price the service on the line-item. | |||
| Claim Federal Type Service Code | Indicates the type of service (e.g., consultation, surgery) provided to the beneficiary. Types of Service Codes are defined in the Medicare Carrier Manual. | |||
| Claim Line From Date | The date the service associated with the line item began. | |||
| Claim Line Thru Date | The date the service associated with the line item ended. | |||
| HCPCS Code | The HCPCS code representing the procedure, supply, product, and/or service provided to the beneficiary. | |||
| Claim Line Covered Paid Amount |
The amount Medicare reimbursed the provider for covered services associated with the claim-line. |
|||
| Claim Primary Payer Code | If a payer other than Medicare has primary responsibility for payment of the service indicated on the claim line, this code indicates the primary payer. This field is also known as the Line Beneficiary Primary Payer Code. | |||
| Diagnosis Code | The ICD-9/10 diagnosis code identifying the beneficiary’s principal illness or disability. | |||
| Claim Provider Tax Number | The SSN or Employee Identification Number (EIN) of the provider of the indicated service. This number identifies who receives payment for the indicated service. | |||
| Rendering Provider NPI Number | A number that identifies the provider rendering the indicated service on the claim line. Each provider is assigned its own unique NPI. | |||
| Claim Carrier Payment Denial Code |
Indicates to whom payment was made (e.g., physician, beneficiary), or if the claim was denied. |
|||
| Claim Line Processing Indicator Code |
Indicates whether the service indicated on the claim line was allowed or the reason it was denied. |
|||
| Claim Adjustment Type Code | Claim adjustment types (Original, Adjustment, Deleted, Resubmitted, etc.) | |||
| Claim Effective Date | Date the claim was processed and added to the NCH. | |||
| Claim IDR Load Date | When the claim was loaded into the IDR. | |||
| Claim Control Number | A unique number assigned to a claim by the Medicare carrier. | |||
| Beneficiary Equitable BIC HICN Number |
This number is an “umbrella” HICN that groups certain HICNs together at the beneficiary level. |
|||
| Claim Line Allowed Charges Amount |
The amount Medicare approved for payment to the provider. |
| 7 |
| Claim Line Service Unit Quantity |
The number of dosage units of medication that were dispensed in this fill. |
|||
| HCPCS First Modifier Code | The first code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| HCPCS Second Modifier Code | The second code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| HCPCS Third Modifier Code | The third code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| HCPCS Fourth Modifier Code | The fourth code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
| HCPCS Fifth Modifier Code | The fifth code to modify the HCPCS procedure code associated with the claim-line. This provides more specific procedure identification for the line item service. | |||
|
Claim Disposition Code |
Information regarding payment actions on the claim. | |||
| Claim Disposition Codes are: | ||||
| 01=Debit accepted | ||||
| 02=Debit accepted (automatic adjustment) | ||||
| 03=Cancel accepted | ||||
| Claim Diagnosis First Code | The first of eight allowable ICD-9/10 diagnosis codes identifying the beneficiary’s illness or disability. | |||
| Claim Diagnosis Second Code | The second of eight allowable ICD-9/10 diagnosis codes identifying the beneficiary’s illness or disability. | |||
| Claim Diagnosis Third Code | The third of eight allowable ICD-9/10 diagnosis codes identifying the beneficiary’s illness or disability. | |||
| Claim Diagnosis Fourth Code | The fourth of eight allowable ICD-9/10 diagnosis codes identifying the beneficiary’s illness or disability. | |||
| Claim Diagnosis Fifth Code | The fifth of eight allowable ICD-9/10 diagnosis codes identifying the beneficiary’s illness or disability. | |||
| Claim Diagnosis Sixth Code | The sixth of eight allowable ICD-9/10 diagnosis codes identifying the beneficiary’s illness or disability. | |||
| Claim Diagnosis Seventh Code | The seventh of eight allowable ICD-9/10 diagnosis codes identifying the beneficiary’s illness or disability. | |||
| Claim Diagnosis Eighth Code | The eighth of eight allowable ICD-9/10 diagnosis codes identifying the beneficiary’s illness or disability. | |||
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number |
The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. |
|||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
| Part B DMEs | Current Claim Unique Identifier | A unique identification number assigned to the claim. | ||
| Claim Line Number | A sequential number that identifies a specific claim line | |||
| Beneficiary HIC Number | A beneficiary identifier. | |||
|
Claim Type Code |
Signifies the type of claim being submitted through the Medicare or Medicaid programs. | |||
| Claim type codes are: | ||||
| 10=HHA claim | ||||
| 20=Non swing bed SNF claim | ||||
| 30=Swing bed SNF claim | ||||
| 40=Outpatient claim | ||||
| 50=Hospice claim | ||||
| 60=Inpatient claim | ||||
| 61=Inpatient “Full-Encounter” claim | ||||
| Claim From Date | The first day on the billing statement that covers services rendered to the beneficiary. | |||
| Claim Thru Date | The last day on the billing statement that covers services rendered to the beneficiary. | |||
| Claim Federal Type Service Code | Indicates the type of service (e.g., consultation, surgery) provided to the beneficiary. Types of Service Codes are defined in the Medicare Carrier Manual. |
| 8 |
| Claim Place of Service Code | Indicates the place where the indicated service was provided (e.g., ambulance, school). Places of service are defined in the Medicare Carrier Manual. | |||
| Claim Line From Date | The date the service associated with the line item began. | |||
| Claim Line Thru Date | The date the service associated with the line item ended. | |||
| HCPCS Code | The HCPCS code representing the procedure, supply, product, and/or service provided to the beneficiary. | |||
| Claim Line Covered Paid Amount |
The amount Medicare reimbursed the provider for covered services associated with the claim-line. |
|||
| Claim Primary Payer Code | If a payer other than Medicare has primary responsibility for payment of the service indicated on the claim line, this code indicates the primary payer. | |||
| Pay to Provider NPI Number | A number that identifies the provider billing for the indicated service on the claim line. Each provider is assigned its own unique NPI. | |||
| Ordering Provider NPI Number | A number that identifies the provider ordering the indicated service on the claim line. Each provider is assigned its own unique NPI. | |||
| Claim Carrier Payment Denial Code | Indicates to whom payment was made (e.g., physician, beneficiary), or if the claim was denied. | |||
| Find Carrier Payment Denial Codes here: | ||||
| Claim Line Processing Indicator Code |
Indicates whether the service indicated on the claim line was allowed or the reason it was denied. |
|||
| Claim Adjustment Type Code | Claim adjustment types (Original, Adjustment, Deleted, Resubmitted, etc.) | |||
| Claim Effective Date | Date the claim was processed and added to the NCH. Also referred to as the NCH Weekly Processing Date. | |||
| Claim IDR Load Date | When the claim was loaded into the IDR. | |||
| Claim Control Number | A unique number assigned to a claim by the Medicare carrier. | |||
| Beneficiary Equitable BIC HICN Number |
This number is an “umbrella” HICN that groups certain HICNs together at the beneficiary level. |
|||
| Claim Line Allowed Charges Amount |
The amount Medicare approved for payment to the provider. |
|||
|
Claim Disposition Code |
Information regarding payment actions on the claim. | |||
| Claim Disposition Codes are: | ||||
| 01=Debit accepted | ||||
| 02=Debit accepted (automatic adjustment) | ||||
| 03=Cancel accepted | ||||
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number |
The year and calendar month number combination in the format 'YYYYMM'. . |
|||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
| Part D | Current Claim Unique Identifier | A unique identification number assigned to the claim. | ||
| Beneficiary HIC Number | A beneficiary identifier. | |||
| NDC Code | A universal unique product identifier for human drugs. | |||
|
Claim Type Code |
Signifies the type of claim being submitted through the Medicare or Medicaid programs. | |||
| Claim type codes are: | ||||
| 10=HHA claim | ||||
| 20=Non swing bed SNF claim | ||||
| 30=Swing bed SNF claim | ||||
| 40=Outpatient claim | ||||
| 50=Hospice claim | ||||
| 60=Inpatient claim | ||||
| 61=Inpatient “Full-Encounter” claim |
| 9 |
| Claim Line From Date | The date the service associated with the line item began. | |||
|
Provider Service Identifier Qualifier Code |
Indicates the type of number used to identify the pharmacy providing the services: | |||
| 01= NPI Number | ||||
| 06=Unique Physician Identification Number (UPIN) | ||||
| 07=National Council for Prescription Drug Programs (NCPDP) Number | ||||
| 08=State License Number | ||||
| 11=TIN | ||||
| 99=Other mandatory for Standard Data Format | ||||
| Claim Service Provider Generic ID Number |
The number associated with the indicated code in the Provider Service Identification Qualifier Code field. |
|||
|
Claim Dispensing Status Code |
Indicates the status of prescription fulfillment. | |||
| Dispensing Codes are: | ||||
| P=Partially filled | ||||
| C=Completely filled | ||||
|
Claim Dispense as Written DAW Product Selection Code |
Indicates the prescriber's instructions regarding generic substitution or how those instructions were followed. | |||
| DAW Product Selection Codes are: | ||||
| 0=No product selection indicated | ||||
| 1=Substitution not allowed by prescriber | ||||
| 2=Substitution allowed – Patient requested that brand be dispensed | ||||
| 3=Substitution allowed – Pharmacist selected product dispensed | ||||
| 4=Substitution allowed – Generic not in stock | ||||
| 5=Substitution allowed – Brand drug dispensed as generic | ||||
| 6=Override | ||||
| 7=Substitution not allowed – Brand drug mandated by law | ||||
| 8=Substitution allowed – Generic drug not available in marketplace | ||||
| 9=Other | ||||
| Claim Line Service Unit Quantity |
The number of dosage units of medication that were dispensed in this fill. |
|||
| Claim Line Days’ Supply Quantity | The number of days the supply of medication dispensed by the pharmacy will cover. | |||
|
Provider Prescribing ID Qualifier Code |
The number of days the supply of medication dispensed by the pharmacy will cover. | |||
| Indicates the type of number used to identify the prescribing provider: | ||||
| 01= NPI Number | ||||
| 06= UPIN | ||||
| 07= NCPDP Number | ||||
| 08=State License Number | ||||
| 11=TIN | ||||
| 99=Other mandatory for Standard Data Format | ||||
| Claim Prescribing Provider Generic ID Number | The number associated with the indicated code in the Provider Prescribing Service Identification Qualifier Code field. | |||
| Claim Line Beneficiary Payment Amount | The dollar amount paid by the beneficiary that is not reimbursed by a third party (e.g., copayments, coinsurance, deductible or other patient pay amounts). | |||
| Claim Adjustment Type Code | Claim adjustment types (Original, Adjustment, Deleted, Resubmitted, etc.) | |||
| Claim Effective Date | Date the claim was processed and added to the NCH. Also referred to as the NCH Weekly Processing Date. | |||
| Claim IDR Load Date | When the claim was loaded into the IDR. | |||
| Claim Line Prescription Service Reference Number |
Identifies a prescription dispensed by a particular service provider on a particular service date. |
|||
| Claim Line Prescription Fill Number | Assigned to the current dispensed supply by the pharmacy. It designates the sequential order of the original fill or subsequent refills of a prescription. |
| 10 |
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number |
The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. |
|||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
| Beneficiary Demographics | Beneficiary HICN Number | This number is an “umbrella” HICN that groups certain HICNs together at the beneficiary level. | ||
| Beneficiary FIPS State Code | Identifies the state where the beneficiary receiving services resides. | |||
| Beneficiary FIPS County Code | Identifies the county where the beneficiary receiving services resides. | |||
| Beneficiary ZIP Code | The beneficiary’s ZIP code as indicated in their Medicare enrollment record. | |||
| Beneficiary Date of Birth | The month, day, and year of the beneficiary’s birth. | |||
|
Beneficiary Sex Code |
The beneficiary’s sex: | |||
| 1=Male | ||||
| 2=Female | ||||
| 0=Unknown | ||||
|
Beneficiary Race Code |
The beneficiary's race: | |||
| 0=Unknown | ||||
| 1=White | ||||
| 2=Black | ||||
| 3=Other | ||||
| 4=Asian | ||||
| 5=Hispanic | ||||
| 6=North American Native | ||||
| Beneficiary Age | The beneficiary’s current age, as calculated by subtracting the beneficiary’s date of birth from the current date. | |||
|
Beneficiary Medicare Status Code |
Indicates the reason for a beneficiary's entitlement to Medicare benefits as of a particular date, broken down by the following categories: Old Age & Survivors Insurance (OASI), Disabled, and End Stage Renal Disease (ESRD), and by appropriate combinations of these categories: | |||
| 10=Aged without ESRD | ||||
| 11=Aged with ESRD | ||||
| 20=Disabled without ESRD | ||||
| 21=Disabled with ESRD | ||||
| 31=ESRD only | ||||
| Beneficiary Dual Status Code | Identifies the most recent entitlement status of beneficiaries eligible for a program(s) in addition to Medicare (e.g., Medicaid). | |||
| Beneficiary Death Date | The month, day, and year of a beneficiary’s death. | |||
| Date beneficiary enrolled in Hospice |
The date the beneficiary enrolled in Hospice. |
|||
| Date beneficiary ended Hospice | The date the beneficiary is-enrolled in hospice. | |||
| Beneficiary First Name | The first name of the beneficiary. | |||
| Beneficiary Middle Name | The middle name of the beneficiary. | |||
| Beneficiary Last Name | The last name of the beneficiary. | |||
|
Beneficiary Original Entitlement Reason Code |
Original Reason for the beneficiary's entitlement to Medicare Benefits. | |||
| Values are: | ||||
| 0 Beneficiary insured due to age (OASI); | ||||
| 1 Beneficiary insured due to disability; | ||||
| 2 Beneficiary insured due to End Stage; Renal Disease (ESRD); | ||||
| 3 Beneficiary insured due to disability and current ESRD. | ||||
| 4. None of the above |
| 11 |
| Beneficiary Entitlement Buy In Indicator | Indicates for each month of the Denominator reference year, the entitlement of the beneficiary to Medicare Part A, Medicare Part B, or Medicare Parts A and B both, as well as whether or not the beneficiary’s state of residence was liable and paid for the beneficiary’s Medicare Part B monthly premiums. | |||
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number |
The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. |
|||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
| Beneficiary XREF | Current HIC Number | A beneficiary identifier. | ||
| Previous HIC Number | The HICN that appears in this field is the beneficiary’s previous HICN. | |||
| Previous HICN Effective Date | The date the previous HICN became active. | |||
| Previous HICN Obsolete Date | The date the previous HICN ceased to be active. | |||
| Beneficiary Railroad Board Number |
The external (to Medicare) HICN for beneficiaries that are RRB members. |
|||
| Beneficiary Surrogate Key | A IDR assigned surrogate key used to uniquely identify a beneficiary | |||
| ACO Identifier | The unique identifier of an ACO | |||
| Calendar Century Year Month Number |
The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. |
|||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
|
Summary Statistics |
ACO Identifier | The unique identifier of an ACO | ||
| File Type | The CCLF File Type | |||
| Calendar Century Year Month Number |
The year and calendar month number combination in the format 'YYYYMM'. e.g. 200701, 200702, etc. |
|||
| Meta Process Date | The date the CCLF process loaded the historical record in the table | |||
| File Description | The description of the CCLF File | |||
| Total Records Count | The total number of records in the file | |||
| Record Length | The length of the record for the file | |||
| File Name | The name the CCLF extract file that was sent to be swept by the EFT process |
| 12 |
Next Generation ACO Model Participation Agreement
Appendix F
Quality Measures
| I. | CY2016 Quality Measures |
The following quality measures are the measures for use in establishing quality performance standards in the first Performance Year of the Model (CY2016).
|
Domain |
ACO Measure # |
Measure Title |
Method
of |
Pay for Performance Phase In R—Reporting P—Performance PY1 |
||||
| AIM: Better Care for Individuals | ||||||||
| Patient / Caregiver Experience | ACO - 1 | CAHPS: Getting Timely Care, Appointments, and Information | Survey | R | ||||
| ACO - 2 | CAHPS: How Well Your Providers Communicate | Survey | R | |||||
| ACO - 3 | CAHPS: Patients' Rating of Provider | Survey | R | |||||
| ACO - 4 | CAHPS: Access to Specialists | Survey | R | |||||
| ACO - 5 | CAHPS: Health Promotion and Education | Survey | R | |||||
| ACO - 6 | CAHPS: Shared Decision Making | Survey | R | |||||
| ACO - 7 | CAHPS: Health Status/Functional Status | Survey | R | |||||
| ACO - 34 | CAHPS: Stewardship of Patient Resources | Survey | R | |||||
|
Care Coordination / Patient Safety |
ACO - 8 | Risk-Standardized, All Condition Readmission | Claims | R | ||||
| ACO - 35 | Skilled Nursing Facility 30-Day All-Cause Readmission Measure (SNFRM) | Claims | R | |||||
| ACO - 36 | All-Cause Unplanned Admissions for Patients with Diabetes | Claims | R | |||||
| ACO - 37 | All-Cause Unplanned Admissions for Patients with Heart Failure | Claims | R | |||||
| ACO - 38 | All-Cause Unplanned Admissions for Patients with Multiple Chronic Conditions | Claims | R | |||||
| ACO - 9 | Ambulatory Sensitive Conditions Admissions: Chronic Obstructive Pulmonary Disease or Asthma in Older Adults (AHRQ Prevention Quality Indicator (PQI) #5) | Claims | R | |||||
| ACO - 10 | Ambulatory Sensitive Conditions Admissions: Heart Failure (AHRQ Prevention Quality Indicator (PQI) #8 ) | Claims | R | |||||
| ACO - 39 | Documentation of Current Medications in the Medical Record | CMS Web Interface | R | |||||
| ACO - 13 | Falls: Screening for Future Fall Risk | CMS Web Interface | R | |||||
| AIM: Better Care for Populations | ||||||||
| 1 |
| Domain |
ACO Measure # |
Measure Title | Method of Data Submission |
Pay for Performance Phase In R—Reporting P—Performance PY1 |
||||
| Preventive Health | ACO - 14 | Preventive Care and Screening: Influenza Immunization | CMS Web Interface | R | ||||
| ACO - 15 | Pneumonia Vaccination Status for Older Adults | CMS Web Interface | R | |||||
| ACO - 16 | Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow Up | CMS Web Interface | R | |||||
| ACO - 17 | Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention | CMS Web Interface | R | |||||
| ACO - 18 | Preventive Care and Screening: Screening for Clinical Depression and Follow-up Plan | CMS Web Interface | R | |||||
| ACO - 19 | Colorectal Cancer Screening | CMS Web Interface | R | |||||
| ACO - 20 | Breast Cancer Screening | CMS Web Interface | R | |||||
| ACO - 21 | Preventive Care and Screening: Screening for High Blood Pressure and Follow-up Documented | CMS Web Interface | R | |||||
| ACO - 42 | Statin Therapy for the Prevention and Treatment of Cardiovascular Disease | CMS Web Interface | R | |||||
| Clinical Care for At Risk Population - Depression | ACO - 40 | Depression Remission at Twelve Months | CMS Web Interface | R | ||||
| Clinical Care for At Risk Population - Diabetes | ACO - 27 |
Diabetes Composite (All or Nothing Scoring): ACO - 27: Diabetes Mellitus: Hemoglobin A1c Poor Control ACO - 41: Diabetes: Eye Exam |
CMS Web Interface | R | ||||
| ACO - 41 | ||||||||
| Clinical Care for At Risk Population - Hypertension | ACO - 28 | Hypertension (HTN): Controlling High Blood Pressure | CMS Web Interface | R | ||||
| Clinical Care for At Risk Population - Ischemic Vascular Disease | ACO - 30 | Ischemic Vascular Disease (IVD): Use of Aspirin or Another Antithrombotic | CMS Web Interface | R | ||||
| Clinical Care for At Risk | ACO - 31 | Heart Failure (HF): Beta-Blocker Therapy for Left Ventricular Systolic Dysfunction (LVSD) | CMS Web Interface | R |
| 2 |
|
Domain |
ACO Measure # |
Measure Title |
Method
of |
Pay for Performance Phase In R—Reporting P—Performance PY1 |
||||
| Population - Heart Failure | ||||||||
| Clinical Care for At Risk Population – Coronary Artery Disease | ACO - 33 | Angiotensin-Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor Blocker (ARB) Therapy – for patients with CAD and Diabetes or Left Ventricular Systolic Dysfunction (LVEF<40%) | CMS Web Interface | R |
| 3 |
| II. | CY2017 Quality Measures |
The following quality measures are the measures for use in establishing quality performance standards in the second Performance Year of the Model (CY2017).
The column “2017 Starters (ACO PY1)” represents that all measures are pay-for- reporting (“R”) for ACOs that began participation in the Model January 1, 2017, and the column “2016 Starters (ACO PY2) represents whether the measure is pay-for-reporting (“R”) or pay-for-performance (“P”) for ACOs that began participation in the Model January 1, 2016.
|
R—Reporting P—Performance |
||||||||||
| Domain |
ACO Measure # |
Measure Title |
Method of Data Submission |
2017 Starters (ACO PY1) |
2016 Starters (ACO PY2) |
|||||
| AIM: Better Care for Individuals | ||||||||||
| Patient / Caregiver Experience | ACO - 1 | CAHPS: Getting Timely Care, Appointments, and Information | Survey | R | P | |||||
| ACO - 2 | CAHPS: How Well Your Providers Communicate | Survey | R | P | ||||||
| ACO - 3 | CAHPS: Patients' Rating of Provider | Survey | R | P | ||||||
| ACO - 4 | CAHPS: Access to Specialists | Survey | R | P | ||||||
| ACO - 5 | CAHPS: Health Promotion and Education | Survey | R | P | ||||||
| ACO - 6 | CAHPS: Shared Decision Making | Survey | R | P | ||||||
| ACO - 7 | CAHPS: Health Status/Functional Status | Survey | R | R | ||||||
| ACO - 34 | CAHPS: Stewardship of Patient Resources | Survey | R | P | ||||||
| Care Coordination / Patient Safety | ACO - 8 | Risk-Standardized, All Condition Readmission | Claims | R | R | |||||
| ACO - 35 | Skilled Nursing Facility 30-Day All-Cause Readmission Measure (SNFRM) | Claims | R | R | ||||||
| ACO - 36 | All-Cause Unplanned Admissions for Patients with Diabetes | Claims | R | R | ||||||
| ACO - 37 | All-Cause Unplanned Admissions for Patients with Heart Failure | Claims | R | R | ||||||
| ACO - 38 | All-Cause Unplanned Admissions for Patients with Multiple Chronic Conditions | Claims | R | R | ||||||
| ACO - 43 | Ambulatory Sensitive Condition Acute Composite (AHRQ Prevention Quality Indicator [PQI] #91) | Claims | R | R* | ||||||
| ACO - 44 | Use of Imaging Studies for Low Back Pain | Claims | R | R | ||||||
| ACO - 12 | Medication Reconciliation Post-Discharge | CMS Web Interface | R | R* | ||||||
| ACO -13 | Falls: Screening for Future Fall Risk | CMS Web Interface | R | P | ||||||
| AIM: Better Care for Populations | ||||||||||
| 4 |
|
R—Reporting P—Performance |
||||||||||
| Domain |
ACO Measure # |
Measure Title |
Method of Data Submission |
2017 Starters |
2016 Starters |
|||||
| Preventive Health | ACO - 14 | Preventive Care and Screening: Influenza Immunization | CMS Web Interface | R | P | |||||
| ACO - 15 | Pneumonia Vaccination Status for Older Adults | CMS Web Interface | R | P | ||||||
| ACO - 16 | Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow Up | CMS Web Interface | R | P | ||||||
| ACO - 17 | Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention | CMS Web Interface | R | P | ||||||
| ACO - 18 | Preventive Care and Screening: Screening for Clinical Depression and Follow-up Plan | CMS Web Interface | R | P | ||||||
| ACO - 19 | Colorectal Cancer Screening | CMS Web Interface | R | R | ||||||
| ACO - 20 | Breast Cancer Screening | CMS Web Interface | R | R | ||||||
| ACO - 42 | Statin Therapy for the Prevention and Treatment of Cardiovascular Disease | CMS Web Interface | R | R | ||||||
| Clinical Care for At Risk Population - Depression | ACO - 40 | Depression Remission at Twelve Months | CMS Web Interface | R | R | |||||
| Clinical Care for At Risk Population - Diabetes |
ACO – 27
ACO - 41 |
Diabetes Composite (All or Nothing Scoring): ACO - 27: Diabetes Mellitus: Hemoglobin A1c Poor Control ACO - 41: Diabetes: Eye Exam |
CMS Web Interface | R | P | |||||
| Clinical Care for At Risk Population - Hypertension | ACO - 28 | Hypertension (HTN): Controlling High Blood Pressure | CMS Web Interface | R | P | |||||
| Clinical Care for At Risk Population - Ischemic Vascular Disease (IVD) | ACO - 30 | Ischemic Vascular Disease (IVD): Use of Aspirin or Another Antithrombotic | CMS Web Interface | R | P | |||||
* Measure introduced in the 2017 Physician Fee Schedule, and will remain Pay-for-Reporting in 2017 and 2018; after that, the phase-in schedule will apply. Measure will be Pay-for-Performance for all NGACOs in the Model in 2019.
| 5 |
Next Generation ACO Model Participation Agreement
Appendix G
Alternative Payment Mechanism - Infrastructure Payments
| I. | Infrastructure Payment Election |
| A. | CMS may reject the ACO’s election to participate in Infrastructure Payments for a performance year if CMS has imposed any remedial actions pursuant to Section XIX of this Agreement, or similar remedial actions pursuant to participation in another Medicare ACO program during the two performance years prior to the applicable performance year. |
| B. | If CMS rejects the ACO’s election to participate in Infrastructure Payments for a Performance Year (in accordance with Section X.C), the ACO will defer to traditional FFS, a non-alternative payment mechanism, for the Performance Year. The ACO will not have the ability to choose another alternative payment mechanism for the Performance Year. |
| II. | Calculation |
| A. | Determining Aligned Population |
CMS will calculate the amount of the ACO’s Infrastructure Payments using an estimation of the Performance-Year aligned population, calculated as follows:
| 1. | Calibration Year Used to Estimate PY Exclusions |
CMS will use exclusions from a calibration year to estimate the proportion of initially aligned Beneficiaries that will be excluded because of alignment-eligibility requirements and service area requirements are not met and to estimate the number of person-months that each aligned Beneficiary will accrue during the Performance Year. The calibration year is the most recent calendar year for which complete data needed to perform alignment-eligibility exclusions and service area exclusions are available.
| 2. | Estimation of Performance-Year Aligned Population Person-Months |
The estimate of the number of person-months that will accrue during the Performance Year is the product of:
| a. | The number of initially aligned Beneficiaries prospectively aligned with the ACO for the Performance Year; and |
| b. | The proportion of Beneficiaries aligned in the calibration year who were excluded on the basis of alignment-eligibility and service area requirements; and |
| 1 |
| c. | The number of person-months accrued per remaining (non-excluded) aligned Beneficiary during the calibration year. |
| B. | PBPM Payment |
| 1. | If the ACO elects to participate in Infrastructure Payments through the annual selections process under Section X of this Agreement, the ACO must select the dollar amount of the per-beneficiary per-month (“PBPM”) payment. |
| 2. | The PBPM amount may not exceed $6.00 PBPM. |
| C. | Monthly Payment |
| 1. | The amount of the monthly Infrastructure Payment: |
| (a) | Is the mathematical product of the number of aligned beneficiaries in II.A and the selected PBPM amount in II.B; |
| (b) | Will be calculated by CMS prior to the start of each Performance Year in which the ACO has elected to participate in Infrastructure Payments; and |
| (c) | Will not be updated during the Performance Year. |
| 2. | CMS will make Infrastructure Payments as a monthly lump sum payment to the ACO. |
| 3. | Infrastructure Payments may be subject to budget sequestration. |
| D. | Claims Payment |
In a Performance Year in which the ACO has elected to receive Infrastructure Payments, CMS will continue to pay all claims for services furnished to Next Generation Beneficiaries as normal through the FFS claims system.
| E. | Reconciliation of Infrastructure Payments |
| 1. | The ACO shall repay CMS all Infrastructure Payments amounts received during a Performance Year as Other Monies Owed at the Performance Year settlement or through settlement reports issued at such other times as may be required under this Agreement under Section XIV. |
| 2. | Infrastructure Payments do not affect the calculation of Shared Savings/Losses, which will continue to be based on total FFS expenditures during the Performance Year for Next Generation Beneficiaries (see Appendix B for more detail). |
| 2 |
| 3. | The reconciliation of Infrastructure Payments does not affect and is not affected by the ACO’s selected risk arrangement or savings/losses cap. |
| 4. | Infrastructure Payments will be reconciled as Other Monies Owed during the Performance Year financial settlement or through a settlement report at such other time as may be required under this Agreement. |
| 5. | To reduce the number of transactions between the ACO and CMS, the amount of Infrastructure Payments owed will be added to any Shared Losses to be paid to CMS or deducted from any Shared Savings to be paid to the ACO, such that the ACO may owe CMS a payment despite earning Shared Savings. |
| 6. | Settlement and repayment of Infrastructure Payments will occur in accordance with Section XIV of this Agreement. |
| 3 |
Next Generation ACO Model
Appendix H
Alternative Payment Mechanism - Population-Based Payments (PBP)
| I. | PBP Election |
| A. | If the ACO wishes to participate in PBP, it must - |
| 1. | Timely submit to CMS its selection of PBP as an Alternative Payment Mechanism for a Performance Year in accordance with Section X.A of this Agreement; |
| 2. | Submit in accordance with Section IV of this Agreement an accurate and complete list of Next Generation Participants that have agreed to participate in PBP and an accurate and complete list of Preferred Providers that have agreed to participate in PBP; |
| 3. | Timely submit a fully executed “Next Generation ACO Model: Population-Based Payments Fee Reduction Agreement” for each Next Generation Participant and Preferred Provider that is identified as participating in PBP, as set forth on the lists submitted in accordance with Section I.A.2 of this Appendix; and |
| 4. | Submit by a date and in a manner specified by CMS a certification that the ACO has satisfied the notice and education requirement under Section II.A of this Appendix. |
| B. | CMS may reject the ACO’s election to participate in PBP for a Performance Year if: |
| 1. | CMS has taken any remedial actions pursuant to Section XIX of this Agreement; |
| 2. | CMS has taken any remedial actions against the ACO in connection with its participation in another Medicare ACO initiative during either of the ACO’s last two performance years in that initiative; |
| 3. | CMS determines on the basis of a program integrity screening or other information that the ACO’s participation in PBP might compromise the integrity of the Model; or |
| 4. | The ACO’s election to participate in PBP is for its first Performance Year in the Model and the ACO has not participated in any Medicare ACO initiative prior to its participation in the Model. |
| C. | CMS may prohibit the ACO from having a PBP Payment Arrangement (as defined in Section III of this Appendix) with a Next Generation Participant or Preferred Provider if: |
| 1. | The conduct of the Next Generation Participant or Preferred Provider has caused CMS to impose remedial action pursuant to Section XIX of this Agreement or to impose a sanction under any CMS administrative authority; or |
| 2. | CMS determines on the basis of a program integrity screening or other information that the Next Generation Participant’s or Preferred Provider’s participation in PBP might compromise the integrity of the Model. |
| 1 |
| D. | If CMS rejects or later terminates the ACO’s election to participate in PBP for a Performance Year (in accordance with Section X.C or XIX.A. of this Agreement, respectively), payments to the ACO’s Next Generation Participants and Preferred Providers will default to traditional FFS for remainder of the Performance Year. The ACO will not have the ability to choose a different Alternative Payment Mechanism for the Performance Year. |
| II. | PBP Fee Reduction |
| A. | If the ACO elects to participate in PBP for a Performance Year in accordance with Section I.A of this Appendix, the ACO shall, by a date specified by CMS, notify and educate all Next Generation Participants and Preferred Providers about the ACO’s intended participation in PBP and the associated PBP Fee Reductions. Providing a copy of the PBP Fee Reduction Agreement does not constitute notification and education for purposes of this requirement. If the ACO’s election to participate in PBP for a Performance year is rejected, the ACO shall notify all Next Generation Participants and Preferred Providers that it is not participating in PBP for that Performance Year. |
| B. | A Next Generation Participant or Preferred Provider may participate in PBP for a Performance Year only if the Next Generation Participant or Preferred Provider was included on the ACO’s Participant List or Preferred Provider List, respectively, at the start of that Performance Year. Next Generation Participants and Preferred Providers who were added to the ACO’s Participant List or Preferred Provider List during a Performance Year may participate in PBP in a subsequent Performance Year only if they are included on the ACO’s Participant List or Preferred Provider List at the start of the subsequent Performance Year. |
| C. | Not all Next Generation Participants and Preferred Providers must agree to participate in PBP for the ACO to participate in PBP. |
| D. | Not all Next Generation Participants and Preferred Providers billing under a TIN must agree to participate in PBP for other Next Generation Participants and Preferred Providers billing under the same TIN to participate in PBP. |
| E. | CMS will reduce FFS payments on claims for services furnished to Next Generation Beneficiaries by the agreed PBP Fee Reduction percentage only for those Next Generation Participants and Preferred Providers that have consented to receive the PBP Fee Reduction and with whom the ACO is not prohibited under Section I.C of this Appendix from having a PBP Payment Arrangement. |
| F. | A hospital paid under the Inpatient Prospective Payment System that is a Next Generation Participant or Preferred Provider that has agreed to receive the PBP Fee Reduction will continue to receive IME, DSH, inpatient outlier, and inpatient new technology payments calculated in accordance with the applicable statutory and regulatory provisions. |
| G. | For certain types of institutional providers, such as Method II CAHs and FQHCs, that are Next Generation Participants or Preferred Providers and are participating in PBP, CMS will reduce by the agreed PBP Fee Reduction percentage all FFS payments for services furnished to Next Generation Beneficiaries that are billed under that institution’s CCN and organizational NPI regardless of whether the individual NPIs rendering the service are Next Generation Participants or Preferred Providers. |
| 2 |
| H. | Written Confirmation of Consent |
| 1. | The ACO shall obtain written confirmation that each PBP-participating Next Generation Participant or Preferred Provider has consented to receive the PBP Fee Reduction. Such written confirmation of consent must be in the form of a completed PBP Fee Reduction Agreement signed by an individual legally authorized to act for the entity through whose TIN the Next Generation Participant or Preferred Provider bills Medicare. |
| 2. | As part of the written confirmation of consent, the individual legally authorized to act for the entity through whose TIN the Next Generation Participant or Preferred Provider bills Medicare must verify the accuracy of the list of Next Generation Participants and Preferred Providers that have affirmatively consented to receiving the PBP Fee Reduction. |
| 3. | A Next Generation Participant’s or Preferred Provider’s consent to receive the PBP Fee Reduction must apply for the full Performance Year and must be renewed annually in order for the Next Generation Participant or Preferred Provider to continue to participate in PBP. |
| 4. | Consent to participate in PBP by a Next Generation Participant or Preferred Provider must be voluntary and must not be contingent on or related to receipt of referrals from the ACO, its Next Generation Participants, or Preferred Providers. |
| III. | PBP Payment Arrangement |
| A. | The ACO shall have a written payment arrangement with each PBP-participating Next Generation Participant or Preferred Provider that establishes how the ACO will compensate the PBP-participating Next Generation Participant or Preferred Provider for Covered Services that are subject to the PBP Fee Reduction (“PBP Payment Arrangement”). |
| B. | In establishing the terms of any PBP Payment Arrangement, neither party gives or receives remuneration in return for or to induce business other than business covered by the PBP Payment Arrangement. |
| C. | The compensation paid by the ACO under a PBP Payment Arrangement may not be made knowingly to induce the PBP-participating Next Generation Participant or Preferred Provider to reduce or limit Medically Necessary items or services to Beneficiaries. |
| D. | The compensation paid by the ACO under a PBP Payment Arrangement must be negotiated in good faith and may be monetary or nonmonetary, or both. |
| E. | The ACO shall maintain, in accordance with Section XVIII.B. records of all payments made pursuant to each PBP Payment Arrangement. |
| 3 |
| F. | The PBP Payment Arrangement must: |
| 1. | Require the Next Generation Participant or Preferred Provider to make Medically Necessary Covered Services available to Next Generation Beneficiaries in accordance with all applicable laws and regulations. |
| 2. | Prohibit the ACO from requiring prior authorization for services furnished to Next Generation Beneficiaries. |
| 3. | Prohibit the ACO and Next Generation Participant or Preferred Provider from interfering with a Next Generation Beneficiary’s freedom to receive Covered Services from the Medicare-enrolled provider or supplier of his or her choice, regardless of whether the provider or supplier is participating in PBP or with the ACO. |
| 4. | Require the Next Generation Participant or Preferred Provider to maintain records regarding the PBP Payment Arrangement (including records of any compensation paid under the arrangement) in accordance with Section XVIII.B of the Agreement. |
| 5. | Require the Next Generation Participant or Preferred Provider to provide the Government with access to records regarding the PBP Payment Arrangement (including records of any payments made under the arrangement) in accordance with Section XVIII.A. of the Agreement. |
| IV. | Calculation of the Population-Based Payment |
| A. | Overview |
| 1. | CMS shall calculate the Monthly PBP Payment in accordance with Section IV.B of this Appendix. |
| 2. | CMS will make a Monthly PBP Payment to the ACO for each month that the ACO participates in PBP during the Performance Year. |
| 3. | CMS shall not make any Monthly PBP Payments to the ACO after the effective date of termination of this Agreement. |
| 4. | CMS shall not make any Monthly PBP Payments after the effective date of CMS’s termination (in accordance with Section XIX.A. of this Agreement) of the ACO’s election to participate in PBP. |
| B. | PBP Payment Calculation |
| 1. | Calibration Year Used to Estimate the Reduction in FFS Payments |
CMS will use FFS payments from a calibration year to estimate the reduction in FFS payments to PBP-participating Next Generation Participants and Preferred Providers for Parts A and B services furnished to Next Generation Beneficiaries during the applicable Performance Year. The calibration year is the calendar year prior to the Performance Year.
| 4 |
| 2. | Population Used to Estimate the Reduction in FFS Payments |
The population used to estimate the reduction in FFS Payments to PBP-participating Next Generation Participants and Preferred Providers for a Performance Year consists of those Beneficiaries that would have been aligned with the ACO for the calibration year on the basis of Performance Year Next Generation Participants. This population includes Beneficiaries who were alive on January 1 of the calibration year and not enrolled in a managed care plan in January of that year. This population also includes Beneficiaries who would later have been excluded from alignment to the ACO because they did not meet alignment-eligibility requirements during the calibration year or who would have been excluded based on service-area restrictions that are applied retrospectively.
| 3. | Use of Completion Factors to Estimate PBP Monthly Payment |
| i. | CMS will use a partial year of claims experience, without run-out, to calculate the estimated reduction in FFS payments to PBP-participating Next Generation Participants and Preferred Providers because the total PBP payment amounts is generally calculated prior to or at the start of the Performance Year. |
| ii. | To adjust for run-out and claims not yet incurred, a completion factor is applied based on the experience of the most recent calendar year for which complete experience is available. The most recent calendar year for which complete experience is available is typically the calendar year that is two years prior to the Performance Year. (For example, for PY2017, the completion factor will be based on claims from CY2015 and applied to the CY2016 calibration year.) |
| iii. | A completion factor will be calculated and applied for each claim type (e.g., inpatient hospital, skilled nursing facility, home health agency, hospice, physician, and outpatient hospital service, etc.). |
| iv. | The completion factor is calculated using the ratio of total expenditures for claims paid for the completion year through December 1 of that year (e.g., December 1, 2015, for PY2017) to expenditures for claims incurred and paid for the completion factor year through a three-month run-out period into the following calendar year. (If CY2015 is the completion factor year, this would be March 31, 2016.) |
| 4. | Calculation of Total PBP Payment and Monthly PBP Payment |
The total amount of PBP payments to the ACO for a Performance Year is calculated by determining the total estimated PBP Fee Reduction for each PBP-participating Next Generation Participant and Preferred Provider, which is equal to:
| i. | The aggregate Parts A and B payments made for services rendered by all of the PBP-participating Next Generation Participants and Preferred Providers in the calibration year; |
| ii. | Multiplied by the PBP reduction for each PBP-participating Next Generation Participant or Preferred Provider; |
| iii. | Multiplied by the completion factor for the relevant claim type; |
| 5 |
| iv. | Multiplied by the ratio of the number of Next Generation Beneficiaries for the Performance Year to the number of aligned Beneficiaries for the calibration year; and |
| v. | Multiplied by 0.98 (i.e., reduced by 2%) if budget sequestration is in effect for the Performance Year. |
The resulting amount is then divided by 12 to determine the Monthly PBP payment.
| C. | PBP Payment Recalculation |
| 1. | CMS will not recalculate the total amount of the PBP payment for the Performance Year and the Monthly PBP Payment during the Performance Year, except as otherwise provided for in this section. |
| 2. | CMS will review actual PBP Fee Reductions during the Performance Year. If Performance Year performance data shows, after two quarters, that the Monthly PBP Payments for the previous quarter are at least 25% greater than or 25% less than the total actual PBP Fee Reductions taken in the previous quarter, CMS may recalculate the amount of the monthly PBP Payment calculated under Section IV.B.4 based on Performance Year data and make monthly PBP payments in this revised amounts for future months of the Performance Year. The revised Monthly PBP Payment shall be payable on a prospective basis only. CMS will provide a report of the recalculated amount to the ACO. |
| V. | Reconciliation of Total Monthly PBP Payments |
| A. | CMS will reconcile total Monthly PBP payments with total PBP Fee Reductions for each Performance Year the ACO participates in PBP, by calculating the difference between the total Monthly PBP payments CMS paid to the ACO during the Performance Year and the total PBP Fee Reductions taken during the Performance Year. Any difference will constitute Other Monies Owed and may be subject to recoupment during annual financial settlement as described in Section XIV.C of this Agreement: |
| 1. | The ACO shall pay CMS the difference in accordance with Section V.E of this Appendix if the amount CMS paid in Monthly PBP payments is greater than the total PBP Fee Reductions, and |
| 2. | CMS shall pay the ACO the difference in accordance with Section V.D of this Appendix if the amount CMS paid in Monthly PBP payments is less than the total PBP Fee Reductions. |
| B. | CMS will reconcile total Monthly PBP Payments separately from the annual financial settlement with the ACO’s benchmark under Appendix B to determine the ACO’s Shared Savings or Shared Losses. The PBP Fee Reductions do not affect the calculation of Shared Savings or Shared Losses, which will continue to be based on the amount of the FFS payments that would have been made in the absence of the PBP Fee Reduction. The reconciliation of total Monthly PBP Payments and total PBP Fee Reductions does not affect and is not affected by the sharing rate or savings/loss cap. |
| C. | During the annual financial settlement, CMS will include any Other Monies Owed due to reconciliation of total Monthly PBP Payments, with the Shared Savings or Shared Losses on the settlement report issued under Section XIV.C.1. of this Agreement, such that the settlement report will show the amount of Shared Savings or Shared Losses, the amount of Other Monies Owed by either CMS or the ACO, as well as the net amount owed by either CMS or the ACO. |
| 6 |
| D. | If the total PBP Fee Reductions exceed the total Monthly PBP Payments paid to the ACO, CMS will: |
| 1. | Add the difference to the amount paid to the ACO if the ACO has earned Shared Savings; |
| 2. | Subtract the difference from the amount of the Shared Losses owed by the ACO if the ACO owes Shared Losses; or |
| 3. | Pay the amount to the ACO as Other Monies Owed if no Shared Savings are earned and no Shared Losses are owed. |
| E. | If the total Monthly PBP Payments paid to the ACO exceed the total PBP Fee Reductions, CMS will: |
| 1. | Subtract the difference from the amount paid to the ACO if the ACO has earned Shared Savings; |
| 2. | Add the difference to the amount owed to CMS by the ACO if the ACO owes Shared Losses; or |
| 3. | Recover the difference from the ACO as Other Monies Owed if no Shared Savings are earned and no Shared Losses are owed. |
| F. | In the event that a PBP-participating ACO elects to withdraw and terminate without financial reconciliation in accordance with XIX.C.1 and XIX.D.3 of the Agreement, CMS will reconcile total Monthly PBP Payments within three (3) months after the ACO’s effective termination date, and the ACO must pay any Other Monies Owed to CMS in accordance with XIV.C.5 of the Agreement. |
| G. | CMS will include in the reconciliation of total Monthly PBP Payments any PBP Fee Reductions for services provided to Beneficiaries who were Next Generation Beneficiaries at the time the services were furnished but were later excluded from the aligned population during the Performance Year because they did not meet alignment- eligibility requirements. |
| H. | If, as a result of provider appeals or additional claims adjustments after the initial PBP reconciliation, CMS pays an amount in excess of the Reduced FFS Payment for any item or service furnished to a Next Generation Beneficiary by a Next Generation Participant or Preferred Provider participating in PBP, the ACO shall owe CMS the difference between the total amount CMS actually paid for such item or service and the total amount of the Reduced FFS Payment for such claim. Such difference would constitute Other Monies Owed and be subject to recoupment during settlement under Section XIV.C of this Agreement. |
| I. | Adjusted Settlement |
| 1. | For each Performance Year in which the ACO participates in PBP, CMS shall conduct a second PBP Reconciliation one year after the original PBP Reconciliation at the same time that CMS issues the settlement report for the subsequent Performance Year. |
| 7 |
| 2. | If, as a result of the second PBP Reconciliation, CMS determines that: |
| a. | The total PBP Fee Reductions exceeds the total amount of PBP Payments made to the ACO as Monthly PBP Payments during the Performance Year, as reconciled during the initial PBP Reconciliation for the applicable Performance Year under Section V.A of this Appendix, the difference will be deemed Other Monies Owed and CMS will pay the amount to the ACO pursuant to Section XIV.C.5 of the Agreement; |
| b. | The total amount of PBP payments made to the ACO as Monthly PBP Payments during the Performance Year, reconciled during the initial PBP Reconciliation for the applicable Performance Year under Section V.A of this Appendix, exceeds the total PBP Fee Reductions during the Performance Year, the difference will be deemed Other Monies Owed and the ACO will pay the amount to CMS pursuant to Section XIV.C.5 of the Agreement; |
| 3. | In the case of the final year of the Agreement Term or termination of the Agreement by the ACO before the date determined under Section XIX.D.3 of the Agreement: |
| a. | CMS will make reasonable efforts to conduct the second PBP Reconciliation within 12 months after the issuance of the original settlement report for the applicable Performance Year; |
| b. | CMS will issue an adjusted settlement report to the ACO setting forth the results of the second PBP Reconciliation and identifying any Other Monies Owed by the ACO to CMS, or by CMS to the ACO, as a result of this second PBP Reconciliation. |
| c. | Any amounts owed by the ACO to CMS, or by CMS to the ACO, as a result of this second PBP Reconciliation will be payable in accordance with XIV.C.5 of the Agreement. |
| 8 |
Next Generation ACO Model Participation Agreement
Appendix I
3-Day SNF Rule Waiver Benefit Enhancement
| I. | Election of the 3-Day SNF Rule Waiver Benefit Enhancement |
If the ACO wishes to offer the 3-Day SNF Rule Waiver Benefit Enhancement during a Performance Year it must –
| A. | Timely submit to CMS its election of the 3-Day SNF Rule Waiver as a Benefit Enhancement in accordance with Section X.A of this Agreement and an Implementation Plan in accordance with Section XI of this Agreement; and |
| B. | Submit in accordance with Section IV of this Agreement an accurate and complete list of Next Generation Participants that have agreed to participate in the 3-Day SNF Rule Waiver Benefit Enhancement and an accurate and complete list of Preferred Providers that have agreed to participate in the 3-Day SNF Rule Waiver Benefit Enhancement. |
| II. | Waiver |
CMS waives the requirement in section 1861(i) of the Social Security Act for a three-day inpatient hospital stay prior to the provision of otherwise covered Medicare post-hospital extended care services (“SNF Services”) furnished under the terms and conditions set forth in this Appendix (“3-Day SNF Rule Waiver”).
| III. | Eligible SNFs |
| A. | For purposes of this waiver, an “Eligible SNF” is a skilled nursing facility (“SNF”) or a hospital or critical access hospital (“CAH”) that has swing-bed approval for SNF services (“swing-bed hospital”) that is a Next Generation Participant or Preferred Provider that has (i) entered into a written agreement with the ACO to provide SNF Services in accordance with the SNF 3-Day Rule Waiver under Section II of this Appendix; (ii) been identified by the ACO as having agreed to participate in the 3-Day SNF Rule Waiver Benefit Enhancement in accordance with Section I.B of this Appendix; and (iii) been approved by CMS to participate under the 3-Day SNF Rule Waiver following a review of the qualifications of the SNF to accept admissions without a prior inpatient hospital stay (“Direct SNF Admissions”) or admissions after an inpatient stay of fewer than three days. |
| B. | CMS review and approval of a SNF to provide services in accordance with the 3-Day SNF Rule Waiver Benefit Enhancement under Section II of this Appendix includes consideration of the program integrity history of the SNF and any other factors that CMS determines may affect the qualifications of the SNF to provide SNF Services under the terms of the 3-Day SNF Rule Waiver. Additionally, at the time of CMS review and approval of the SNF to participate under the 3-Day SNF Rule Waiver, the SNF must have an overall rating of three or more stars under the CMS 5-Star Quality Rating System, as reported on the Nursing Home Compare website. |
| 1 |
| C. | Eligibility of SNFs and swing bed hospitals to provide services under this 3-Day SNF Rule Waiver will be reassessed annually, prior to the start of each Performance Year. |
| D. | The ACO shall maintain and provide to its Next Generation Participants and Preferred Providers an accurate and complete list of Eligible SNFs and shall furnish updated lists as necessary to reflect any changes in SNF eligibility. The ACO shall also furnish these lists to a Next Generation Beneficiary, upon request. |
| E. | The ACO must provide written notification to CMS within 10 days of any changes its list of Eligible SNFs. Within 10 days following the removal of any Eligible SNF from the list of Eligible SNFs, the ACO must also provide written notification to the SNF or swing-bed hospital that it has been removed from the list and that it no longer qualifies to use this 3-Day SNF Rule Waiver. |
| F. | The ACO shall provide a copy of this 3-Day SNF Rule Waiver to each Eligible SNF to which Next Generation Beneficiaries are referred. |
| IV. | Beneficiary Eligibilty Requirements |
| A. | To be eligible for reimbursement under the terms of the 3-Day SNF Rule Waiver under Section II of this Appendix the Beneficiary must be: |
| 1. | A Next Generation Beneficiary at the time of SNF admission under this waiver or within the grace period under Section VI of this Appendix; and |
| 2. | Not residing in a SNF or long-term care facility at the time of SNF admission under this waiver. For purposes of this waiver, independent living facilities and assisted living facilities shall not be deemed long-term care facilities. |
| B. | A Direct SNF Admission will be covered under the terms of the 3-Day SNF Rule Waiver under Section II of this Appendix only if, at the time of admission, the Eligible Next Generation Beneficiary: |
| 1. | Is medically stable; |
| 2. | Has confirmed diagnoses; |
| 3. | Has been evaluated by a physician or other practitioner licensed to perform the evaluation within three days prior to SNF admission; |
| 4. | Does not require inpatient hospital evaluation or treatment; and |
| 5. | Has a skilled nursing or rehabilitation need that is identified by the evaluating physician and cannot be provided as an outpatient. |
| C. | A SNF admission will be covered for a Beneficiary who is discharged to an Eligible SNF after fewer than three days of inpatient hospitalization only if at the time of admission the Beneficiary: |
| 1. | Is medically stable; |
| 2. | Has confirmed diagnoses; |
| 2 |
| 3. | Does not require further inpatient hospital evaluation or treatment; and |
| 4. | Has a skilled nursing or rehabilitation need that has been identified by a physician during the inpatient hospitalization and that cannot be provided on an outpatient basis. |
| V. | Grace Period for Excluded Beneficiaries |
In the case of a former Next Generation Beneficiary, that is, a Beneficiary who was aligned to the ACO at the start of the applicable Performance Year but who is later excluded from alignment to the ACO, CMS shall make payment for SNF Services furnished to such a Beneficiary without a prior 3 day inpatient hospitalization by an Eligible SNF under the terms of the 3-Day SNF Rule Waiver under the terms of the waiver in Section II of this Appendix as if the Beneficiary were still aligned to the ACO when the admission to the Eligible SNF occurs within 90 days following the date of the alignment exclusion and all requirements under Section IV of this Appendix are met.
| VI. | SNF Services Provided to Non-Eligible Next Generation Beneficiaries |
If an Eligible SNF provides SNF Services under this 3-Day SNF Rule Waiver to a Next Generation Beneficiary who does not meet the Beneficiary Eligibility Requirements in Section IV of this Appendix, the following rules shall apply:
| A. | CMS shall make no payment to the Eligible SNF for such services; |
| B. | The ACO shall ensure that the Eligible SNF that provided the SNF Services does not charge the Next Generation Beneficiary for the expenses incurred for such services; |
| C. | The ACO shall ensure that the Eligible SNF that provided the SNF Services returns to the Next Generation Beneficiary any monies collected from the Next Generation Beneficiary. |
| VII. | Responsibility for Denied Claims |
| A. | If a claim for any SNF Services furnished to a Beneficiary by an Eligible SNF is denied as a result of a CMS error and the Eligible SNF did not know, and could not reasonably have been expected to know, as determined by CMS, that the claim would be denied, payment shall, notwithstanding such denial, be made by CMS for such SNF Services under the terms of the waiver in Section II of this Appendix as though the coverage denial had not occurred. |
| B. | If a claim for any SNF Services furnished to a Beneficiary by an Eligible SNF is denied for any reason other than a CMS error and CMS determines that that the Eligible SNF did not know, and could not reasonably have been expected to know, that payment would not be made for such items or services under Part A or Part B of Title XVIII: |
| 1. | CMS shall, notwithstanding such determination, pay for such SNF Services under the terms of the waiver in Section II of this Appendix as though the coverage denial had not occurred, but CMS will recoup these payments from the ACO. The ACO shall owe CMS the amount of any such payments, payable as Other Monies Owed for that Performance Year; |
| 3 |
| 2. | The ACO shall ensure that the Eligible SNF that provided the SNF Services does not charge the Beneficiary for the expenses incurred by such services; and |
| 3. | The ACO shall ensure that the Eligible SNF that provided the SNF Services returns to the Beneficiary any monies collected from the Beneficiary. |
| C. | If a claim for any SNF Services furnished to a Beneficiary by an Eligible SNF is denied and the Eligible SNF knew, or reasonably could be expected to have known, as determined by CMS, that payment would not be made for such items or services under Part A or Part B of Title XVIII: |
| 1. | CMS shall not make payment to the Eligible SNF for such services; |
| 2. | The ACO shall ensure that the Eligible SNF that provided the SNF Services does not charge the Beneficiary for the expenses incurred by such services; and |
| 3. | The ACO shall ensure that the Eligible SNF that provided the SNF Services returns to the Beneficiary any monies collected from the Beneficiary. |
| D. | If a Next Generation Participant or Preferred Provider that is not an Eligible SNF submits a claim for SNF Services under this 3-Day SNF Rule Waiver, furnishes services to a Beneficiary for which CMS only would have made payment if the Next Generation Participant or Preferred Provider was an Eligible SNF participating in the 3-Day SNF Rule Waiver in Section II of this Appendix at the time of service: |
| 1. | CMS shall not make payment to the Next Generation Participant or Preferred Provider for such services; |
| 2. | The ACO shall ensure that the Next Generation Participant or Preferred Provider that provided the SNF Services does not charge the Beneficiary for the expenses incurred by such services; and |
| 3. | The ACO shall ensure that the Next Generation Participant or Preferred Provider that provided the SNF Services returns to the Beneficiary any monies collected from the Beneficiary. |
| VIII. | Compliance and Enforcement |
| A. | CMS may revoke its approval of a Next Generation Participant or Preferred Provider to participate as an Eligible SNF under the 3-Day SNF Rule Waiver Benefit Enhancement at any time if the Next Generation Participant or Preferred Provider’s continued participation in this 3-Day SNF Rule Waiver Benefit Enhancement might compromise the integrity of the Model. |
| B. | The ACO must have appropriate procedures in place to ensure that Next Generation Participants and Preferred Providers have access to the most up-to-date information regarding Next Generation Beneficiary alignment to the ACO. |
| C. | The ACO shall submit quarterly reports to CMS, in a manner to be determined by CMS, regarding its use of the 3-Day SNF Rule Waiver under Section II of this Appendix. The ACO shall provide CMS with supplemental information upon request regarding its use of the 3-Day SNF Rule Waiver. |
| 4 |
| D. | CMS will monitor the ACO’s use of the 3-Day SNF Rule Waiver under Section II of this Appendix to ensure that services furnished under the waiver are medically appropriate and consistent with the terms of this waiver. |
| E. | In accordance with Section XIX of the Agreement, CMS may terminate or suspend the 3- Day SNF Rule Waiver under Section II of this Appendix or take other remedial action, as appropriate, if the ACO or any of its Next Generation Participants or Preferred Providers fails to comply with the terms and conditions of the 3-Day SNF Rule Waiver. |
| F. | Notwithstanding Section XXI.D of the Agreement, CMS may amend this Appendix I without the ACO’s consent. To the extent practicable, CMS shall provide the ACO with 30 calendar days advance written notice of any such unilateral amendment, which notice shall specify the amendment’s effective date. |
| 5 |
Next Generation ACO Model Participation Agreement
Appendix J
Telehealth Expansion Benefit Enhancement
| I. | Election of the Telehealth Expansion Benefit Enhancement |
If the ACO wishes to offer the Telehealth Expansion Benefit Enhancement during a Performance Year it must –
| A. | Timely submit to CMS its election of Telehealth Expansion as a Benefit Enhancement in accordance with Section X.A of this Agreement and an Implementation Plan in accordance with Section XI of this Agreement; and |
| B. | Submit in accordance with Section IV of this Agreement an accurate and complete list of Next Generation Participants that have agreed to participate in the Telehealth Expansion Benefit Enhancement and an accurate and complete list of Preferred Providers that have agreed to participate in the Telehealth Expansion Benefit Enhancement Waiver. |
| II. | Waiver |
CMS waives the following provisions with respect to otherwise covered telehealth services furnished to a Next Generation Beneficiary by an Eligible Telehealth Provider and in such other circumstances as provided in this Appendix:
| a. | Waiver of Originating Site Requirements: CMS waives the requirements in section 1834(m)(4)(C) of the Social Security Act and 42 C.F.R. § 410.78(b)(3)–(4) with respect to telehealth services furnished in accordance with this Appendix. |
| b. | Waiver of Originating Site Requirement in the Eligible Telehealth Individual Provision: CMS waives the requirement that telehealth services be “furnished at an originating site” from section 1834(m)(4)(B) of the Social Security Act when furnished in accordance with this Appendix. |
| c. | Waiver of Originating Site Facility Fee provision: CMS waives section 1834(m)(2)(B) and 42 C.F.R. § 414.65(b) with respect to telehealth services furnished to a beneficiary at his/her home or place of residence when furnished in accordance with this Appendix. |
| III. | Eligible Telehealth Providers |
For purposes of this Telehealth Expansion Benefit Enhancement, an “Eligible Telehealth Provider” is a Next Generation Professional or Preferred Provider who is a physician or other practitioner listed at 42 C.F.R. § 410.78(b)(2) and meets the requirements under Section XI.C.2 of the Agreement.
| III. | Eligibility Requirements |
| A. | In order for telehealth services to be eligible for reimbursement under the terms of the waiver under Section II of this Appendix the Beneficiary must be located at an originating site that is either: |
| 1 |
| 1. | One of the sites listed in section 1834(m)(4)(C)(ii) of the Social Security Act; or |
| 2. | The Beneficiary’s home or place of residence. |
| B. | Claims will be denied for the following telehealth services furnished to a Beneficiary located at his/her home or place residence: |
| 1. | Follow-up inpatient telehealth consultations furnished to beneficiaries in hospitals or SNFs. HCPCS codes G0406 - G0408; |
| 2. | Subsequent hospital care services, with the limitation of one telehealth visits every three days. CPT codes 99231 – 99233; and |
| 3. | Subsequent nursing facility care services, with the limitation of one telehealth visit every 30 days. CPT codes 99307 - 99310. |
| C. | In the event that technical issues with telecommunications equipment required for telehealth services cause an inability to appropriately furnish such telehealth services, the Eligible Telehealth Provider shall not submit a claim for such telehealth services. |
| D. | All telehealth services must be furnished in accordance with all other applicable state and Federal laws and all other Medicare coverage and payment criteria, including the remaining portions of section 1834(m) of the Social Security Act and 42 C.F.R. §§ 410.78 and 414.65. |
| E. | An Eligible Telehealth Provider shall not furnish telehealth services in lieu of in person services or encourage, coerce, or otherwise influence a Next Generation Beneficiary to seek or receive telehealth services in lieu of in person services when the Eligible Telehealth Provider knows or should know in person services are medically necessary. |
| IV. | Grace Period for Excluded Beneficiaries |
In the case of a former Next Generation Beneficiary, that is, a Beneficiary who had been aligned with the ACO at the start of the applicable Performance Year and is later excluded from alignment to the ACO, CMS shall make payment for telehealth services furnished to the such a Beneficiary that occur within 90 days following the date of the alignment exclusion under the terms of the waiver in Section II of this Appendix as if the Beneficiary were still aligned to the ACO.
| V. | Responsibility for Denied Claims |
| A. | If a claim for any telehealth services furnished to a Next Generation Beneficiary by an Eligible Telehealth Provider is denied as a result of a CMS error and the Eligible Telehealth Provider did not know, and could not reasonably have been expected to know, as determined by CMS, that the claim would be denied, payment shall, notwithstanding such denial, be made by CMS for such telehealth services under the terms of the waiver in Section II of this Appendix as though the coverage denial had not occurred. |
| B. | If a claim for any telehealth services furnished to a Beneficiary by an Eligible Telehealth Provider is denied for any reason other than a CMS error and CMS determines that the Eligible Telehealth Provider did not know, and could not reasonably have been expected to know, as determined by CMS, that payment would not be made for such items or services under Part A or Part B of Title XVIII: |
| 2 |
| 1. | CMS shall, notwithstanding such denial, pay for such telehealth services under the terms of the waiver in Section II of this Appendix as though the coverage denial had not occurred, but CMS will recoup these payments from the ACO. The ACO shall owe CMS the amount of any such payments, payable as Other Monies Owed for that Performance Year; |
| 2. | The ACO shall ensure that the Eligible Telehealth Provider that provided the telehealth services does not charge the Beneficiary for the expenses incurred by such services; and |
| 3. | The ACO shall ensure that the Eligible Telehealth Provider that provided the telehealth services returns to the Beneficiary any monies collected from the Beneficiary. |
| C. | If a claim for any telehealth services furnished to a Beneficiary by an Eligible Telehealth Provider that has been identified as a provider participating in this Benefit Enhancement pursuant to Section IV of the Agreement is denied and the Eligible Telehealth Provider knew, or reasonably could be expected to have known, as determined by CMS, that payment would not be made for such items or services under Part A or Part B of Title XVIII: |
| 1. | CMS shall not make payment to the Eligible Telehealth Provider for such services; |
| 2. | The ACO shall ensure that the Eligible Telehealth Provider that provided the telehealth services does not charge the Beneficiary for the expenses incurred by such services; and |
| 3. | The ACO shall ensure that the Eligible Telehealth Provider that provided the telehealth services returns to the Beneficiary any monies collected from the Beneficiary. |
| D. | If a Next Generation Participant or Preferred Provider that is not an Eligible Telehealth Provider submits claims for telehealth services under this Telehealth Expansion Benefit Enhancement for which CMS only would have made payment if the Next Generation Participant or Preferred Provider was an Eligible Telehealth Provider participating in the this Telehealth Expansion Benefit Enhancement at the time of service: |
| 1. | CMS shall not make payment to the Next Generation Participant or Preferred Provider for such services; |
| 2. | The ACO shall ensure that the Next Generation Participant or Preferred Provider that provided the telehealth services does not charge the Beneficiary for the expenses incurred by such services; and |
| 3. | The ACO shall ensure that the Next Generation Participant or Preferred Provider that provided the telehealth returns to the Beneficiary any monies collected from the Beneficiary. |
| VI. | Compliance and Enforcement |
| A. | CMS may reject the ACO’s designation of a Next Generation Participant or Preferred Provider as an Eligible Telehealth Provider at any time if the Next Generation Participant or Preferred participate in this Telehealth Expansion Benefit Enhancement at any time if the Next Generation Participant or Preferred Provider’s participation in this Telehealth Expansion Benefit Enhancement might compromise the integrity of the Model. |
| 3 |
| B. | The ACO must have appropriate procedures in place to ensure that Next Generation Participants and Preferred Providers have access to the most up-to-date information regarding Next Generation Beneficiary alignment to the ACO. |
| C. | As a condition of this waiver, the ACO is required to submit quarterly reports to CMS, in a manner to be determined by CMS, regarding its use of this waiver and to provide CMS with supplemental information upon request regarding its use of the waiver. |
| D. | CMS will monitor the ACO’s use of the waiver under Section II of this Appendix to ensure that services furnished under the waiver are medically appropriate and consistent with the terms of the waiver. |
| E. | In accordance with Section XIX of this Agreement, CMS may terminate or suspend this waiver or take other remedial action if the ACO or any of its Next Generation Participants or Preferred Providers fails to comply with the terms and conditions of the waiver under Section II of this Appendix. |
| F. | Notwithstanding Section XXI.D of the Agreement, CMS may amend this Appendix J without the ACO’s consent. To the extent practicable, CMS shall provide the ACO with 30 calendar days advance written notice of any such unilateral amendment, which notice shall specify the amendment’s effective date. |
| 4 |
Next Generation ACO Model Participation Agreement
Appendix K
Post-Discharge Home Visits Benefit Enhancement
This Post-Discharge Home Visits Benefit Enhancement increases the availability to beneficiaries of in-home care following discharge from an acute inpatient hospital, inpatient psychiatric facility, inpatient rehabilitation facility, long-term care hospital, or skilled nursing facility by altering the supervision level for “incident to” services to allow personnel under a physician’s general supervision (instead of direct supervision) to make home visits under certain conditions.
| I. | Post-Discharge Home Visits Benefit Enhancement Election |
If the ACO wishes to offer the Post-Discharge Home Visits Benefit Enhancement during a Performance Year it must –
| A. | Timely submit to CMS its election of Post-Discharge Home Visits as a Benefit Enhancement in accordance with Section X.A of this Agreement and an Implementation Plan in accordance with Section XI of this Agreement; and |
| B. | Submit in accordance with Section IV of this Agreement an accurate and complete list of Next Generation Participants that have agreed to participate in the Post-Discharge Home Visits Benefit Enhancement and an accurate and complete list of Preferred Providers that have agreed to participate in the Post-Discharge Home Visits Benefit Enhancement. |
| II. | Waiver and Terms |
CMS waives the requirement in 42 C.F.R. § 410.26(b)(5) that services and supplies furnished incident to the service of a physician (or other practitioner) (“incident to” services) must be furnished under the direct supervision of the physician (or other practitioner)1, provided that such services are furnished as follows:
| A. | The services are furnished to a Next Generation Beneficiary who either does not qualify for Medicare coverage of home health services under 42 C.F.R. § 409.42 or who qualifies for Medicare coverage of home health services on the sole basis of living in a medically underserved area, as provided in Medicare Benefit Policy Manual, Chapter 15 § 60.4; |
| B. | The services are furnished in the Next Generation Beneficiary’s home after the beneficiary has been discharged from an acute inpatient hospital, inpatient psychiatric facility, inpatient rehabilitation facility, long-term care hospital, or skilled nursing facility; |
1 For additional guidance on “incident to” billing, the ACO may refer to the Medicare Benefit Policy Manual, Chapter 15 § 60, found at: http://www.cms.gov/Regulations-and- Guidance/Guidance/Manuals/Downloads/bp102c15.pdf, excepting the references therein to direct supervision.
| 1 |
| C. | The services are furnished by “auxiliary personnel,” as defined in 42 C.F.R. § 410.26(a)(1), under the general supervision, as defined in 42 C.F.R. § 410.32(b)(3)(i), of a Next Generation Professional or Preferred Provider identified on the ACO’s Participant List or Preferred Provider List submitted in accordance with Section IV of this Agreement as participating in the Post-Discharge Home Visits Benefit Enhancement under the terms of this Appendix who is a physician or other practitioner and meets the requirements under Section XI.D.2 of the Agreement; |
| D. | The claims for such services are billed by the supervising Next Generation Professional or Preferred Provider who is a physician or other practitioner; |
| E. | The services are furnished not more than twice: one time in the first ten (10) days following discharge and one additional time in the first thirty (30) days following discharge; and |
| F. | The two services described in Section II.E. of this Appendix cannot be accumulated: if the beneficiary is readmitted prior to receiving the second allowed service, that second allowed service is voided by the readmission and following discharge the beneficiary may receive only the two services described in Section II.E. above in connection with the most recent discharge and the provision of such services should be documented and records maintained by the ACO in accordance with Section XVIII.B. of the Agreement; and |
| G. | The services are furnished in accordance with all other applicable state and Federal laws and all other Medicare coverage and payment criteria, including the remaining provisions of 42 C.F.R. § 410.26(b). |
CMS also waives the direct supervision requirement in 42 C.F.R. § 410.26(b)(5) under such other circumstances as provided in this Appendix.
| III. | Grace Period for Excluded Beneficiaries |
In the case of a former Next Generation Beneficiary, that is, a Beneficiary who had been aligned with the ACO at the start of the applicable Performance Year and is later excluded from alignment to the ACO, CMS shall make payment the Post-Discharge Home Visits services furnished to such a Beneficiary that occur within 90 days following the date of the alignment exclusion under the terms of the waiver in Section II of this Appendix as if the Beneficiary were still aligned to the ACO.
| IV. | Responsibility for Denied Claims |
| A. | If a claim for any Post-Discharge Home Visits services furnished to a Next Generation Beneficiary by a Next Generation Professional or Preferred Provider that has been identified as a provider participating in this Benefit Enhancement pursuant to Section IV of the Agreement is denied as a result of a CMS error and the Next Generation Professional or Preferred Provider did not know, and could not reasonably have been expected to know, as determined by CMS, that the claim would be denied, payment shall, notwithstanding such denial, be made by CMS for such services (and for such period of time as CMS finds will carry out the objectives of Title XVIII) under the terms of the waiver in Section II of this Appendix as though the coverage denial had not occurred. |
| 2 |
| B. | If a claim for any Post-Discharge Home Visits services furnished to a Beneficiary by a Next Generation Professional or Preferred Provider that has been identified as provider participating in this Benefit Enhancement pursuant to Section IV of the Agreement is denied for any reason other than a CMS error and the Next Generation Professional or Preferred Provider did not know, and could not reasonably have been expected to know, as determined by CMS, that payment would not be made for such items or services under Part A or Part B of Title XVIII: |
| 1. | CMS shall, notwithstanding such determination, pay for such Post-Discharge Home Visits services under the terms of the waiver in Section II of this Appendix as though the coverage denial had not occurred, but CMS will recoup these payments from the ACO. The ACO shall owe CMS the amount of any such payments, payable as Other Monies Owed for that Performance Year; |
| 2. | The ACO shall ensure that the Next Generation Professional or Preferred Provider that provided Post-Discharge Home Visits services does not charge the Beneficiary for the expenses incurred for such services; and |
| 3. | The ACO shall ensure that the Next Generation Professional or Preferred Provider that provided the Post-Discharge Home Visits services returns to the Beneficiary any monies collected from the Beneficiary. |
| C. | If a claim for any Post-Discharge Home Visits services furnished to a Beneficiary by a Next Generation Professional or Preferred Provider that has been identified as provider participating in this Benefit Enhancement pursuant to Section IV of the Agreement is denied and the Next Generation Professional or Preferred Provider knew, or reasonably could be expected to have known, as determined by CMS, that payment would not be made for such items or services under Part A or Part B of Title XVIII: |
| 1. | CMS shall not make payment to the Next Generation Professional or Preferred Provider for such services; |
| 2. | The ACO shall ensure that the Next Generation Professional or Preferred Provider that provided the Post-Discharge Home Visits services does not charge the Beneficiary for the expenses incurred for such services; and |
| 3. | The ACO shall ensure that the Next Generation Professional or Preferred Provider that provided the Post-Discharge Home Visits services returns to the Beneficiary any monies collected from the Beneficiary. |
| D. | If a Next Generation Participant or Preferred Provider that has not been identified as participating in this Benefit Enhancement pursuant to Section IV of the Agreement furnishes Post-Discharge Home Visits services to a Beneficiary for which CMS only would have made payment if the Next Generation Participant or Preferred Provider had been identified as participating in this Benefit Enhancement at the time of service: |
| 1. | CMS shall make no payment to the Next Generation Participant or Preferred Provider for such services; |
| 3 |
| 2. | The ACO shall ensure that the Next Generation Participant or Preferred Provider that provided the Post-Discharge Home Visits services does not charge the Beneficiary for the expenses incurred for such services; and |
| 3. | The ACO shall ensure that the Next Generation Participant or Preferred Provider that provided the Post-Discharge Home Visits services returns to the Beneficiary any monies collect from the Beneficiary. |
| V. | Compliance and Enforcement |
| A. | The ACO shall ensure, through its agreement with each Next Generation Professional and Preferred Provider that will be participating in the Post-Discharge Home Visits Benefit Enhancement, that the Next Generation Professional or Preferred Provider shall require all auxiliary personnel to comply with the terms of this Agreement and Appendix. |
| B. | CMS may remove a Next Generation Professional or Preferred Provider from the list of Next Generation Professionals or Preferred Providers that may participate in this Post- Discharge Home Visits Benefit Enhancement at any time if the Next Generation Professional or Preferred Provider’s participation in this Post-Discharge Home Visits Benefits Enhancement might compromise the integrity of the Model. |
| C. | The ACO must have appropriate procedures in place to ensure that Next Generation Participants and Preferred Providers have access to the most up-to-date information regarding Next Generation Beneficiary alignment to the ACO. |
| D. | As a condition of this waiver, the ACO is required to submit quarterly reports to CMS, in a manner to be determined by CMS, regarding its use of this waiver and to provide CMS with supplemental information upon request regarding its use of the waiver. |
| E. | CMS will monitor the ACO’s use of the waiver under Section II of this Appendix to ensure that services furnished under the waiver are medically appropriate and consistent with the terms of this waiver. |
| F. | In accordance with Section XIX of this Agreement, CMS may terminate or suspend this waiver or take other remedial action if the ACO or any of its Next Generation Participants or Preferred Providers fails to comply with the terms and conditions of the waiver under Section II of this Appendix.. |
| G. | Notwithstanding Section XXI.D of the Agreement, CMS may amend this Appendix K without the ACO’s consent. To the extent practicable, CMS shall provide the ACO with 30 calendar days advance written notice of any such unilateral amendment, which notice shall specify the amendment’s effective date. |
| 4 |
Next Generation ACO Model Participation Agreement
Appendix L
Financial Guarantee
This Appendix provides requirements regarding the ACO’s financial guarantee for repayment of amounts owed to CMS as Shared Losses and/or Other Monies Owed, as required under Section XIV.D of this Agreement.
| 1. | Form of Financial Guarantee |
| 1.1. | The financial guarantee must be in one or more of the following forms: |
| (a) | Funds placed in escrow; |
| (b) | A line of credit as evidenced by a letter of credit upon which CMS may draw; |
| (c) | Surety bond. |
| 1.2. | CMS may reject any financial guarantee that does not comply with the terms of this Appendix L. |
| 1.3. | Consistent with Section XIV.D.3 of the Agreement, any changes made to a financial guarantee must be approved in advance by CMS. |
| 2. | Amount of the Financial Guarantee |
| 2.1. | For each Performance Year, the ACO shall obtain a financial guarantee in an amount equal to two percent of its total capped Medicare Parts A and B fee-for-service expenditures for beneficiaries, which represents the ACO’s baseline expenditures for the relevant Performance Year. |
| 2.2. | CMS shall provide written notice to the ACO annually of the amount that must be funded by the financial guarantee. The amount will be calculated by CMS using a financial report that will be provided to the ACO prior to the start of the Performance Year. |
| 2.3. | For each Performance Year during which the ACO participates in the Model, the ACO shall obtain a financial guarantee in the amount specified by CMS in the annual written notice furnished to the ACO under paragraph 2.2. |
| 2.4. | The ACO shall submit to CMS written documentation of the form and amount of its financial guarantee for the Performance Year for CMS review within 60 days of the date of the annual written notice furnished to the ACO under paragraph 2.2 |
| 3. | Duration of the Financial Guarantee |
| 3.1. | Except as set forth in paragraph 3.2, the financial guarantee for each Performance Year must remain in effect (or the amount funded for a Performance Year in a financial guarantee that funds multiple Performance Years must remain available to CMS) until the earliest of the earliest of the following: |
| (a) | The ACO has fully repaid CMS any Shared Losses and/or Other Monies Owed for the Performance Year; |
| (b) | CMS has exhausted the amount funded by the financial guarantee for the Performance Year and CMS determines that the ACO does not need to replenish the financial guarantee in accordance with paragraph 3.3; or |
| 1 |
| (c) | CMS determines that the ACO does not owe any Shared Losses and/or Other Monies Owed under this Model for the Performance Year. |
| 3.2. | The ACO shall maintain its financial guarantee until the earlier of the following with respect to the final Performance Year: |
| (a) | The date on which the settlement report for the final Performance Year, including any second AIPBP reconciliation or PBP reconciliation for the final Performance Year, is deemed final, if such settlement report indicates that the ACO does not owe any Shared Losses or Other Monies Owed for any Performance Year; or |
| (b) | The date on which the ACO makes payment in full for all Shared Losses or Other Monies Owed for any Performance Year. |
| 3.3. | If any portion of the financial guarantee is used to repay Shared Losses or Other Monies Owed to CMS for a Performance Year and the financial guarantee for the Performance Year must remain in effect in accordance with paragraph 3.1 or the financial guanrantee funds multiple Performance years, the ACO must, within 90 days of the date that CMS draws on the financial guarantee: (1) replenish the amount of its financial guarantee or establish another financial guarantee to ensure it maintains coverage equal to the amount required under paragraph 2.1; and (2) submit to CMS documentation demonstrating that it has complied with this provision. |
| 4. | Other requirements |
| 4.1. | Beneficiary/Obligee: The ACO shall designate CMS as the sole beneficiary or obligee of the financial guarantee. CMS’s address is 7500 Security Boulevard, Baltimore, MD 21244. |
| 4.2. | Condition for calling funds: The financial guarantee should indicate that the ACO is obligated to repay money it owes to CMS as a result of participation in the Next Generation ACO Model, citing the Next Generation ACO Participation Agreement. |
Example:
The ACO is obligated to repay money it owes to CMS under the Next Generation ACO Model, as required by the Next Generation ACO Participation Agreement. The amount of Shared Losses and/or Other Monies Owed will be noted in a demand letter to the ACO from CMS.
| 4.3. | Demand letter: The financial guarantee must allow for payment to CMS in response to a demand letter from CMS. |
| 4.4. | Account fees: Account fees or other fees associated with establishing, maintaining, or cancelling a financial guarantee are the responsibility of the ACO and must not be paid out of the principal for the financial guarantee. |
| 5. | Requirements for specific financial guarantee mechanisms |
| 5.1. | Funds placed in Escrow |
CMS and U.S. Bank National Association (“U.S. Bank”) have a standard escrow account agreement available for use between U.S. Bank, CMS, and third parties, where CMS is the recipient of funds held in escrow if payment is due to CMS. The ACO should contact the Next Generation ACO Model (as specified below) to open a U.S. Bank escrow account.
| 2 |
If the ACO wants to establish an escrow account at a different institution, CMS must approve the escrow agreement and the instructions for disbursement of the assets. Generally, CMS will accept an escrow agreement with a different institution under the following conditions:
| (a) | The funds are invested in Treasury-backed securities or a money market fund; |
| (b) | The instructions for disbursement of the assets are consistent with CMS’ standard escrow instructions (see Escrow Instructions of Depositor below); |
| (c) | The costs, fees, and expenses associated with the escrow account, including any legal expenses incurred by the escrow agent or the ACO, are not borne by CMS and such costs are not charged to principal; |
| (d) | The principal cannot be encumbered for any purpose other than repaying Shared Losses and/or Other Monies Owed by the ACO to CMS; |
| (e) | CMS is not required to indemnify any person or entity against any loss, claim, damages, liabilities, or expenses, including the costs of litigation arising from the escrow agreement or the subject of the agreement; |
| (f) | CMS will receive advance notice of early termination of the escrow account and any change in the amount of funds held in escrow. |
| 5.2. | Letter of Credit |
| (a) | CMS will generally accept a Letter of Credit under the following conditions: |
| i. | The letter of credit is irrevocable; |
| ii. | CMS is designated as the sole beneficiary; |
| iii. | The appropriate credit amount is specified; |
| iv. | The terms allow an authorized official of CMS to draw on the letter of credit upon submission to the issuing bank of the following items: (a) a certification that “The amount of the drawing under this credit represents funds due to CMS from [ACO Name] under the Next Generation ACO Model and which have remained unpaid for at least 30 days”; and (b) a copy of the appropriate written notice to the ACO of the amount owed; and |
| v. | The letter must show that CMS will receive advance notice if there is any change in the amount of credit. |
| (b) | Auto renewal clauses: ACO must not use clauses providing for the automatic renewal of an irrevocable standby letter of credit to establish the required term. The ACO may, however, use these clauses to automatically renew the letter of credit for a period of time beyond the required term. If the ACO uses an auto renewal clause, it should state that the lender will notify CMS and the ACO at least 90 days in advance if electing not to renew. |
| (c) | Sanctioned entity clauses: The bank issuing the letter of credit must omit these clauses entirely, or, if included, exclude entities sanctioned by a federal health care program or by any federal agency. |
| 5.3. | Surety Bond |
| (a) | Surety Companies: The surety bond should be issued from a company included on the U.S. Department of Treasury’s Listing of Certified (Surety Bond) Companies (https://www.fiscal.treasury.gov/fsreports/ref/suretyBnd/c570_a-z.htm). If the ACO uses a bond from a company not included on the Department of Treasury listing, it may be subject to additional scrutiny to make sure appropriate safeguards are in place. |
| (b) | Surety Bond Terms: The bond must contain: |
| 3 |
| i. | A statement that the surety is liable for assessments that occur during the term of the bond; |
| ii. | The surety's name, street address or post office box number, city, state, and zip code; and |
| iii. | A statement naming the ACO as the Principal, CMS as the Obligee, and the surety (and its heirs, executors, administrators, successors and assignees, jointly and severally) as surety. |
| 4 |
Escrow Instructions of Depositor
| 1) | Immediately upon deposit, all monies (“Assets”) held in the Account shall be invested by Agent in Treasury-backed securities. Upon deposit and at such other times as may be requested by Recipient, Agent shall notify Recipient of the date and amount of each deposit and other Account transaction. |
| 2) | Agent shall dispose of the Assets only upon written instruction from an authorized representative of Recipient. Such written instructions shall: |
| a) | Identify the amount, if any, of Shared Losses and/or Other Monies Owed incurred by the Depositor for the relevant performance year, as determined by CMS and set forth in a final settlement report, as revised if applicable, issued by CMS pursuant to Section XIV.C of the Next Generation ACO Agreement. |
| b) | Identify the amount of such Shared Losses and/or Other Monies Owed that Depositor has failed to pay (the “Debt”) within 30 days of the date of the settlement report. |
| c) | Instruct Agent to convert the Assets to cash and pay the amount of the Debt to Recipient. If the Assets will be zero after delivering the amount of the Debt to Recipient, Agent shall notify Recipient, and Recipient shall provide further instructions, in consultation with Depositor, for the replenishment of assets or closure of the Account. |
| d) | In the event of the expiration or termination of the Depositor’s Next Generation ACO Model Participation Agreement or other circumstances requiring closure of the Account, the Depositor will notify the Agent and instruct Agent to convert the Assets to cash and dispose of them as follows: |
| i) | If the Debt is zero, Agent shall return the full cash value of the Assets to Depositor, less Agent’s unpaid fees, costs and expenses. |
| ii) | If the cash value of the Assets is less than or equal to the amount of the Debt, Agent shall deliver to Recipient payment by check or wire transfer in the amount of the full cash value of the Assets. |
| iii) | If the cash value of the Assets exceeds the amount of the Debt, Agent shall deliver to Recipient payment by check or wire transfer in the amount of the Debt and shall return the remaining Assets to Depositor, less Agent’s unpaid fees, costs and expenses. |
| 3) | Upon disposition of the Assets as specified in paragraph 2(d), Agent shall close the Account and the Escrow Agreement shall terminate. |
| 4) | Unless otherwise specified by written notice of the Parties, the following persons are authorized to provide instructions from Depositor or Recipient, as the case may be, to Agent, consistent with the terms of this Agreement: |
| Depositor | |||
| Name: | |||
| Specimen Signature | |||
| Title: | |||
| Recipient |
| Name: | |||
| Specimen Signature | |||
| Title: |
| 5 |
Next Generation ACO Model Participation Agreement
Appendix M
ACO Proprietary and Confidential Information
The following are specific examples, without limitation, of what the ACO considersproprietary and confidential information currently contained in its program that should not be publicly disclosed:
1)
2)
3)
In accordance with Section XV.D of the Agreement, this information shall remain the sole property of the ACO and, except as required by federal law, shall not be released by CMS without the express written consent of the ACO.
| 1 |
Next Generation ACO Model
Appendix N
Alternative Payment Mechanism – All-Inclusive Population-Based Payments (AIPBP)
| I. | AIPBP Election |
| A. | If the ACO wishes to participate in AIPBP, it must — |
| 1. | Timely submit to CMS its selection of AIPBP as an Alternative Payment Mechanism for a Performance Year in accordance with Section X.A of this Agreement; |
| 2. | Submit in accordance with Section IV of this Agreement an accurate and complete list of Next Generation Participants that have agreed to participate in AIPBP and an accurate and complete list of Preferred Providers that have agreed to participate in AIPBP; |
| 3. | Timely submit a fully executed “Next Generation ACO Model: All-Inclusive Population-Based Payments Fee Reduction Agreement” for each Next Generation Participant and Preferred Provider that is identified as participating in AIPBP, as set forth on the lists submitted in accordance with Section I.A.2 of this Appendix; |
| 4. | Submit by a date and in a manner specified by CMS a certification that the ACO has satisfied the notice and education requirement under Section II.B of this Appendix; and |
| 5. | Submit by a date and in a manner specified by CMS a certification that the ACO has the necessary infrastructure to be able to pay its AIPBP-participating Next Generation Participants and Preferred Providers promptly in accordance with Section IV.F.2 of this Appendix. |
| B. | CMS may reject the ACO’s election to participate in AIPBP for a Performance Year if: |
| 1. | CMS has taken any remedial actions against the ACO pursuant to Section XIX of this Agreement; |
| 2. | CMS has taken any remedial actions against the ACO in connection with its participation in another Medicare ACO initiative during either of the ACO’s last two performance years in that initiative; |
| 3. | CMS determines on the basis of a program integrity screening or other information that the ACO’s participation in AIPBP might compromise the integrity of the Model; or |
| 4. | The ACO’s election to participate in AIPBP is for its first Performance Year in the Next Generation ACO Model and the ACO has not participated in any Medicare ACO initiative prior to its participation in the Model. |
| C. | CMS may prohibit the ACO from having an AIPBP Payment Arrangement (as defined in Section III of this Appendix) with a Next Generation Participant or Preferred Provider if: |
| 1 |
| 1. | The conduct of the Next Generation Participant or Preferred Provider has caused CMS to impose remedial action pursuant to Section XIX of this Agreement or to impose a sanction under any CMS administrative authority; or |
| 2. | CMS determines on the basis of a program integrity screening or other information that the Next Generation Participant’s or Preferred Provider’s Participation in AIPBP might compromise the integrity of the Model. |
| D. | If CMS rejects or later terminates the ACO’s election to participate in AIPBP for a Performance Year (in accordance with Section X.C or XIX.A of this Agreement, respectively), payments to the ACO and its Next Generation Participants and Preferred Providers will default to traditional FFS for the Performance Year. The ACO will not have the ability to choose a different Alternative Payment Mechanism for the Performance Year. |
| II. | AIPBP Fee Reduction |
| A. | If the ACO elects to participate in AIPBP for the 2017 Performance Year, Monthly AIPBP Payments to the ACO and AIPBP Fee Reductions in payments to Next Generation Participants and Preferred Providers that have agreed to accept the AIPBP Fee Reduction (100% Reduced FFS Payments) in the Performance Year will be made only for the period from April 1 through December 31, 2017. For the period from January 1 through March 31, 2017, no Monthly AIPBP Payments will be made to the ACO and no AIPBP Fee Reductions will be made to payments to Next Generation Participants and Preferred Providers who have agreed to receive the AIPBP Fee Reduction for the 2017 Performance Year. |
| B. | If the ACO has elected to participate in AIPBP for a Performance Year in accordance with Section I.A, the ACO shall, by a date specified by CMS, notify and educate all Next Generation Participants and Preferred Providers about the ACO’s intended participation in AIPBP and the associated AIPBP Fee Reduction. Providing a copy of the AIPBP Fee Reduction Agreement does not constitute notification and education for purposes of this requirement. If the ACO’s election to participate in AIPBP for a Performance Year is rejected, the ACO shall notify all Next Generation Participants and Preferred Providers that it is not participating in AIPBP for that Performance Year. |
| C. | A Next Generation Participant or Preferred Provider may participate in AIPBP for a Performance Year only if the Next Generation Participant or Preferred Provider was included on the ACO’s Participant List or Preferred Provider List, respectively, at the start of that Performance Year. Next Generation Participants and Preferred Providers who were added to the ACO’s Participant List or Preferred Provider List during a Performance Year may participate in AIPBP in a subsequent Performance Year only if they are included on the ACO’s Participant List or Preferred Provider List at the start of the subsequent Performance Year. |
| D. | Not all Next Generation Participants and Preferred Providers must agree to participate in AIPBP for the ACO to participate in AIPBP. |
| E. | Not all Next Generation Participants and Preferred Providers billing under a TIN must agree to participate in AIPBP for other Next Generation Participants and Preferred Providers billing under the same TIN to participate in AIPBP. |
| 2 |
| F. | CMS will reduce FFS Payments on claims for services furnished to Next Generation Beneficiaries by 100% only for those Next Generation Participants and Preferred Providers that have consented to receive the AIPBP Fee Reduction and with whom the ACO is not prohibited under Section I.C of this Appendix from having an AIPBP Payment Arrangement. |
| G. | A hospital paid under the Inpatient Prospective Payment System that is a Next Generation Participant or Preferred Provider that has agreed to receive the AIPBP Fee Reduction will continue to receive IME, DSH, inpatient outlier, and inpatient new technology payments calculated in accordance with the applicable statutory and regulatory provisions. |
| H. | For certain types of institutional providers, such as Method II CAHs and FQHCs, that are Next Generation Participants or Preferred Providers and are participating in AIPBP, CMS will reduce by 100% all FFS payments for services furnished to Next Generation Beneficiaries that are billed under that institution’s CCN and organizational NPI regardless of whether the individual NPIs rendering the service are Next Generation Participants or Preferred Providers. |
| I. | CMS will not reduce FFS Payments on claims for services furnished to Next Generation Beneficiaries who elect to decline data sharing or for claims for services related to the diagnosis and treatment of substance abuse furnished to Next Generation Beneficiaries. |
| J. | Written Confirmation of Consent |
| 1. | The ACO shall obtain written confirmation that each AIPBP-participating Next Generation Participant and Preferred Provider has consented to receive the AIPBP Fee Reduction. Such written confirmation of consent must be in the form of a completed AIPBP Fee Reduction Agreement signed by an individual legally authorized to act for the entity through whose TIN the Next Generation Participant or Preferred Provider bills Medicare. |
| 2. | As part of the written confirmation of consent, the legally authorized individual must verify the accuracy of the list of Next Generation Participants and Preferred Providers billing under that TIN that have affirmatively consented to AIPBP Fee Reductions. |
| 3. | A Next Generation Participant’s or Preferred Provider’s consent to receive the AIPBP Fee Reduction must apply for the full Performance Year and must be renewed annually in order for the Next Generation Participant or Preferred Provider to continue to participate in AIPBP. |
| 4. | Consent to participate in AIPBP by a Next Generation Participant or Preferred Provider must be voluntary and must not be contingent on or related to receipt of referrals from the ACO, its Next Generation Participants, or Preferred Providers. |
| III. | AIPBP Payment Arrangements |
| A. | The ACO shall have a written payment arrangement with each AIPBP-participating Next Generation Participant or Preferred Provider that establishes how the ACO will make payments for Covered Services that are subject to the AIPBP Fee Reduction (“AIPBP Payment Arrangement”). |
| 3 |
| B. | In establishing the terms of any AIPBP Payment Arrangement, neither party gives or receives remuneration in return for or to induce business other than business covered by the AIPBP Payment Arrangement. |
| C. | The payments made by the ACO under an AIPBP Payment Arrangement may not be made knowingly to induce AIPBP-participating Next Generation Participants and Preferred Providers to reduce or limit Medically Necessary items or services to Beneficiaries. |
| D. | All payments the ACO makes for Covered Services under an AIPBP Payment Arrangement must be monetary payments that have been negotiated in good faith and are consistent with fair market value (which may be more or less than the Medicare Payment amount for a given Medicare-reimbursable service). |
| E. | The ACO shall maintain, in accordance with Section XVIII.B, records of all payments made pursuant to each AIPBP Payment Arrangement. |
| F. | The AIPBP Payment Arrangement must: |
| 1. | Require the ACO to reimburse Next Generation Participants and Preferred Providers for all Covered Services that Medicare would have otherwise paid for, but for the AIPBP Fee Reduction. |
| 2. | Require the ACO to pay for Covered Services furnished by AIPBP-participating Next Generation Participants and Preferred Providers no later than 30 days after receiving notice of the processed claim, as indicated on a weekly report from CMS to the ACO. |
| 3. | Require the Next Generation Participant or Preferred Provider to make Medically Necessary Covered Services available to Next Generation Beneficiaries in accordance with all applicable laws and regulations. |
| 4. | Prohibit the ACO from requiring prior authorization for services furnished to Next Generation Beneficiaries. |
| 5. | Prohibit the ACO and the Next Generation Participant or Preferred Provider from interfering with a Next Generation Beneficiary’s freedom to receive Covered Services from the Medicare-enrolled provider or supplier of his or her choice, regardless of whether the provider or supplier is participating in AIPBP or with the ACO. |
| 6. | Require the Next Generation Participant or Preferred Provider to maintain records regarding the AIPBP Payment Arrangement (including records of any payments made or received under the arrangement) in accordance with Section XVIII.B of the Agreement. |
| 7. | Require the Next Generation Participant or Preferred Provider to provide the Government with access to records regarding the AIPBP Payment Arrangement (including records of any payments made or received under the arrangement) in accordance with Section XVIII.A of the Agreement. |
| G. | The ACO shall ensure that it has and will maintain the capability and funds to reimburse AIPBP-participating Next Generation Participants and Preferred Providers for all Covered Services that they furnish, and that it will promptly make such payments in accordance with Section III.F.2 of this Appendix. |
| 4 |
| IV. | Beneficiary Disputes |
| A. | CMS will process all claims submitted by AIPBP-participating Next Generation Participants and Preferred Providers, and assess coverage for such services and any Beneficiary liability using the same standards that apply under traditional Medicare fee- for-service. |
| B. | All disputes brought by Beneficiaries regarding denied claims will be adjudicated under the claims appeals process at 42 C.F.R. Part 405, subpart I. |
| V. | Provider Payment Dispute Resolution |
The ACO must establish procedures under which AIPBP-participating Next Generation Participants and Preferred Providers may request reconsideration by the ACO of a payment determination. The procedures for requesting reconsideration must be included in the written AIPBP Payment Arrangement between the ACO and the AIPBP-participating Next Generation Participant or Preferred Provider required under Section III.A of this Appendix.
| VI. | Calculation of the All-Inclusive Population-Based Payment |
| A. | Overview |
| 1. | CMS shall calculate the Monthly AIPBP Payment in accordance with Section VI.B of this Appendix. |
| 2. | CMS will make a Monthly AIPBP Payment to the ACO for each month that the ACO participates in AIPBP during the Performance Year. |
| 3. | CMS shall not make any Monthly AIPBP Payments to the ACO after the effective date of the termination of this Agreement. |
| 4. | CMS shall not make any Monthly AIPBP Payments after the effective date of CMS’ termination (in accordance with Section XIX.A of this Agreement) of the ACO’s election to participate in AIPBP. |
| B. | AIPBP Payment Calculation |
| 1. | Calibration Year Used to Estimate the Reduction in FFS Payments |
CMS will use FFS payments from a calibration year to estimate the reduction in FFS payments to AIPBP-participating Next Generation Participants and Preferred Providers for Parts A and B services furnished to Next Generation Beneficiaries during the applicable Performance Year. The calibration year is the calendar year prior to the Performance Year.
| 2. | Population Used to Estimate the Reduction in FFS Payments |
The population used to estimate the reduction in FFS Payments to AIPBP-participating Next Generation Participants and Preferred Providers for a Performance Year consists of those Beneficiaries that would have been aligned with the ACO during the calibration year on the basis of Performance Year Next Generation Participants. This population includes Beneficiaries who were alive on January 1 of the calibration year and not enrolled in a managed care plan in January of that year. This population includes Beneficiaries who would later have been excluded from alignment to the ACO because they did not meet alignment-eligibility requirements during the calibration year or who would have been excluded based on service-area restrictions that are applied retrospectively.
| 5 |
| 3. | Use of Completion Factors to Estimate the Reduction in FFS Payments |
| i. | CMS will use a partial year of claims experience, without run-out, to calculate the estimated reduction in FFS payments to AIPBP-participating Next Generation Participants and Preferred Providers because the AIPBP payment amount is generally calculated prior to or at the start of the Performance Year. |
| ii. | To adjust for run-out and claims not yet incurred, a completion factor is applied based on the experience of the most recent calendar year for which complete experience is available. The most recent calendar year for which complete experience is available is typically the calendar year that is two years prior to the Performance Year. (For example, for PY2017, the completion factor will be based on claims from CY2015 and applied to the CY2016 calibration year). |
| iii. | A completion factor will be calculated and applied for each claim type (e.g., inpatient hospital, skilled nursing facility, home health agency, hospice, physician, outpatient hospital service, etc.). |
| iv. | The completion factor is calculated using the ratio of total expenditures for claims paid for the completion year through December 1 of that year (e.g., December 1, 2015, for PY2017) to expenditures for claims paid for the completion factor year through a three-month run-out period into the following calendar year. (If CY2015 is the completion factor year, this would be March 31, 2016.) |
| 4. | Calculation of Total AIPBP Payment and Monthly AIPBP Payment |
The total amount of AIPBP payments to the ACO for a Performance Year is calculated by determining the total estimated AIPBP Fee Reduction for each AIPBP-participating Next Generation Participant and Preferred Provider, which is equal to:
| i. | The aggregate Parts A and B payments made for services rendered by all AIPBP-participating Next Generation Participants and Preferred Providers in the calibration year; |
| ii. | Multiplied by the completion factor for the relevant claim type; |
| iii. | Multiplied by the ratio of the number of Next Generation Beneficiaries for the Performance Year to the number of aligned Beneficiaries for the calibration year; and |
| iv. | Multiplied by 0.98 (i.e. reduced by 2%) if budget sequestration is in effect for the Performance Year. |
The resulting amount is then divided by 12 to determine the Monthly AIPBP Payment.
| C. | AIPBP Payment Recalculation |
| 6 |
| 1. | CMS will not recalculate the total amount of the AIPBP payment for the Performance Year and the Monthly AIPBP Payment during the Performance Year, except as provided for in this section. |
| 2. | CMS will review actual AIPBP Fee Reductions during the Performance Year. If Performance Year performance data shows, after two quarters, that the Monthly AIPBP Payments for the previous quarter are at least 25% greater or 25% less than total actual AIPBP Fee Reductions taken in the previous quarter, CMS may recalculate and revise the total amount of the AIPBP payment for the Performance Year and the amount of the Monthly AIPBP Payment calculated under Section IV.B.4 based on Performance Year data. The revised Monthly AIPBP Payment shall be payable on a prospective basis only. CMS will provide a report of the recalculated amounts to the ACO. |
| VII. | Reconciliation of the Total Monthly AIPBP Payments |
| A. | CMS will reconcile total Monthly AIPBP payments with total AIPBP Fee Reductions for each Performance Year the ACO participates in AIPBP, by calculating the difference between the total Monthly AIPBP payments CMS paid to the ACO during the Performance Year and the total AIPBP Fee Reductions taken during the Performance Year. Any difference will constitute Other Monies Owed and may be subject to recoupment during annual financial settlement as described in Section XIV.C of this Agreement: |
| 1. | The ACO shall pay CMS the difference in accordance with Section VII.E of this Appendix if the amount CMS paid in Monthly AIPBP payments is greater than the total AIPBP Fee Reductions, and |
| 2. | CMS shall pay the ACO the difference in accordance with Section VII.D of this Appendix if the amount CMS paid in Monthly AIPBP payments is less than the total AIPBP Fee Reductions. |
| B. | CMS will reconcile total Monthly AIPBP Payments separately from the annual financial settlement with the ACO’s benchmark under Appendix B to determine the ACO’s Shared Savings or Shared Losses. The AIPBP Fee Reductions do not affect the calculation of Shared Savings or Shared Losses, which will continue to be based on the amount of the FFS payments that would have been made in the absence of the AIPBP Fee Reduction. The reconciliation of total Monthly AIPBP Payments and the total AIPBP Fee Reductions does not affect and is not affected by the sharing rate or savings/loss cap. |
| C. | During the annual financial settlement, CMS will include any Other Monies Owed due to reconciliation of the total Monthly AIPBP Payments, with the Shared Savings or Shared Losses on the settlement report issued under Section XIV.C.1. of this Agreement, such that the settlement report will show the amount of Shared Savings or Shared Losses, the amount of Other Monies Owed by either CMS or the ACO, as well as the net amount owed by either CMS or the ACO. |
| D. | If the total AIPBP Fee Reductions exceed the total Monthly AIPBP Payments paid to the ACO, CMS will: |
| 7 |
| 1. | Add the difference to the amount paid to the ACO if the ACO has earned Shared Savings; |
| 2. | Subtract the difference from the amount of the Shared Losses owed by the ACO if the ACO owes Shared Losses; or |
| 3. | Pay the amount to the ACO as Other Monies Owed if no Shared Savings are earned and no Shared Losses are owed. |
| E. | If the total Monthly AIPBP Payments paid to the ACO exceed the total AIPBP Fee Reductions, CMS will: |
| 1. | Subtract the difference from the amount paid to the ACO if the ACO has earned Shared Savings; |
| 2. | Add the difference to the amount owed to CMS by the ACO if the ACO owes Shared Losses; or |
| 3. | Recover the difference from the ACO as Other Monies Owed if no Shared Savings are earned and no Shared Losses are owed. |
| F. | In the event that an AIPBP-participating ACO elects to withdraw and terminate without financial reconciliation in accordance with XIX.C.1 and XIX.D.3 of the Agreement, CMS will reconcile total Monthly AIPBP Payments within three (3) months after the ACO’s effective termination date, and the ACO must pay any Other Monies Owed to CMS in accordance with XIV.C.5. |
| G. | CMS will include in the reconciliation of total Monthly AIPBP Payments any AIPBP Fee Reductions for services provided to Beneficiaries who were Next Generation Beneficiaries at the time the services were furnished but were later excluded from the aligned population during the Performance Year because they did not meet alignment- eligibility requirements. |
| H. | Adjusted Settlement |
| 1. | For each Performance Year in which the ACO participates in AIPBP, CMS shall conduct a second AIPBP Reconciliation one year after the original AIPBP Reconciliation at the same time that CMS issues the settlement report for the subsequent Performance Year. |
| 2. | If, as a result of the second AIPBP Reconciliation, CMS determines that: |
| a. | The total AIPBP Fee Reductions exceeds the total amount of AIPBP Payments made to the ACO as Monthly AIPBP Payments during the Performance Year, as reconciled during the initial AIPBP Reconciliation for the applicable Performance Year under Section VII.A of this Appendix, the difference will be deemed Other Monies Owed and CMS will pay the amount to the ACO pursuant to section XIV.C.5 of the Agreement; |
| b. | The total amount of AIPBP payments made to the ACO as Monthly AIPBP Payments during the Performance Year, as reconciled during the initial AIPBP Reconciliation for the applicable Performance Year under Section VII.A of this Appendix, exceeds the total AIPBP Fee Reductions during the Performance Year, the difference will be deemed Other Monies Owed and the ACO will pay the amount to CMS pursuant to section XIV.C.5 of the Agreement; |
| 8 |
| 3. | In the case of the final year of the Agreement Term or termination of the Agreement by the ACO before the date determined under Section XIX.D.3: |
| a. | CMS will make reasonable efforts to conduct the second AIPBP Reconciliation within 12 months after the issuance of the original settlement report for the applicable Performance Year; |
| b. | CMS will issue an adjusted settlement report to the ACO setting forth the results of the second AIPBP Reconciliation and identifying any Other Monies Owed by the ACO to CMS, or by CMS to the ACO, as a result of this second AIPBP Reconciliation. |
| c. | Any amounts owed by the ACO to CMS, or by CMS to the ACO, as a result of this second AIPBP Reconciliation will be payable in accordance with XIV.C.5 of the Agreement. |
| 9 |