EX-99.1
Published on November 8, 2022

Apollo Medical Holdings November 2022 Powered by Technology. Built by Doctors. For Patients.
This presentation contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995, Section 27A of the Securities Act and Section 21E of the Exchange Act. Forward-looking statements include any statements about the Company's business, financial condition, operating results, plans, objectives, expectations and intentions, expansion plans, integration of acquired companies and any projections of earnings, revenue, EBITDA, Adjusted EBITDA or other financial items, such as the Company's projected capitation and future liquidity, and may be identified by the use of forward-looking terms such as “anticipate,” “could,” “can,” “may,” “might,” “potential,” “predict,” “should,” “estimate,” “expect,” “project,” “believe,” “plan,” “envision,” “intend,” “continue,” “target,” “seek,” “will,” “would,” and the negative of such terms, other variations on such terms or other similar or comparable words, phrases or terminology. Forward-looking statements reflect current views with respect to future events and financial performance and therefore cannot be guaranteed. Such statements are based on the current expectations and certain assumptions of the Company's management, and some or all of such expectations and assumptions may not materialize or may vary significantly from actual results. Actual results may also vary materially from forward-looking statements due to risks, uncertainties and other factors, known and unknown, including the risk factors described from time to time in the Company’s reports to the U.S. Securities and Exchange Commission (the “SEC”), including without limitation the risk factors discussed in the Company's Annual Report on Form 10-K for the year ended December 31, 2021, and subsequent Quarterly Reports on Form 10-Q. Because the factors referred to above could cause actual results or outcomes to differ materially from those expressed or implied in any forward-looking statements, you should not place undue reliance on any such forward-looking statements. Any forward-looking statements speak only as of the date of this presentation and, unless legally required, the Company does not undertake any obligation to update any forward-looking statement, as a result of new information, future events or otherwise. Forward-looking statements 2
ApolloMed investment highlights 3 1. 2. 3. 5. 6. 4. Proven model for 25+ years with demonstrable clinical outcomes across all populations (Medicare Advantage, Managed Medicaid, Commercial, ACA Exchange, and Medicare FFS) Industry-leading unit economics support strong growth, with 3-year revenue CAGR1 of 25- 26% and 3-year adj. EBITDA CAGR1 of 36-45% Creating a differentiated independent provider market by enabling entrepreneurial providers to achieve the same scale and outcomes as an integrated delivery system Proprietary technology platform custom-built for providers, with a data moat Multiple drivers for growth with a scalable and repeatable playbook led by differentiated leadership team Large and growing TAM with significant whitespace ahead across market segments (1) ApolloMed 2019 to mid-point of 2022E revenue growth; ApolloMed 2019 to mid-point of 2022E adj. EBITDA growth. Please refer to the “2022 Guidance Reconciliation of Net Income to EBITDA and Adjusted EBITDA” and “Use of Non-GAAP Financial Measures” slides for more information.

10,600+ Contracted Physicians ApolloMed Overview 4 $132M TTM Adj. EBITDA2 $1.05B TTM Revenue2 ApolloMed is a tech- powered, value-based healthcare network for all Americans We enable best in class clinical outcomes within our value-based care provider organizations We provide quality care to traditionally underserved communities and ethnic minorities Our value-based enablement (VBE) suite positions us to scale rapidly nationwide 1.2M Patients Managed in VBC Contracts1 (1) This figure excludes fee-for-service patients (2) Please refer to the “Reconciliation of TTM and 12 Months Net Income to EBITDA and Adjusted EBITDA” and “Use of Non-GAAP Financial Measures” slides for more information.

Industry Overview & ApolloMed Value Proposition
The U.S. healthcare landscape is rapidly moving towards value-based care… 6 Fee-for-service Value-based care Lack of incentives to improve chronic health conditions Driving a trend of rapidly increasing medical costs Rising patient dissatisfaction with provider relationship and quality of care Providers incentivized to improve general health of patients Compensation models in place to lower the overall cost of care Patients with better access and better care experience CMS, COVID-19, payer contracting, and focus on quality while lowering total cost are driving shifts in healthcare Value-based careFee-for-service
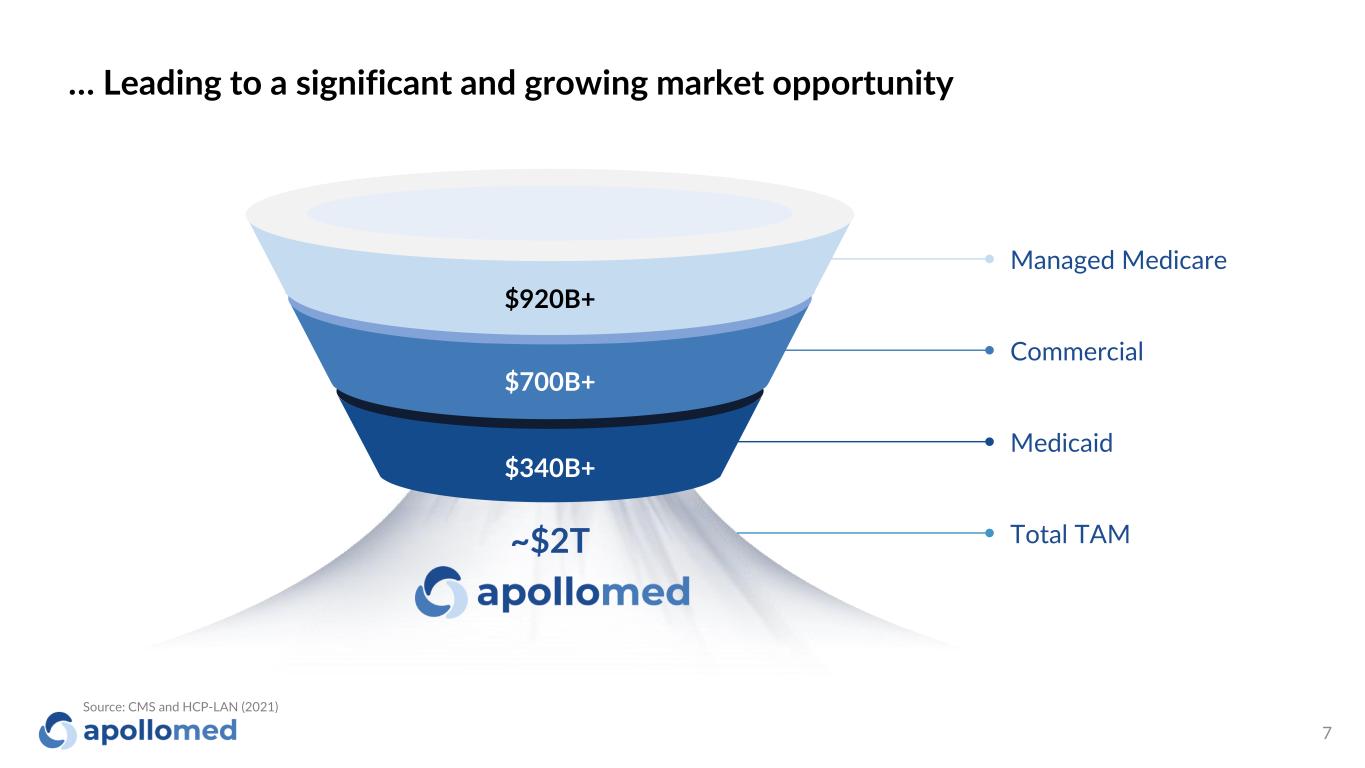
… Leading to a significant and growing market opportunity 7 $920B+ $700B+ $340B+ Managed Medicare Commercial Medicaid Total TAM~$2T Source: CMS and HCP-LAN (2021)
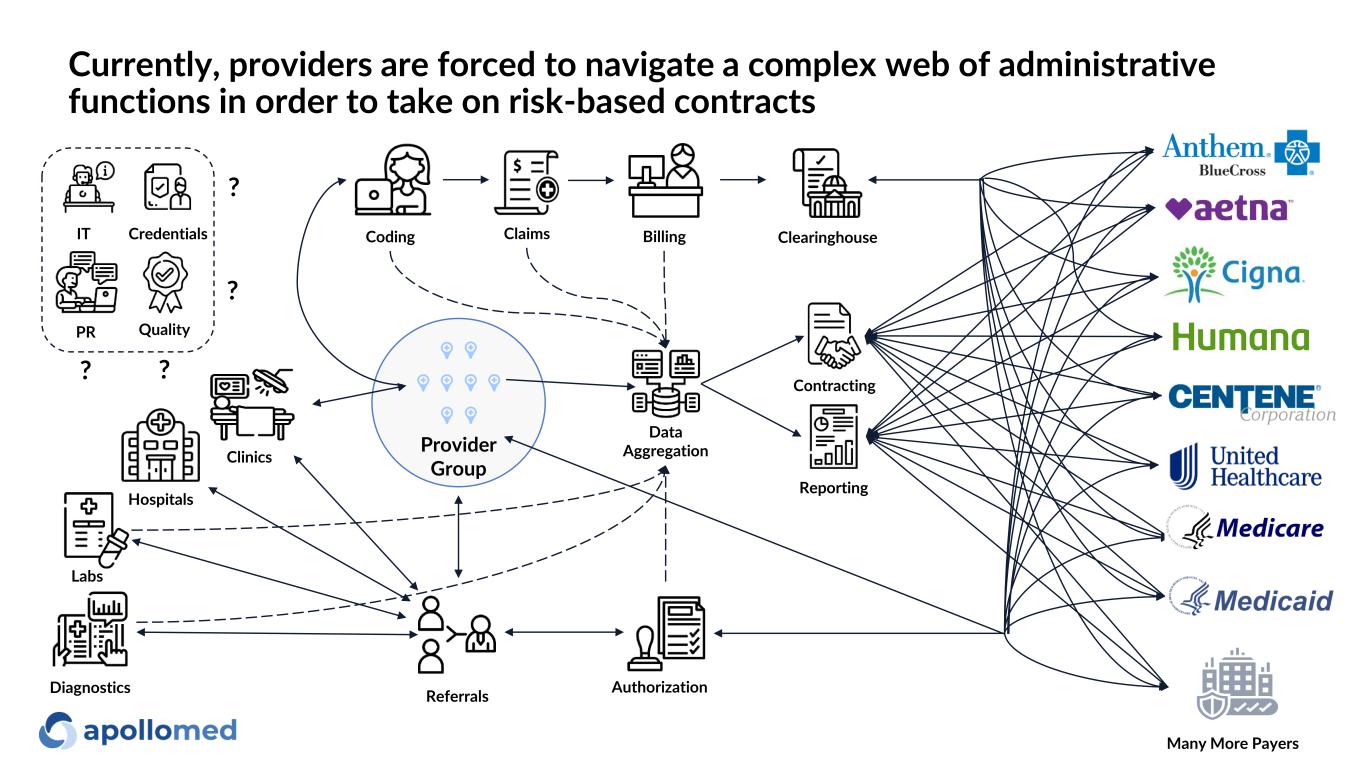
Reporting Contracting Claims Data Aggregation BillingCoding Hospitals Clinics Referrals Provider Group Authorization ClearinghouseIT Credentials PR Quality ? ? ? ? Labs Many More Payers Diagnostics Currently, providers are forced to navigate a complex web of administrative functions in order to take on risk-based contracts
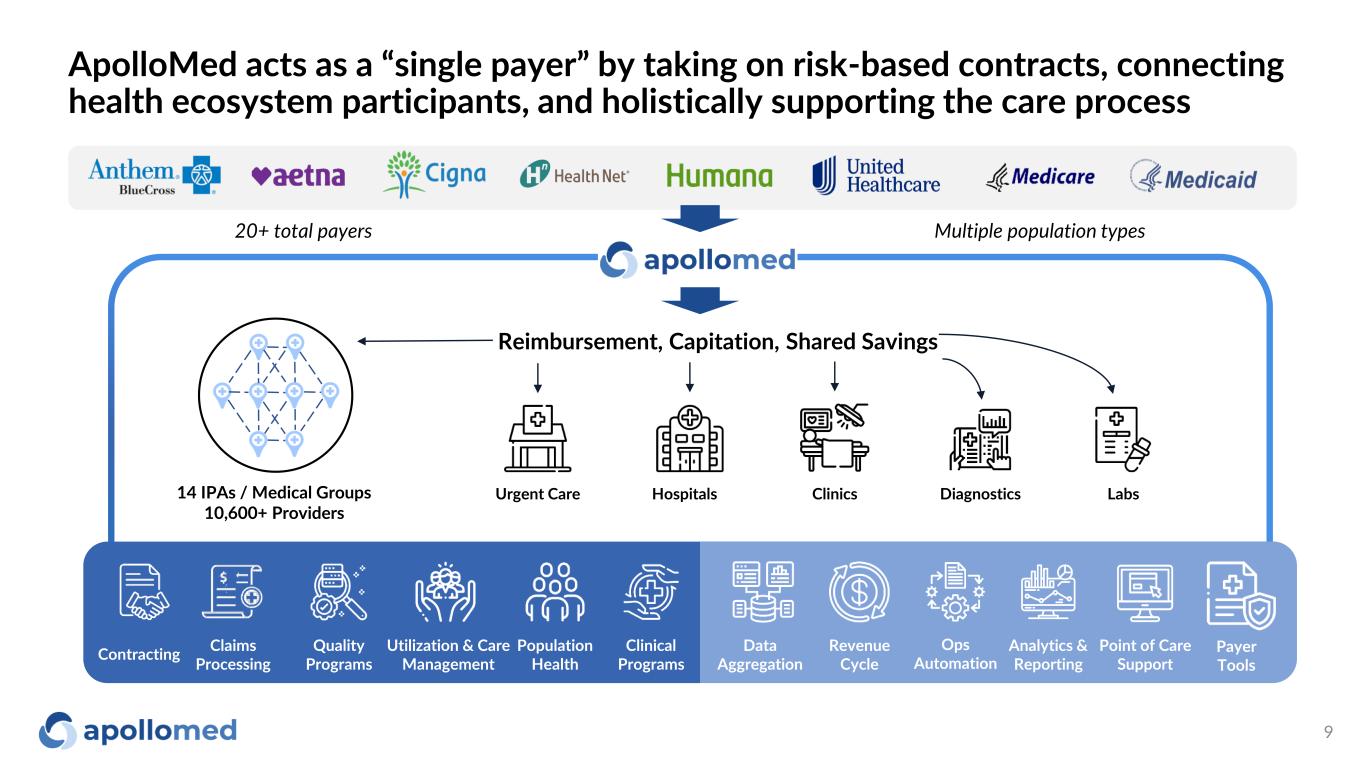
ApolloMed acts as a “single payer” by taking on risk-based contracts, connecting health ecosystem participants, and holistically supporting the care process 9 Reimbursement, Capitation, Shared Savings Hospitals LabsUrgent Care Clinics Diagnostics 20+ total payers Multiple population types 14 IPAs / Medical Groups 10,600+ Providers Utilization & Care Management Claims Processing Ops Automation Point of Care Support Analytics & Reporting Contracting Clinical Programs Quality Programs Population Health Data Aggregation Revenue Cycle Payer Tools
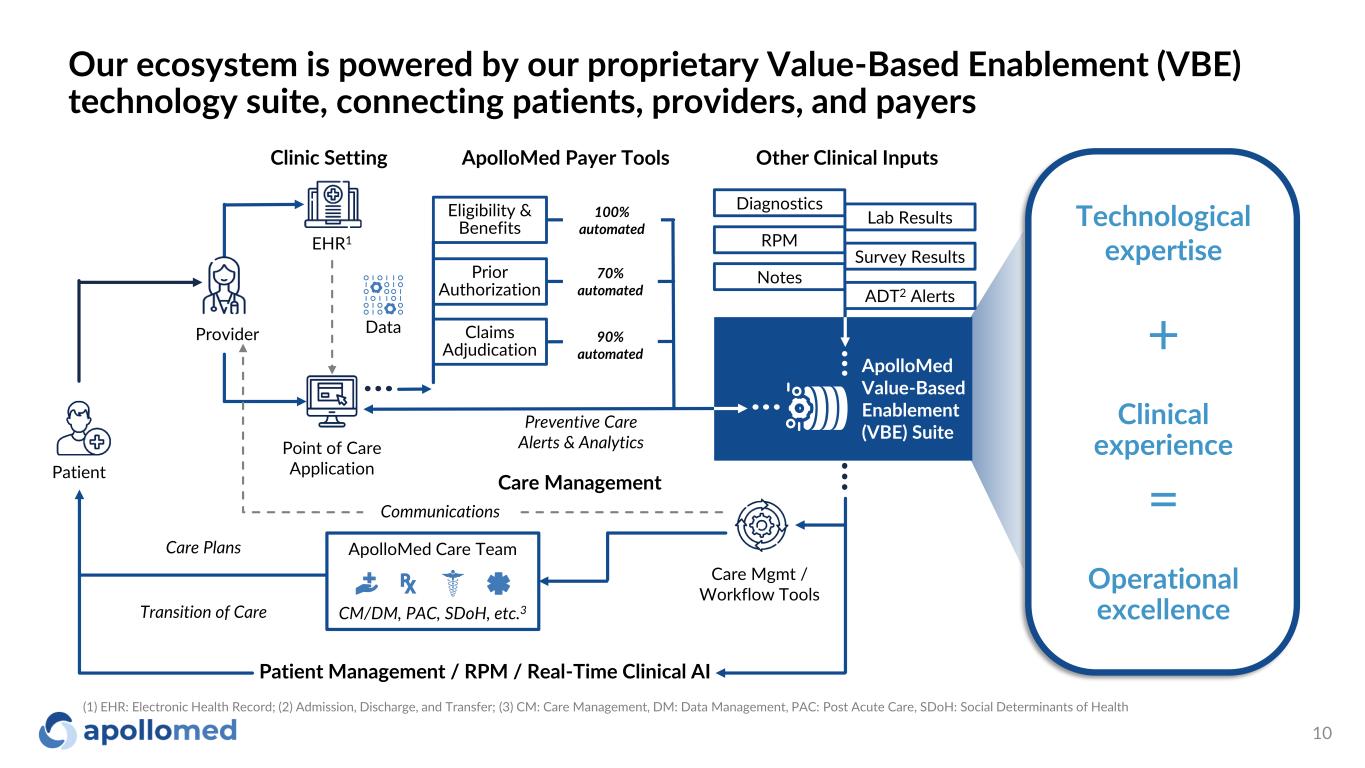
Our ecosystem is powered by our proprietary Value-Based Enablement (VBE) technology suite, connecting patients, providers, and payers 10 Provider Point of Care Application EHR1 Data Patient Care Management ApolloMed Care Team CM/DM, PAC, SDoH, etc.3 Communications Patient Management / RPM / Real-Time Clinical AI Care Mgmt / Workflow Tools Eligibility & Benefits Claims Adjudication Prior Authorization ApolloMed Payer Tools Other Clinical InputsClinic Setting 100% automated 70% automated 90% automated Technological expertise Operational excellence Clinical experience + = ApolloMed Value-Based Enablement (VBE) Suite Care Plans Transition of Care Preventive Care Alerts & Analytics RPM Notes ADT2 Alerts Diagnostics Lab Results Survey Results (1) EHR: Electronic Health Record; (2) Admission, Discharge, and Transfer; (3) CM: Care Management, DM: Data Management, PAC: Post Acute Care, SDoH: Social Determinants of Health
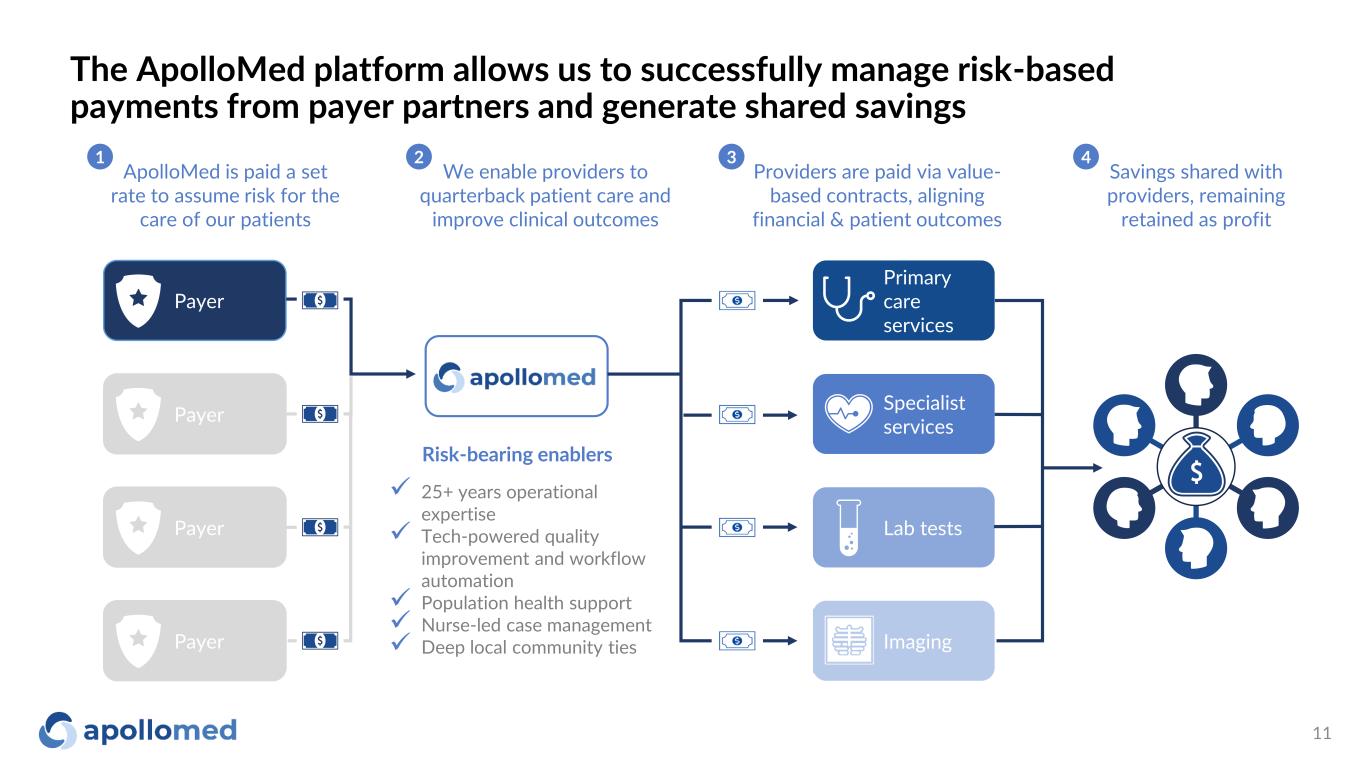
✓ 25+ years operational expertise ✓ Tech-powered quality improvement and workflow automation ✓ Population health support ✓ Nurse-led case management ✓ Deep local community ties The ApolloMed platform allows us to successfully manage risk-based payments from payer partners and generate shared savings 11 Payer Payer Payer Payer Primary care services Specialist services Lab tests Imaging Savings shared with providers, remaining retained as profit Risk-bearing enablers ApolloMed is paid a set rate to assume risk for the care of our patients Providers are paid via value- based contracts, aligning financial & patient outcomes 1 3 4 We enable providers to quarterback patient care and improve clinical outcomes 2
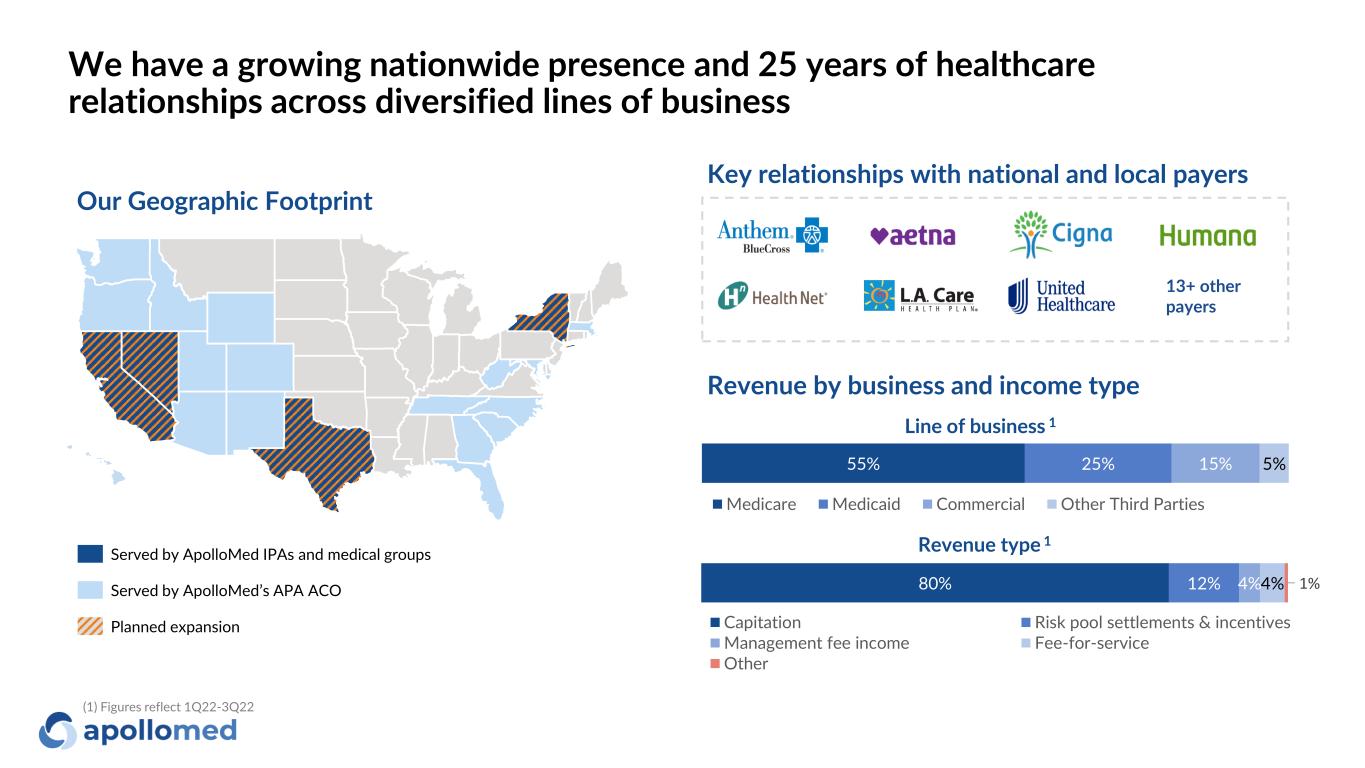
We have a growing nationwide presence and 25 years of healthcare relationships across diversified lines of business Served by ApolloMed IPAs and medical groups Served by ApolloMed’s APA ACO Planned expansion Our Geographic Footprint Key relationships with national and local payers 55% 25% 15% 5% Medicare Medicaid Commercial Other Third Parties 80% 12% 4%4% 1% Capitation Risk pool settlements & incentives Management fee income Fee-for-service Other Revenue by business and income type Line of business 1 Revenue type 1 13+ other payers (1) Figures reflect 1Q22-3Q22
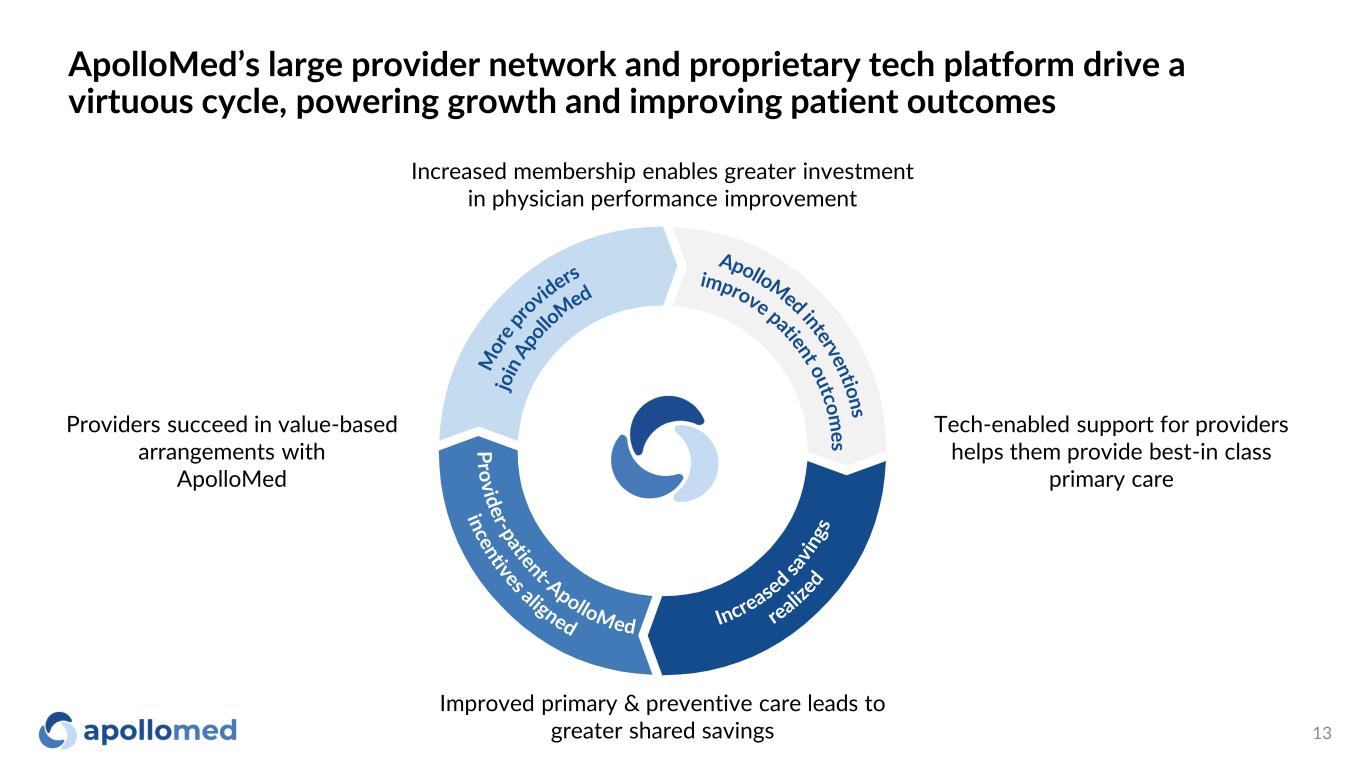
ApolloMed’s large provider network and proprietary tech platform drive a virtuous cycle, powering growth and improving patient outcomes 13 Improved primary & preventive care leads to greater shared savings Tech-enabled support for providers helps them provide best-in class primary care Providers succeed in value-based arrangements with ApolloMed Increased membership enables greater investment in physician performance improvement
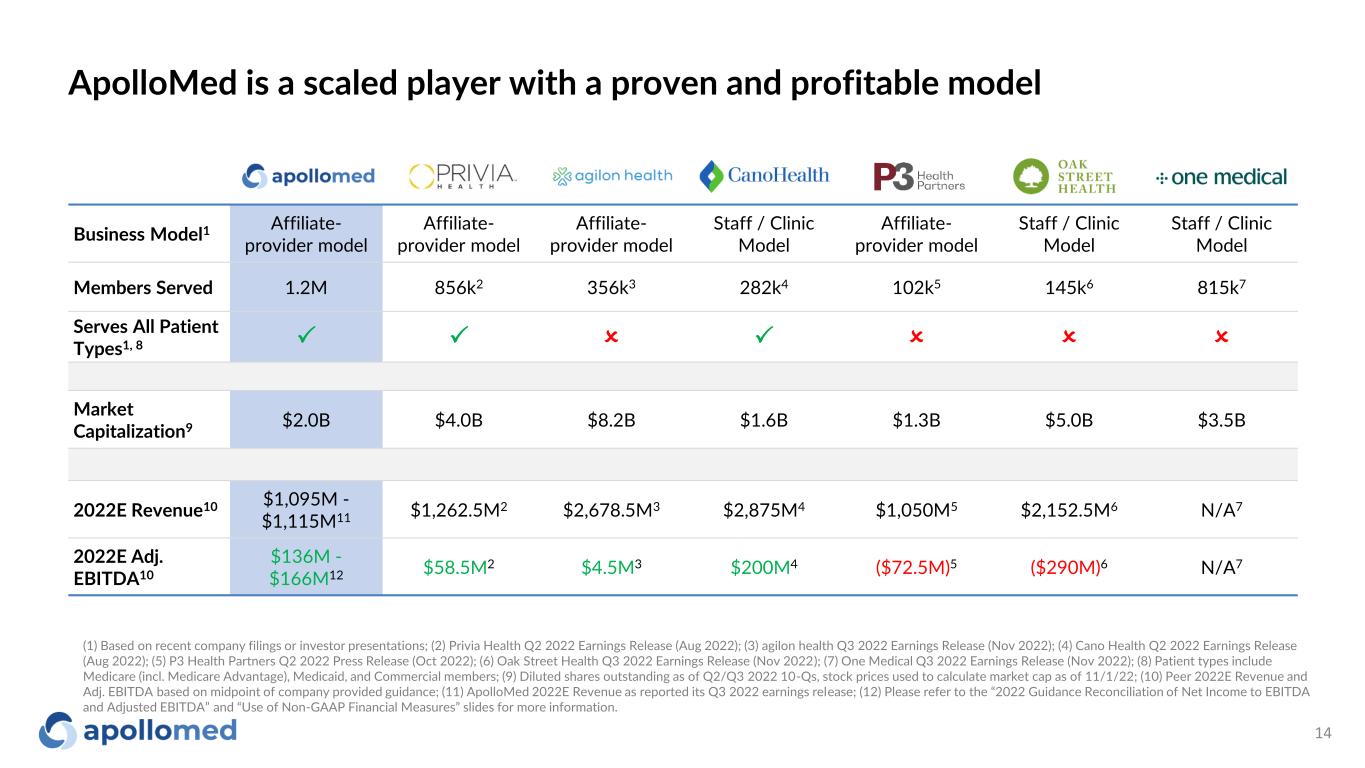
ApolloMed is a scaled player with a proven and profitable model 14 Business Model1 Affiliate- provider model Affiliate- provider model Affiliate- provider model Staff / Clinic Model Affiliate- provider model Staff / Clinic Model Staff / Clinic Model Members Served 1.2M 856k2 356k3 282k4 102k5 145k6 815k7 Serves All Patient Types1, 8 P P O P O O O Market Capitalization9 $2.0B $4.0B $8.2B $1.6B $1.3B $5.0B $3.5B 2022E Revenue10 $1,095M - $1,115M11 $1,262.5M2 $2,678.5M3 $2,875M4 $1,050M5 $2,152.5M6 N/A7 2022E Adj. EBITDA10 $136M - $166M12 $58.5M2 $4.5M3 $200M4 ($72.5M)5 ($290M)6 N/A7 (1) Based on recent company filings or investor presentations; (2) Privia Health Q2 2022 Earnings Release (Aug 2022); (3) agilon health Q3 2022 Earnings Release (Nov 2022); (4) Cano Health Q2 2022 Earnings Release (Aug 2022); (5) P3 Health Partners Q2 2022 Press Release (Oct 2022); (6) Oak Street Health Q3 2022 Earnings Release (Nov 2022); (7) One Medical Q3 2022 Earnings Release (Nov 2022); (8) Patient types include Medicare (incl. Medicare Advantage), Medicaid, and Commercial members; (9) Diluted shares outstanding as of Q2/Q3 2022 10-Qs, stock prices used to calculate market cap as of 11/1/22; (10) Peer 2022E Revenue and Adj. EBITDA based on midpoint of company provided guidance; (11) ApolloMed 2022E Revenue as reported its Q3 2022 earnings release; (12) Please refer to the “2022 Guidance Reconciliation of Net Income to EBITDA and Adjusted EBITDA” and “Use of Non-GAAP Financial Measures” slides for more information.

Clinical Outcomes
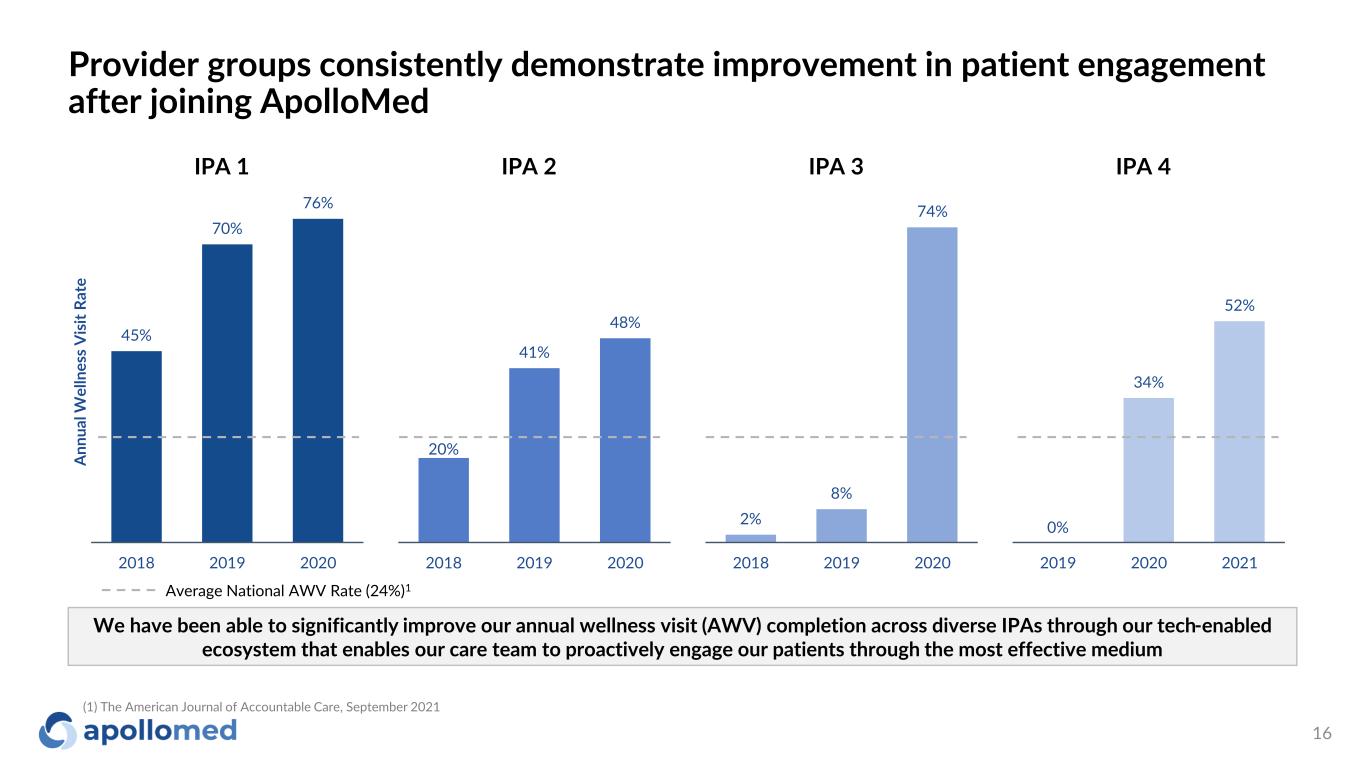
Provider groups consistently demonstrate improvement in patient engagement after joining ApolloMed 16 45% 70% 76% 2018 2019 2020 A nn ua l W el ln es s V is it R at e IPA 1 IPA 2 IPA 3 IPA 4 20% 41% 48% 2018 2019 2020 2% 8% 74% 2018 2019 2020 0% 34% 52% 2019 2020 2021 We have been able to significantly improve our annual wellness visit (AWV) completion across diverse IPAs through our tech-enabled ecosystem that enables our care team to proactively engage our patients through the most effective medium Average National AWV Rate (24%)1 (1) The American Journal of Accountable Care, September 2021
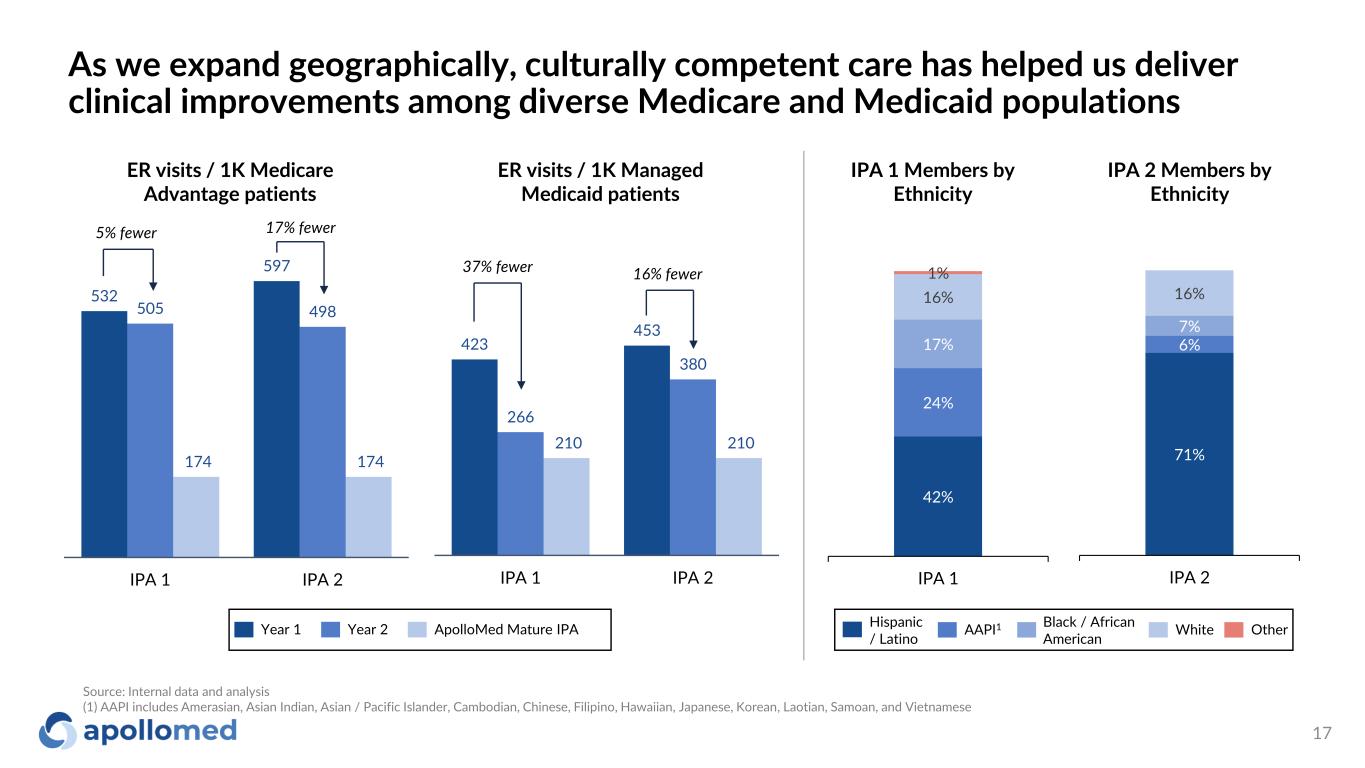
532 597 505 498 174 174 IPA 1 IPA 2 As we expand geographically, culturally competent care has helped us deliver clinical improvements among diverse Medicare and Medicaid populations 17 ER visits / 1K Medicare Advantage patients ER visits / 1K Managed Medicaid patients 423 453 266 380 210 210 IPA 1 IPA 2 42% 24% 17% 16% 1% IPA 1 71% 6% 7% 16% IPA 2 IPA 1 Members by Ethnicity IPA 2 Members by Ethnicity Year 1 Year 2 ApolloMed Mature IPA Hispanic / Latino AAPI1 Black / African American White Other 5% fewer 17% fewer 37% fewer 16% fewer Source: Internal data and analysis (1) AAPI includes Amerasian, Asian Indian, Asian / Pacific Islander, Cambodian, Chinese, Filipino, Hawaiian, Japanese, Korean, Laotian, Samoan, and Vietnamese
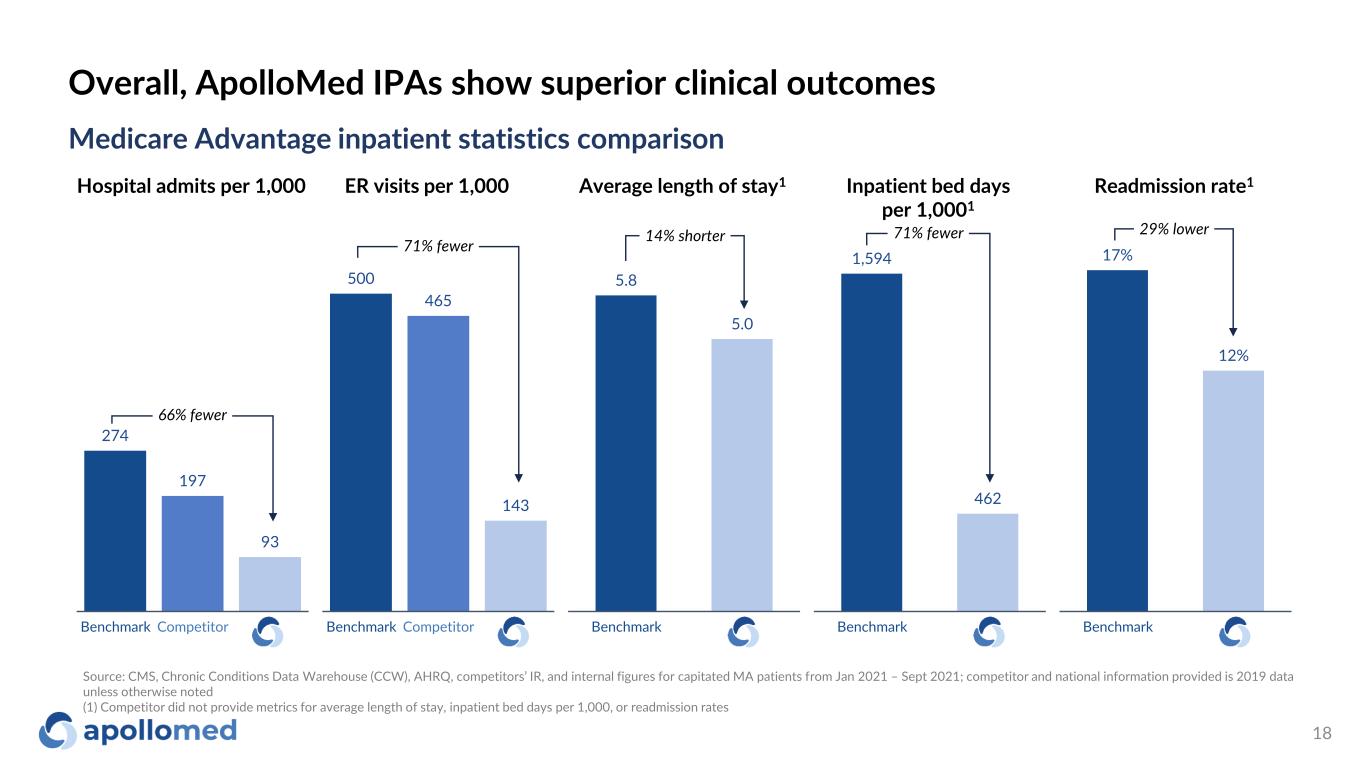
Overall, ApolloMed IPAs show superior clinical outcomes 18 Medicare Advantage inpatient statistics comparison Hospital admits per 1,000 ER visits per 1,000 Average length of stay1 Inpatient bed days per 1,0001 Readmission rate1 274 197 93 Benchmark Competitor 66% fewer 500 465 143 Benchmark Competitor 71% fewer 5.8 5.0 Benchmark 14% shorter 1,594 462 Benchmark 71% fewer 17% 12% Benchmark 29% lower Source: CMS, Chronic Conditions Data Warehouse (CCW), AHRQ, competitors’ IR, and internal figures for capitated MA patients from Jan 2021 – Sept 2021; competitor and national information provided is 2019 data unless otherwise noted (1) Competitor did not provide metrics for average length of stay, inpatient bed days per 1,000, or readmission rates
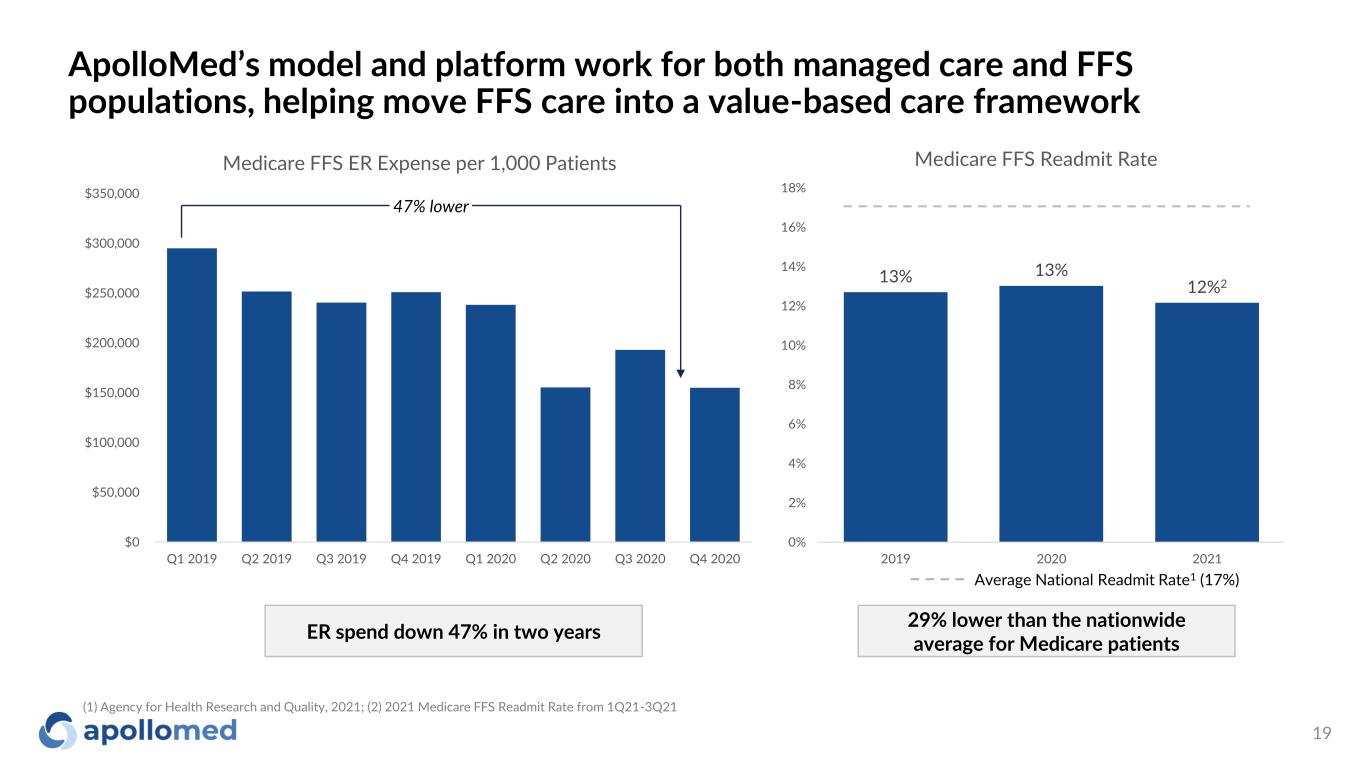
ApolloMed’s model and platform work for both managed care and FFS populations, helping move FFS care into a value-based care framework 19 $0 $50,000 $100,000 $150,000 $200,000 $250,000 $300,000 $350,000 Q1 2019 Q2 2019 Q3 2019 Q4 2019 Q1 2020 Q2 2020 Q3 2020 Q4 2020 Medicare FFS ER Expense per 1,000 Patients 47% lower 13% 13% 12%2 0% 2% 4% 6% 8% 10% 12% 14% 16% 18% 2019 2020 2021 Medicare FFS Readmit Rate Average National Readmit Rate1 (17%) ER spend down 47% in two years 29% lower than the nationwide average for Medicare patients (1) Agency for Health Research and Quality, 2021; (2) 2021 Medicare FFS Readmit Rate from 1Q21-3Q21
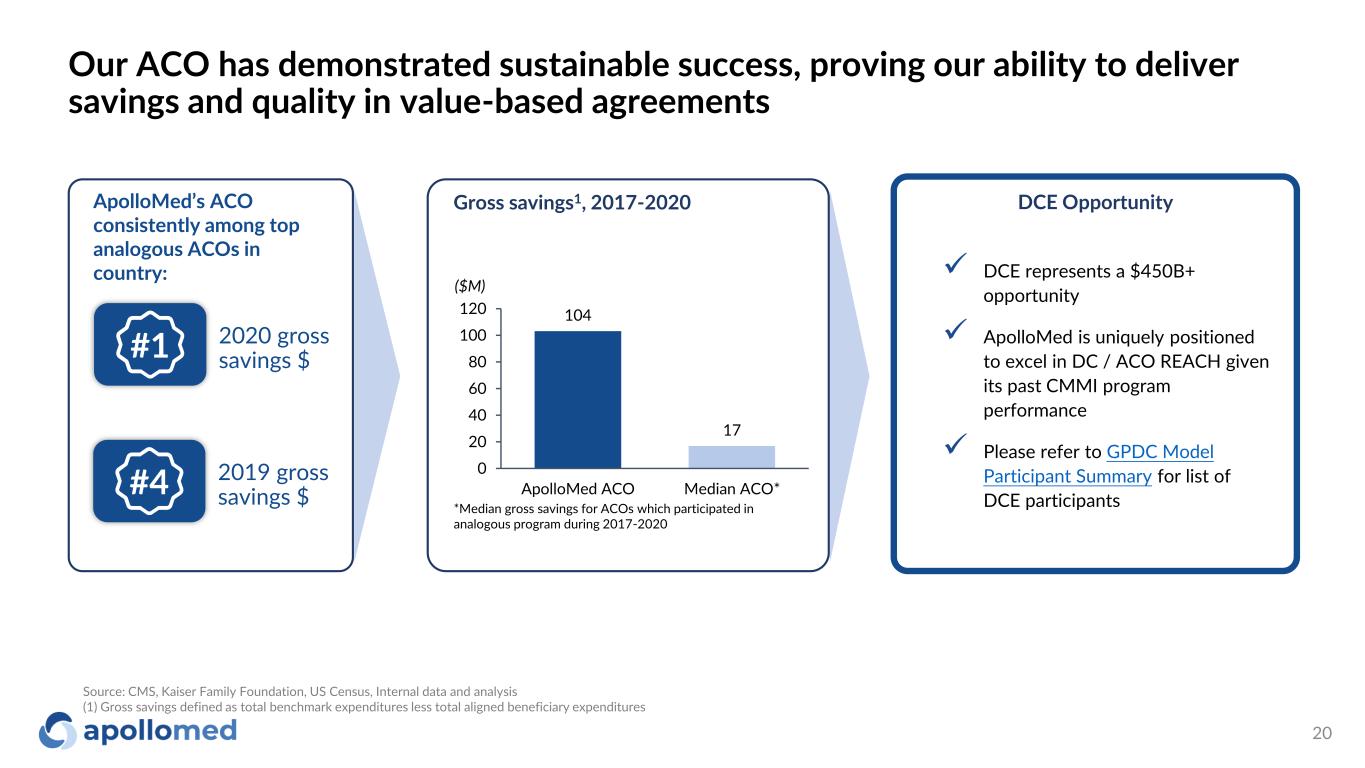
Our ACO has demonstrated sustainable success, proving our ability to deliver savings and quality in value-based agreements 20 ApolloMed’s ACO consistently among top analogous ACOs in country: 2020 gross savings $ 2019 gross savings $ Gross savings1, 2017-2020 *Median gross savings for ACOs which participated in analogous program during 2017-2020 104 17 0 20 40 60 80 100 120 ApolloMed ACO Median ACO* ($M) #1 #4 ✓ DCE represents a $450B+ opportunity ✓ ApolloMed is uniquely positioned to excel in DC / ACO REACH given its past CMMI program performance ✓ Please refer to GPDC Model Participant Summary for list of DCE participants DCE Opportunity Source: CMS, Kaiser Family Foundation, US Census, Internal data and analysis (1) Gross savings defined as total benchmark expenditures less total aligned beneficiary expenditures

Growth Strategy
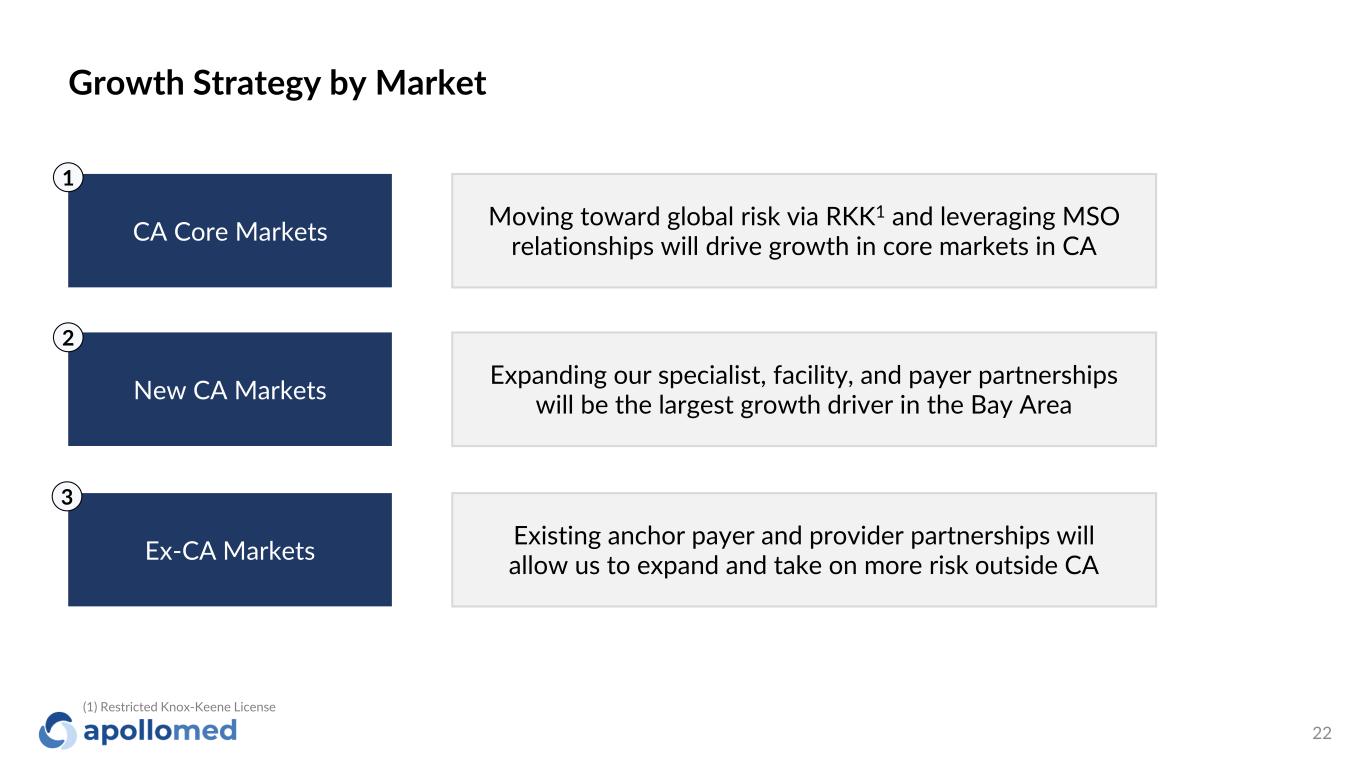
Growth Strategy by Market 22 CA Core Markets New CA Markets Ex-CA Markets Moving toward global risk via RKK1 and leveraging MSO relationships will drive growth in core markets in CA Expanding our specialist, facility, and payer partnerships will be the largest growth driver in the Bay Area Existing anchor payer and provider partnerships will allow us to expand and take on more risk outside CA 1 2 3 (1) Restricted Knox-Keene License
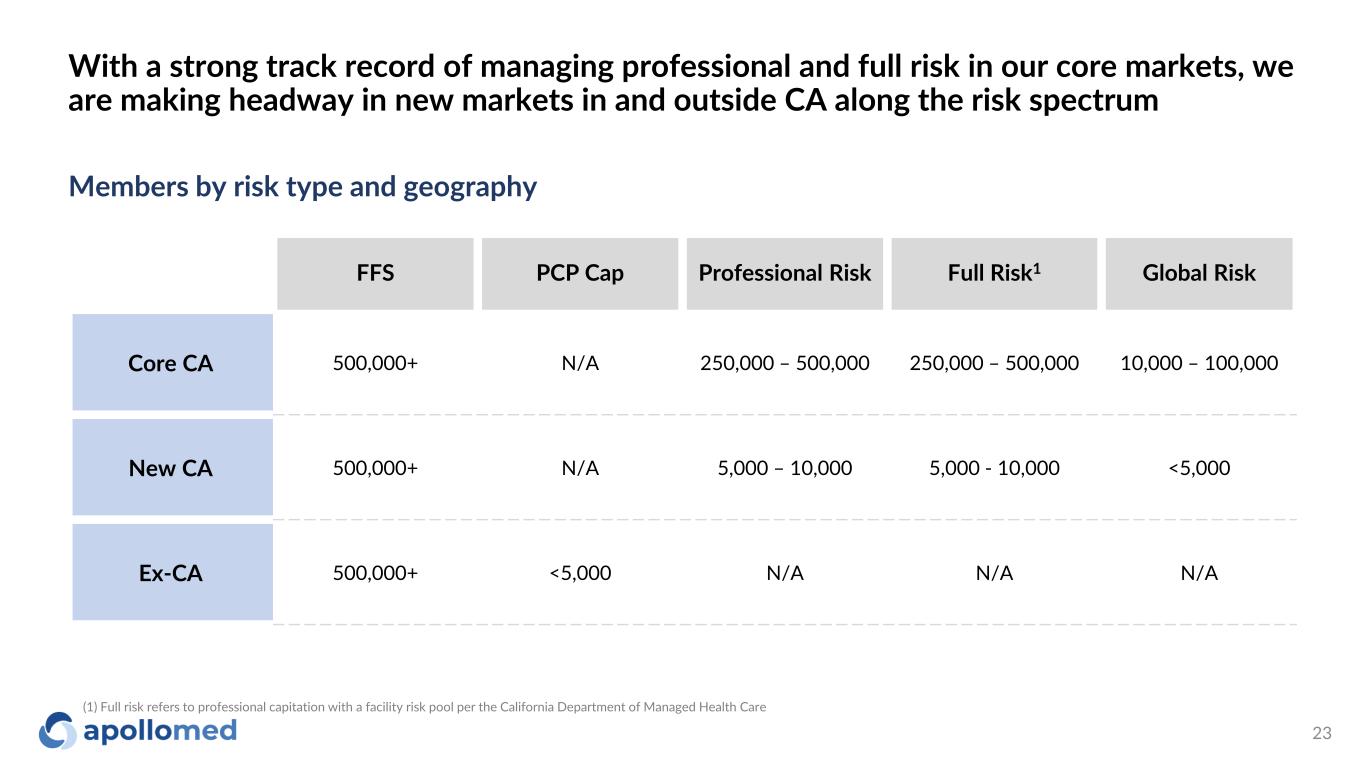
With a strong track record of managing professional and full risk in our core markets, we are making headway in new markets in and outside CA along the risk spectrum 23 FFS PCP Cap Professional Risk Full Risk1 Global Risk Core CA 500,000+ N/A 250,000 – 500,000 250,000 – 500,000 10,000 – 100,000 New CA 500,000+ N/A 5,000 – 10,000 5,000 - 10,000 <5,000 Ex-CA 500,000+ <5,000 N/A N/A N/A Members by risk type and geography (1) Full risk refers to professional capitation with a facility risk pool per the California Department of Managed Health Care
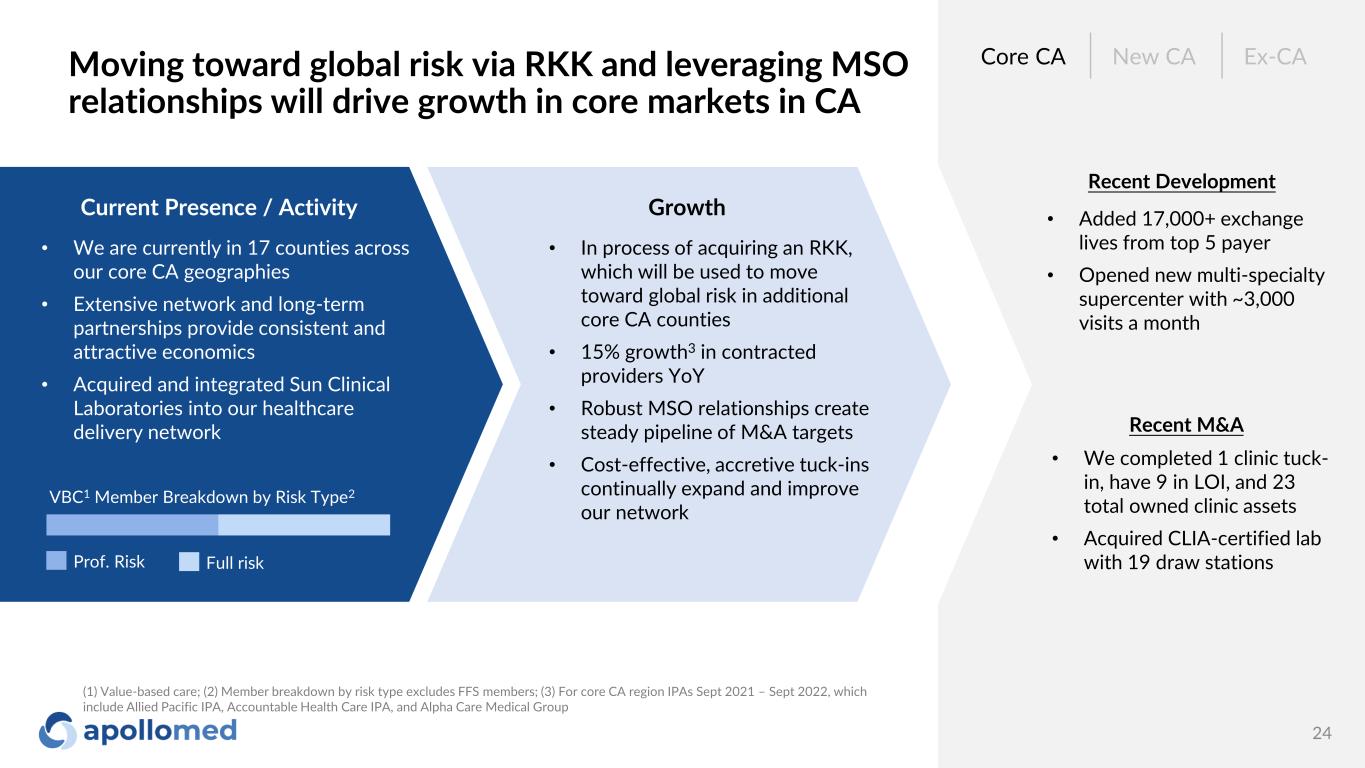
Moving toward global risk via RKK and leveraging MSO relationships will drive growth in core markets in CA 24 Current Presence / Activity • We are currently in 17 counties across our core CA geographies • Extensive network and long-term partnerships provide consistent and attractive economics • Acquired and integrated Sun Clinical Laboratories into our healthcare delivery network Growth • In process of acquiring an RKK, which will be used to move toward global risk in additional core CA counties • 15% growth3 in contracted providers YoY • Robust MSO relationships create steady pipeline of M&A targets • Cost-effective, accretive tuck-ins continually expand and improve our network • Added 17,000+ exchange lives from top 5 payer • Opened new multi-specialty supercenter with ~3,000 visits a month Core CA New CA Ex-CA Prof. Risk Full risk VBC1 Member Breakdown by Risk Type2 Recent Development Recent M&A • We completed 1 clinic tuck- in, have 9 in LOI, and 23 total owned clinic assets • Acquired CLIA-certified lab with 19 draw stations (1) Value-based care; (2) Member breakdown by risk type excludes FFS members; (3) For core CA region IPAs Sept 2021 – Sept 2022, which include Allied Pacific IPA, Accountable Health Care IPA, and Alpha Care Medical Group
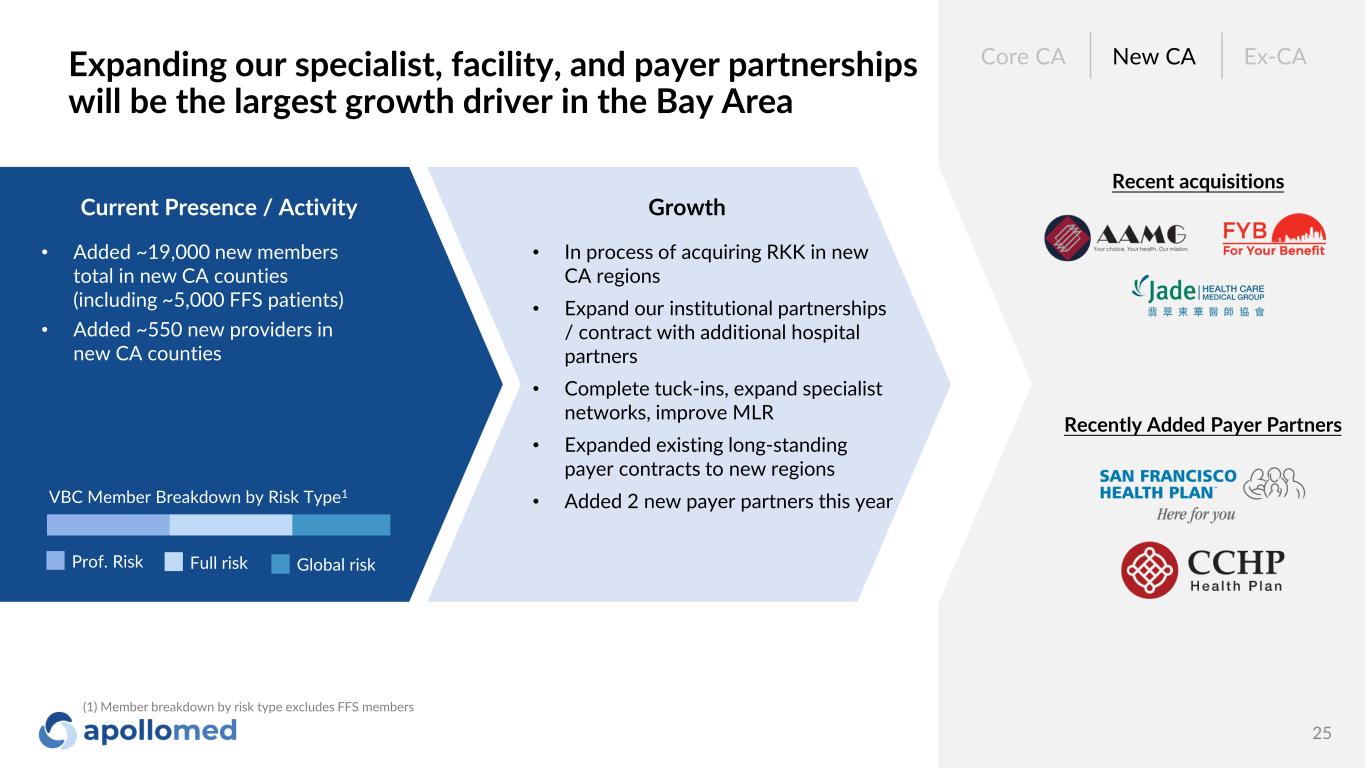
Expanding our specialist, facility, and payer partnerships will be the largest growth driver in the Bay Area 25 Current Presence / Activity • Added ~19,000 new members total in new CA counties (including ~5,000 FFS patients) • Added ~550 new providers in new CA counties Growth • In process of acquiring RKK in new CA regions • Expand our institutional partnerships / contract with additional hospital partners • Complete tuck-ins, expand specialist networks, improve MLR • Expanded existing long-standing payer contracts to new regions • Added 2 new payer partners this year Recent acquisitions Core CA New CA Ex-CA Prof. Risk Full risk VBC Member Breakdown by Risk Type1 Recently Added Payer Partners Global risk (1) Member breakdown by risk type excludes FFS members
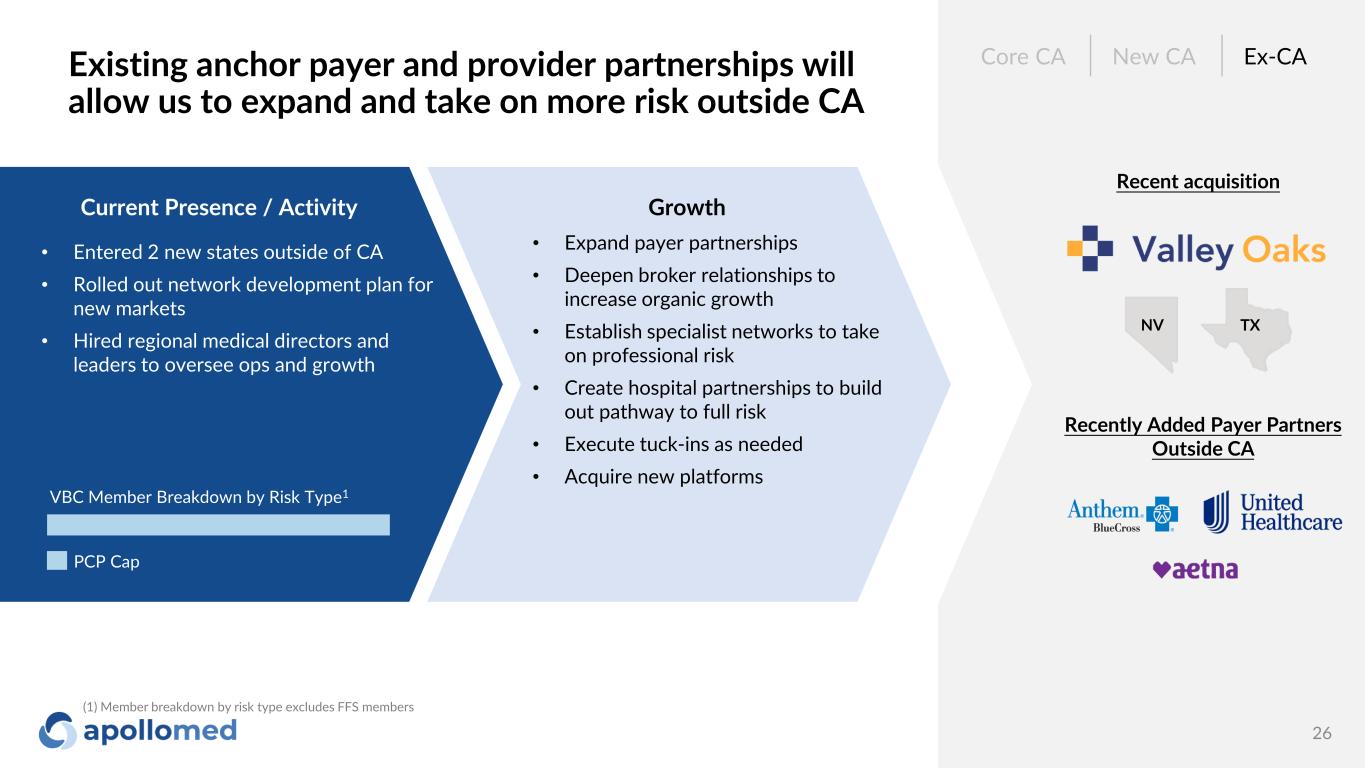
Existing anchor payer and provider partnerships will allow us to expand and take on more risk outside CA 26 Current Presence / Activity • Entered 2 new states outside of CA • Rolled out network development plan for new markets • Hired regional medical directors and leaders to oversee ops and growth Core CA New CA Ex-CA PCP Cap VBC Member Breakdown by Risk Type1 Recent acquisition Recently Added Payer Partners Outside CA NV TX Growth • Expand payer partnerships • Deepen broker relationships to increase organic growth • Establish specialist networks to take on professional risk • Create hospital partnerships to build out pathway to full risk • Execute tuck-ins as needed • Acquire new platforms (1) Member breakdown by risk type excludes FFS members
Financial Overview
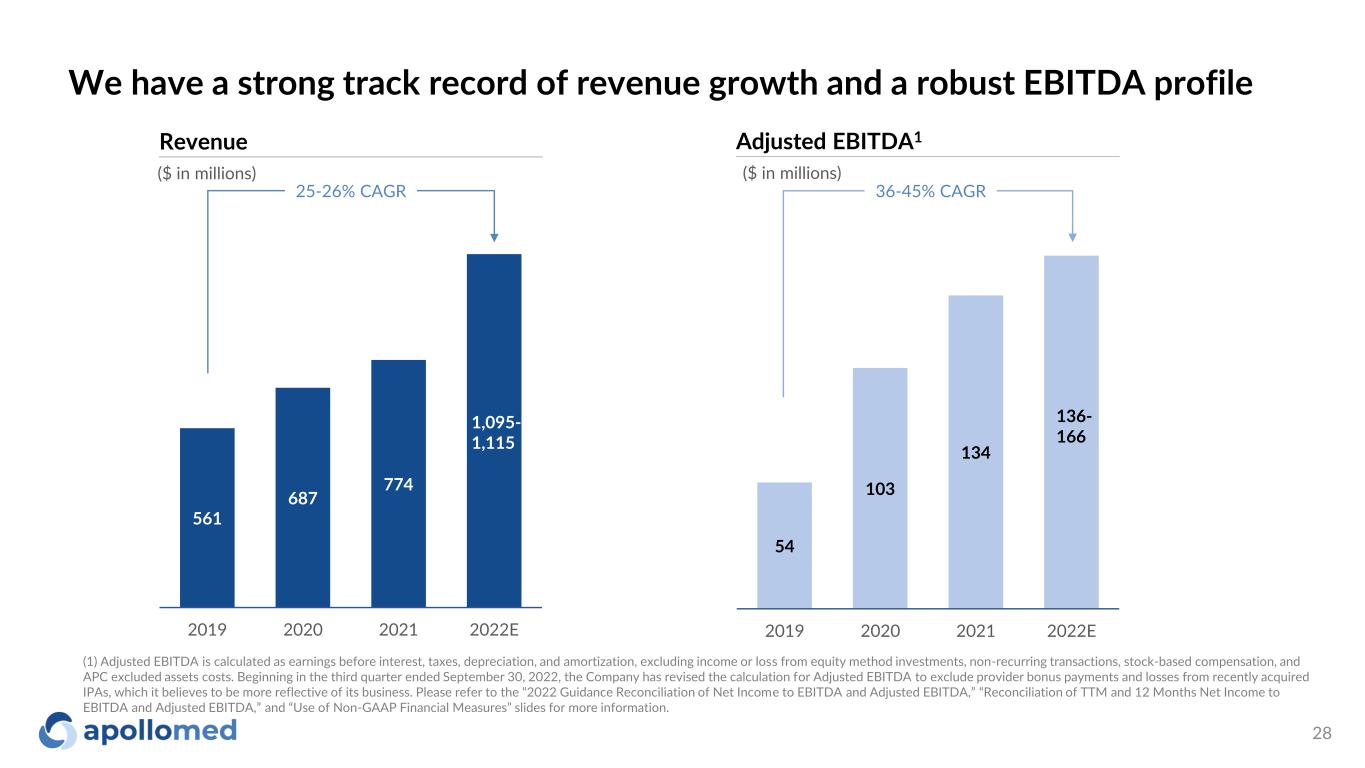
We have a strong track record of revenue growth and a robust EBITDA profile 28 ($ in millions) Revenue 25-26% CAGR ($ in millions) Adjusted EBITDA1 36-45% CAGR 1,095- 1,115 (1) Adjusted EBITDA is calculated as earnings before interest, taxes, depreciation, and amortization, excluding income or loss from equity method investments, non-recurring transactions, stock-based compensation, and APC excluded assets costs. Beginning in the third quarter ended September 30, 2022, the Company has revised the calculation for Adjusted EBITDA to exclude provider bonus payments and losses from recently acquired IPAs, which it believes to be more reflective of its business. Please refer to the “2022 Guidance Reconciliation of Net Income to EBITDA and Adjusted EBITDA,” “Reconciliation of TTM and 12 Months Net Income to EBITDA and Adjusted EBITDA,” and “Use of Non-GAAP Financial Measures” slides for more information. 561 687 774 2019 2020 2021 2022E 1,095- 1,115 54 103 134 2019 2020 2021 2022E 136- 166
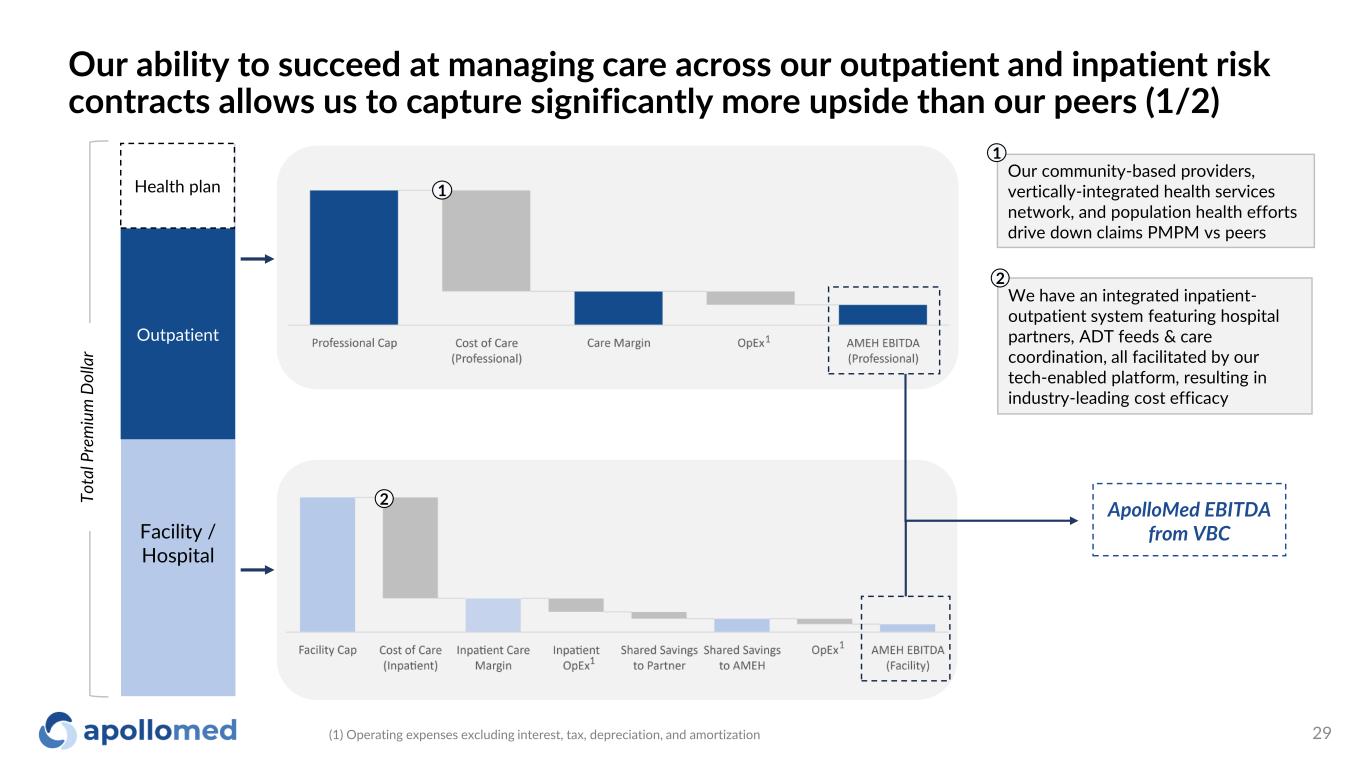
Our ability to succeed at managing care across our outpatient and inpatient risk contracts allows us to capture significantly more upside than our peers (1/2) 29 Facility / Hospital Outpatient To ta l P re m iu m D ol la r ApolloMed EBITDA from VBC We have an integrated inpatient- outpatient system featuring hospital partners, ADT feeds & care coordination, all facilitated by our tech-enabled platform, resulting in industry-leading cost efficacy 2 1 2 Health plan Our community-based providers, vertically-integrated health services network, and population health efforts drive down claims PMPM vs peers 1 1 1 (1) Operating expenses excluding interest, tax, depreciation, and amortization 1
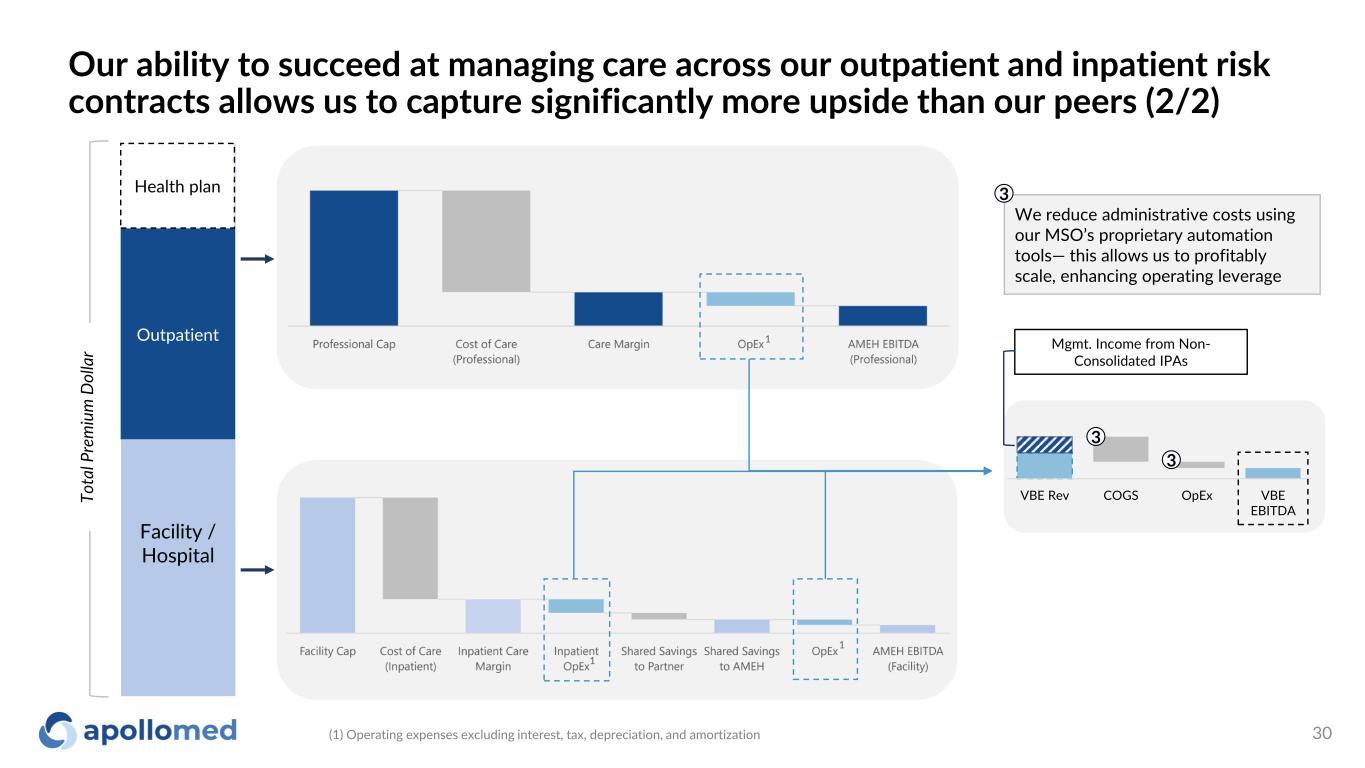
Our ability to succeed at managing care across our outpatient and inpatient risk contracts allows us to capture significantly more upside than our peers (2/2) 30 Facility / Hospital Outpatient To ta l P re m iu m D ol la r Health plan We reduce administrative costs using our MSO’s proprietary automation tools— this allows us to profitably scale, enhancing operating leverage 3 1 1 (1) Operating expenses excluding interest, tax, depreciation, and amortization 1 VBE Rev COGS OpEx VBE EBITDA 3 3 Mgmt. Income from Non- Consolidated IPAs
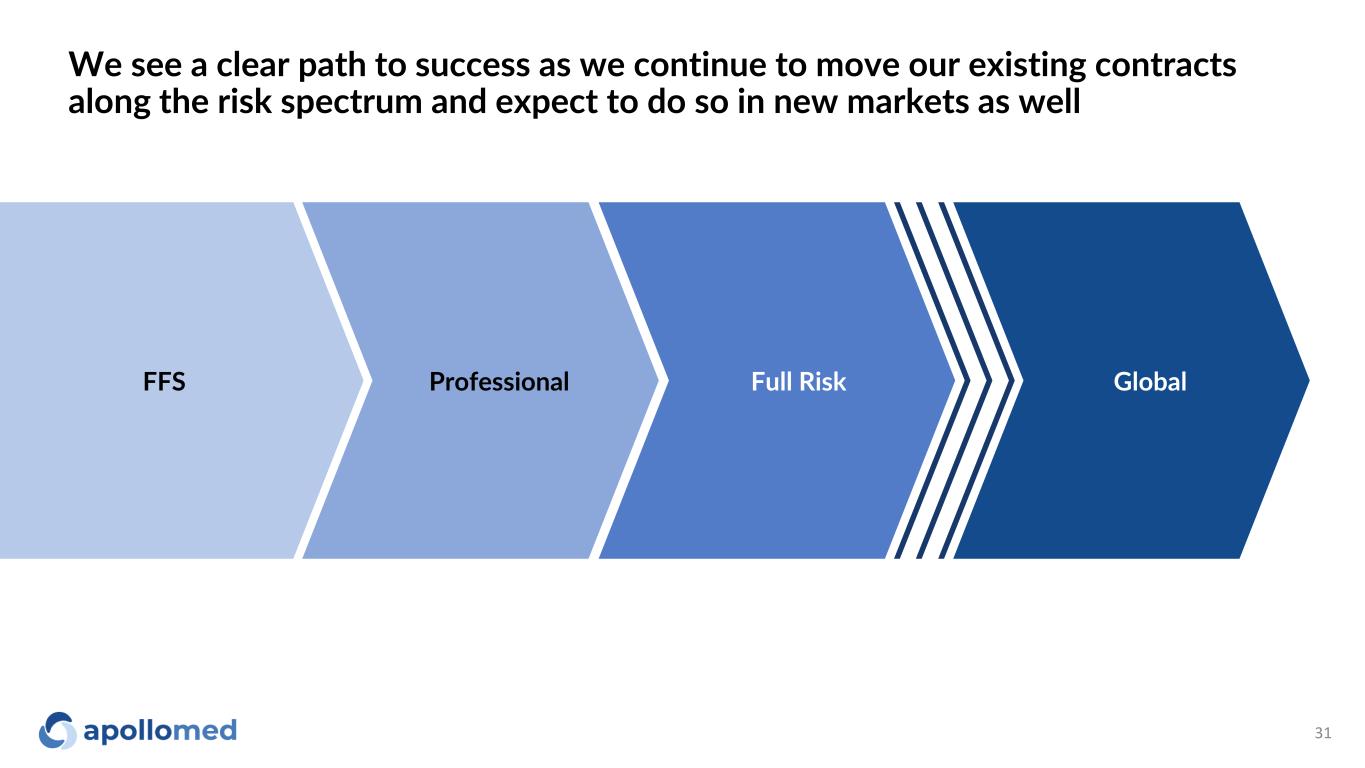
We see a clear path to success as we continue to move our existing contracts along the risk spectrum and expect to do so in new markets as well 31 FFS Professional Full Risk Global
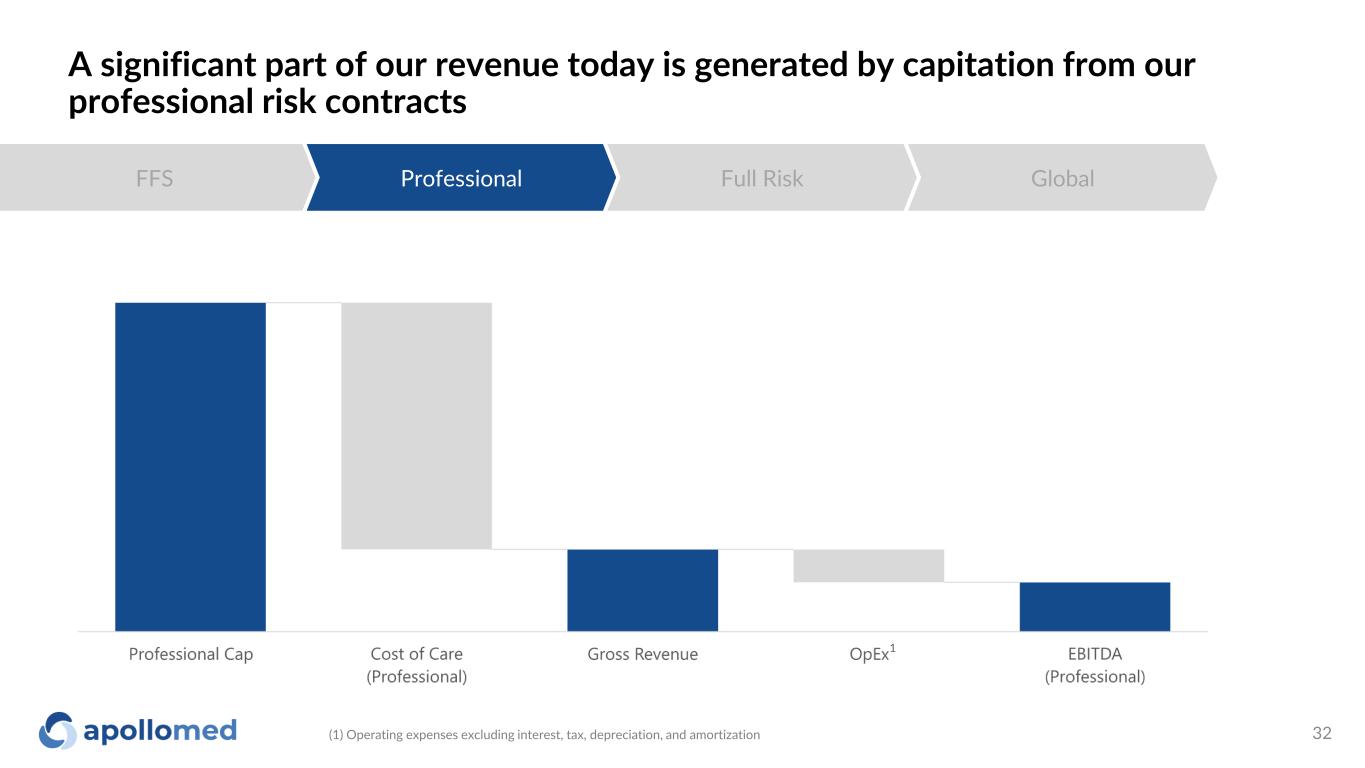
A significant part of our revenue today is generated by capitation from our professional risk contracts 32 FFS Professional Full Risk Global 1 (1) Operating expenses excluding interest, tax, depreciation, and amortization
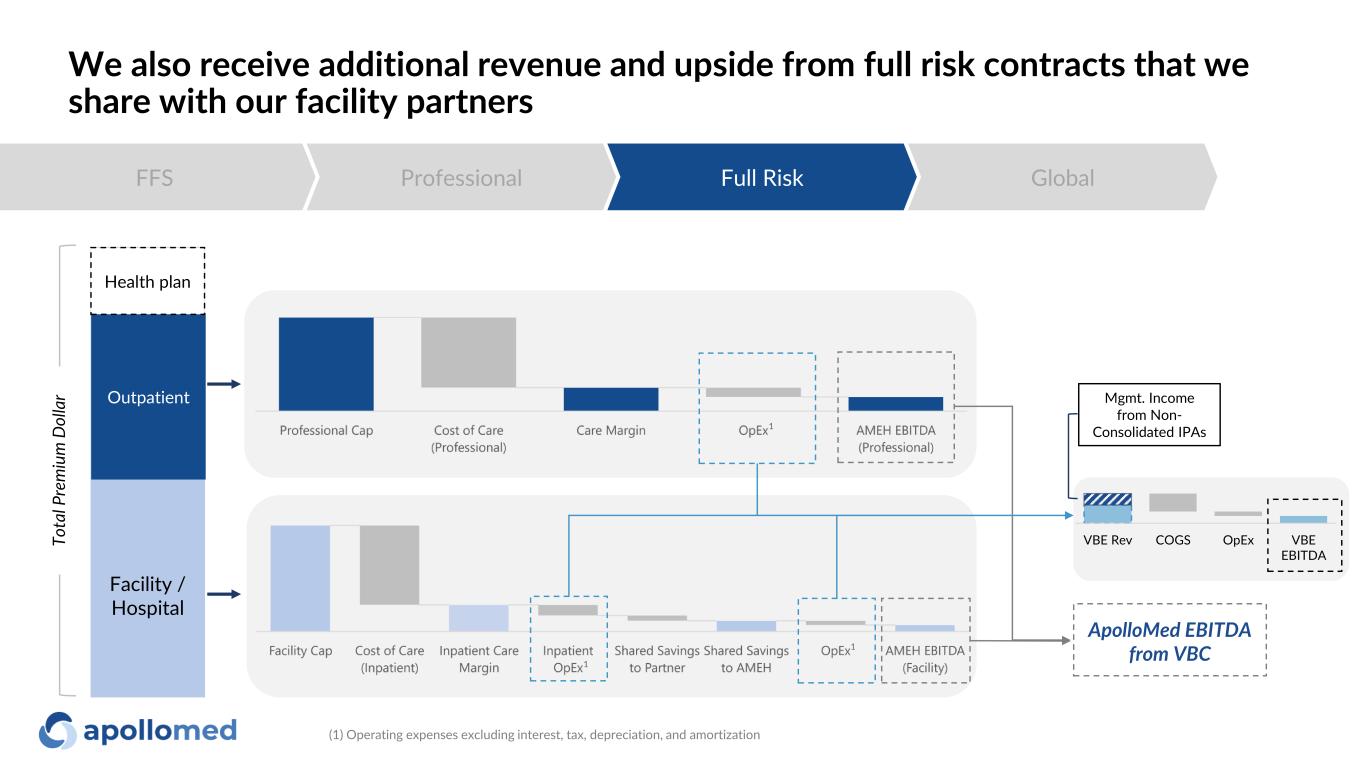
We also receive additional revenue and upside from full risk contracts that we share with our facility partners FFS Professional Full Risk Global Facility / Hospital Outpatient ApolloMed EBITDA from VBC Health plan 1 1 (1) Operating expenses excluding interest, tax, depreciation, and amortization 1 To ta l P re m iu m D ol la r VBE Rev COGS OpEx VBE EBITDA Mgmt. Income from Non- Consolidated IPAs
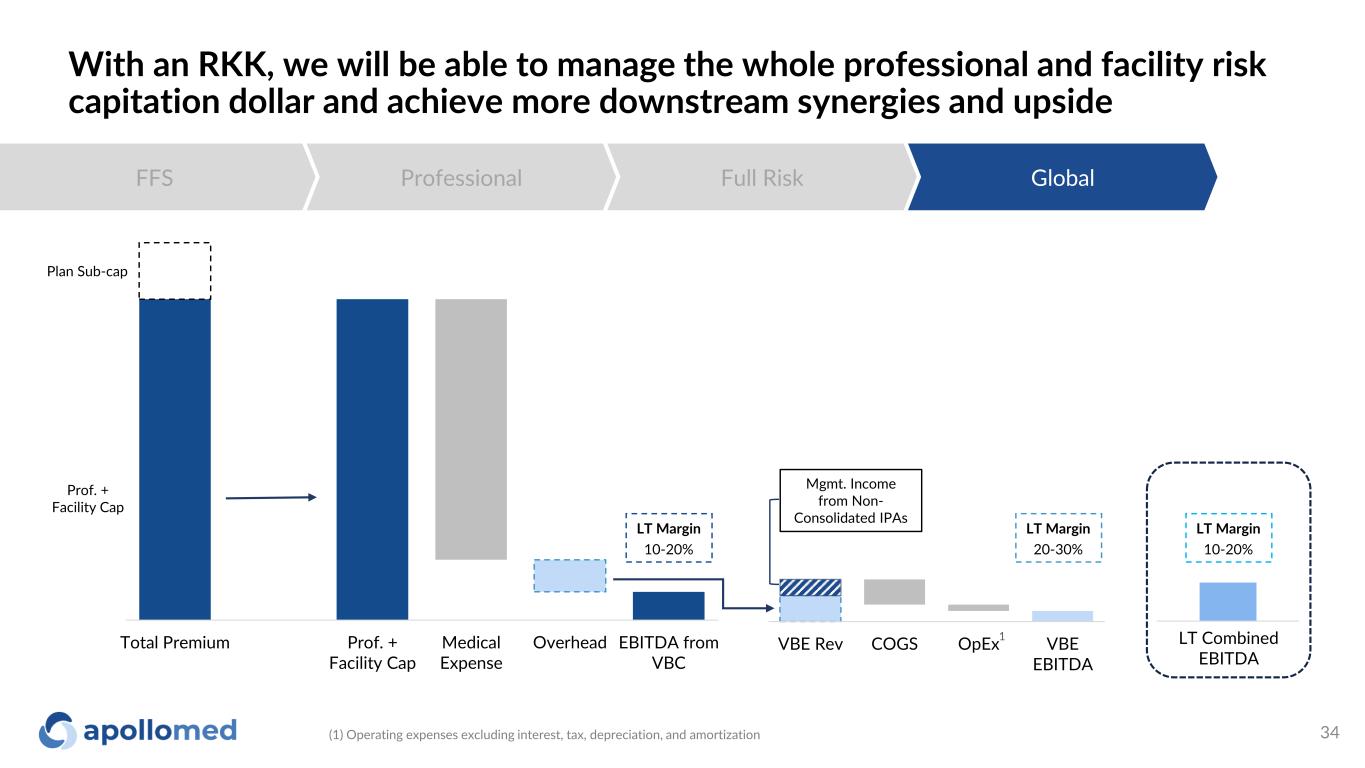
With an RKK, we will be able to manage the whole professional and facility risk capitation dollar and achieve more downstream synergies and upside 34 FFS Professional Full Risk Global Total Premium Prof. + Facility Cap Medical Expense Overhead EBITDA from VBC VBE Rev COGS OpEx VBE EBITDA Plan Sub-cap Prof. + Facility Cap LT Margin 10-20% LT Margin 20-30% LT Margin 10-20% LT Combined EBITDA Mgmt. Income from Non- Consolidated IPAs (1) Operating expenses excluding interest, tax, depreciation, and amortization 1

Conclusion
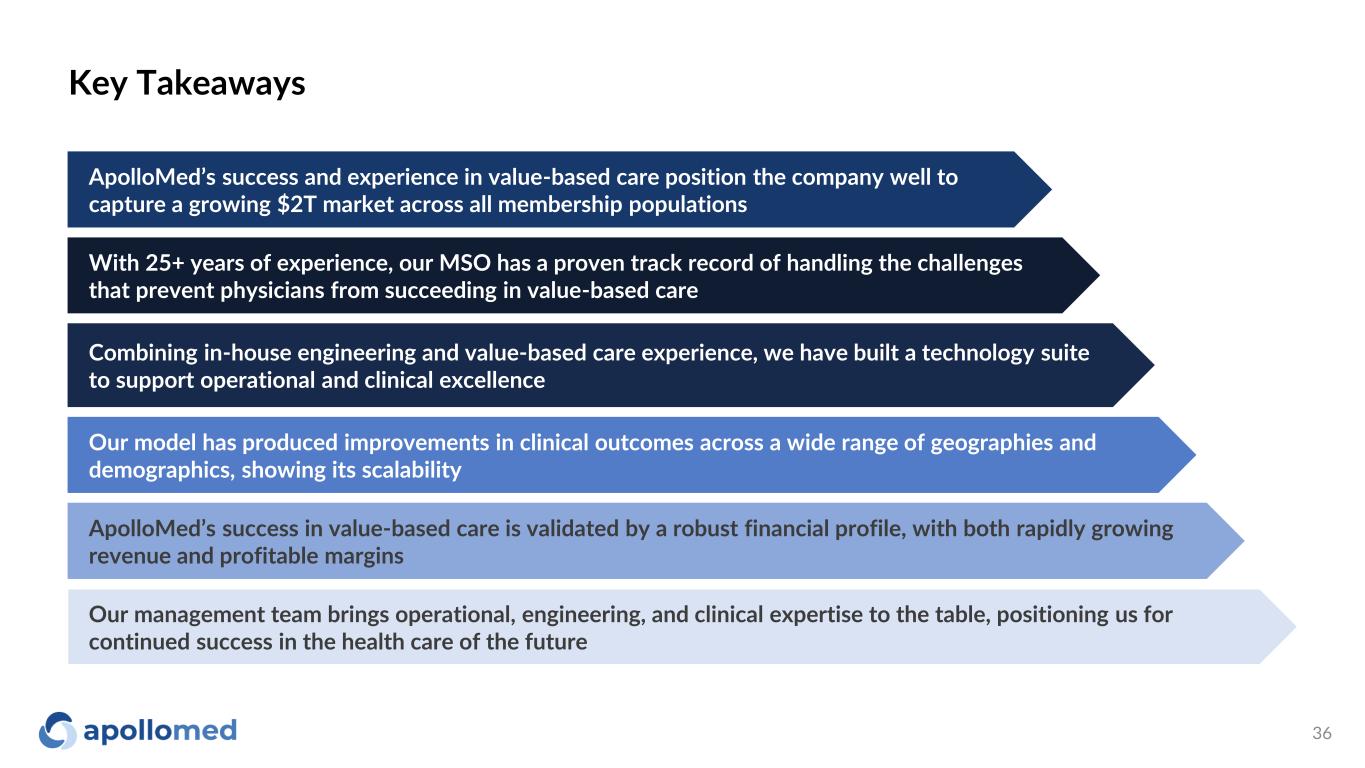
Key Takeaways 36 ApolloMed’s success and experience in value-based care position the company well to capture a growing $2T market across all membership populations With 25+ years of experience, our MSO has a proven track record of handling the challenges that prevent physicians from succeeding in value-based care Combining in-house engineering and value-based care experience, we have built a technology suite to support operational and clinical excellence Our model has produced improvements in clinical outcomes across a wide range of geographies and demographics, showing its scalability ApolloMed’s success in value-based care is validated by a robust financial profile, with both rapidly growing revenue and profitable margins Our management team brings operational, engineering, and clinical expertise to the table, positioning us for continued success in the health care of the future

Appendix

C o p y ri g h t © 2 0 2 0 b y B o st o n C o n su lt in g G ro u p . A ll r ig h ts r e se rv e d . 38 Our ApolloMed Leadership team Thomas S. Lam, MD, MPH Co-Chief Executive Officer & President Brandon Sim Co-Chief Executive Officer Chan Basho Chief Strategy Officer, Interim Chief Financial Officer Allen Hsu Chief Growth Officer Jeremy R. Jackson, MD Chief Quality Officer Albert Young, MD, MPH Chief Administrative Officer Yubin Park Chief Analytics Officer 38
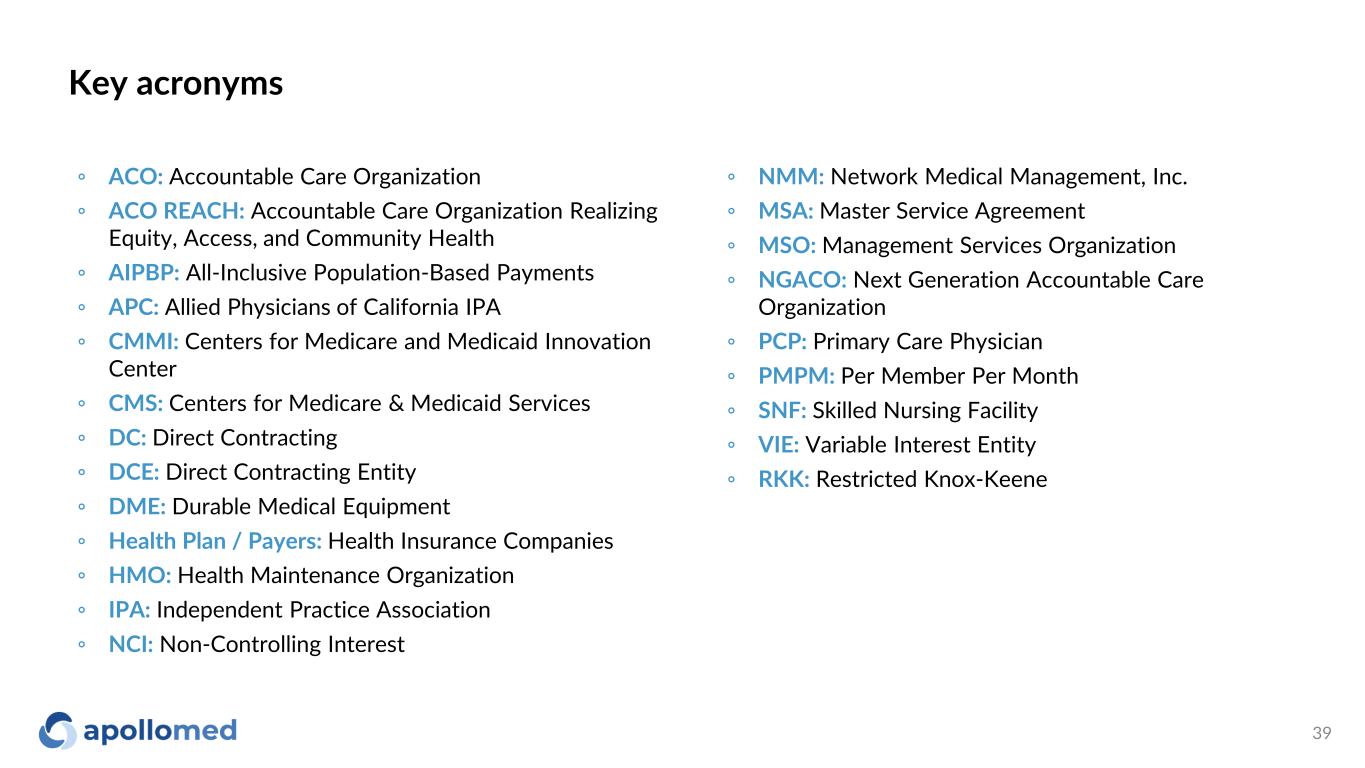
Key acronyms 39 ◦ ACO: Accountable Care Organization ◦ ACO REACH: Accountable Care Organization Realizing Equity, Access, and Community Health ◦ AIPBP: All-Inclusive Population-Based Payments ◦ APC: Allied Physicians of California IPA ◦ CMMI: Centers for Medicare and Medicaid Innovation Center ◦ CMS: Centers for Medicare & Medicaid Services ◦ DC: Direct Contracting ◦ DCE: Direct Contracting Entity ◦ DME: Durable Medical Equipment ◦ Health Plan / Payers: Health Insurance Companies ◦ HMO: Health Maintenance Organization ◦ IPA: Independent Practice Association ◦ NCI: Non-Controlling Interest ◦ NMM: Network Medical Management, Inc. ◦ MSA: Master Service Agreement ◦ MSO: Management Services Organization ◦ NGACO: Next Generation Accountable Care Organization ◦ PCP: Primary Care Physician ◦ PMPM: Per Member Per Month ◦ SNF: Skilled Nursing Facility ◦ VIE: Variable Interest Entity ◦ RKK: Restricted Knox-Keene
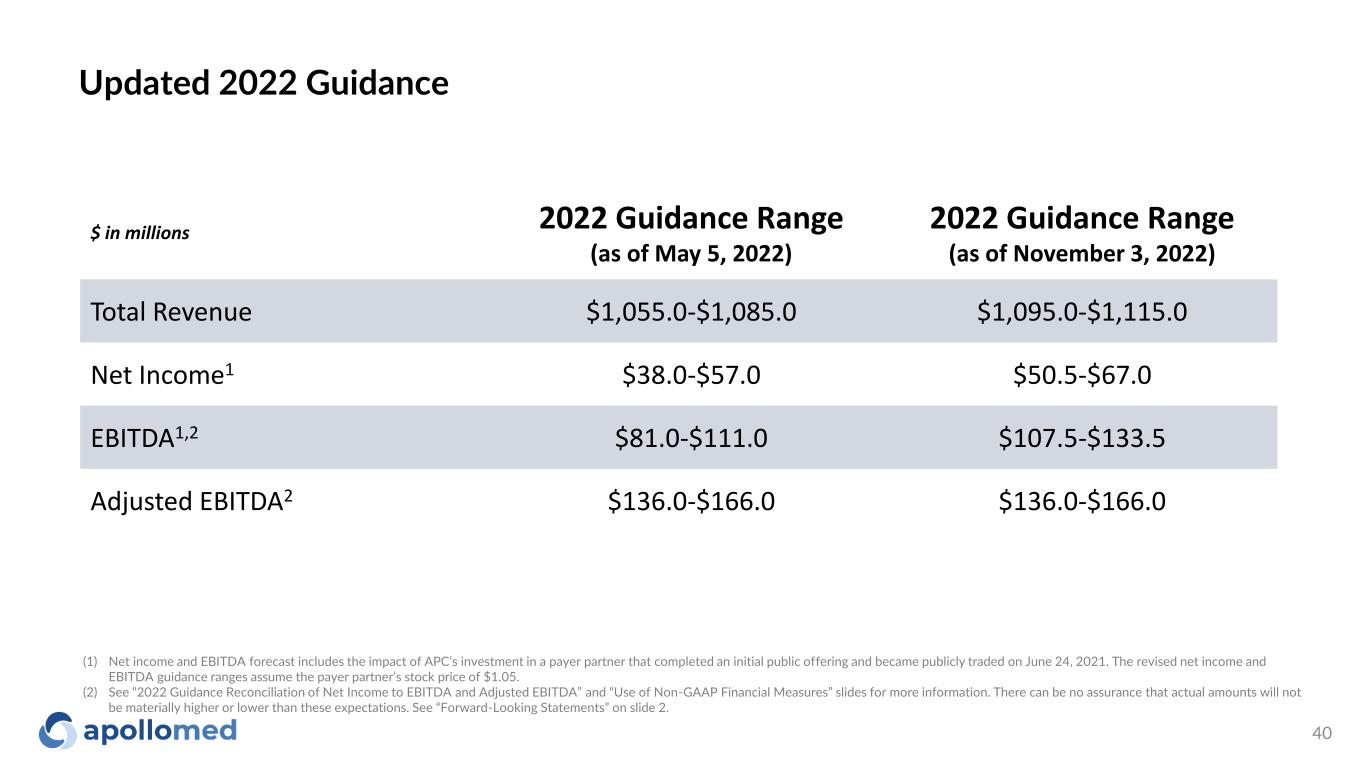
40 $ in millions 2022 Guidance Range (as of May 5, 2022) 2022 Guidance Range (as of November 3, 2022) Total Revenue $1,055.0-$1,085.0 $1,095.0-$1,115.0 Net Income1 $38.0-$57.0 $50.5-$67.0 EBITDA1,2 $81.0-$111.0 $107.5-$133.5 Adjusted EBITDA2 $136.0-$166.0 $136.0-$166.0 Updated 2022 Guidance (1) Net income and EBITDA forecast includes the impact of APC’s investment in a payer partner that completed an initial public offering and became publicly traded on June 24, 2021. The revised net income and EBITDA guidance ranges assume the payer partner’s stock price of $1.05. (2) See “2022 Guidance Reconciliation of Net Income to EBITDA and Adjusted EBITDA” and “Use of Non-GAAP Financial Measures” slides for more information. There can be no assurance that actual amounts will not be materially higher or lower than these expectations. See “Forward-Looking Statements” on slide 2.
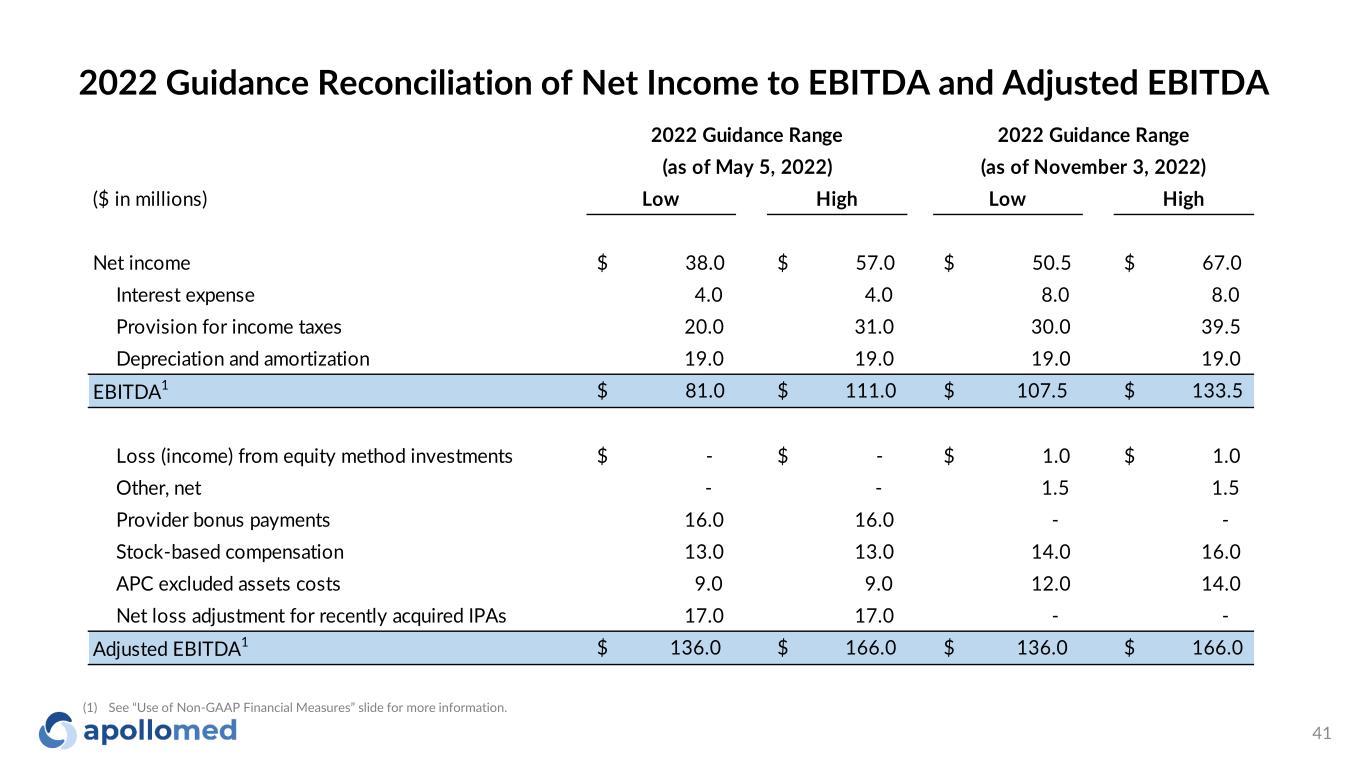
41 ($ in millions) Low High Low High Net income $ 38.0 $ 57.0 $ 50.5 $ 67.0 Interest expense 4.0 4.0 8.0 8.0 Provision for income taxes 20.0 31.0 30.0 39.5 Depreciation and amortization 19.0 19.0 19.0 19.0 EBITDA1 $ 81.0 $ 111.0 $ 107.5 $ 133.5 Loss (income) from equity method investments $ - $ - $ 1.0 $ 1.0 Other, net - - 1.5 1.5 Provider bonus payments 16.0 16.0 - - Stock-based compensation 13.0 13.0 14.0 16.0 APC excluded assets costs 9.0 9.0 12.0 14.0 Net loss adjustment for recently acquired IPAs 17.0 17.0 - - Adjusted EBITDA1 $ 136.0 $ 166.0 $ 136.0 $ 166.0 2022 Guidance Range (as of May 5, 2022) 2022 Guidance Range (as of November 3, 2022) 2022 Guidance Reconciliation of Net Income to EBITDA and Adjusted EBITDA (1) See “Use of Non-GAAP Financial Measures” slide for more information.
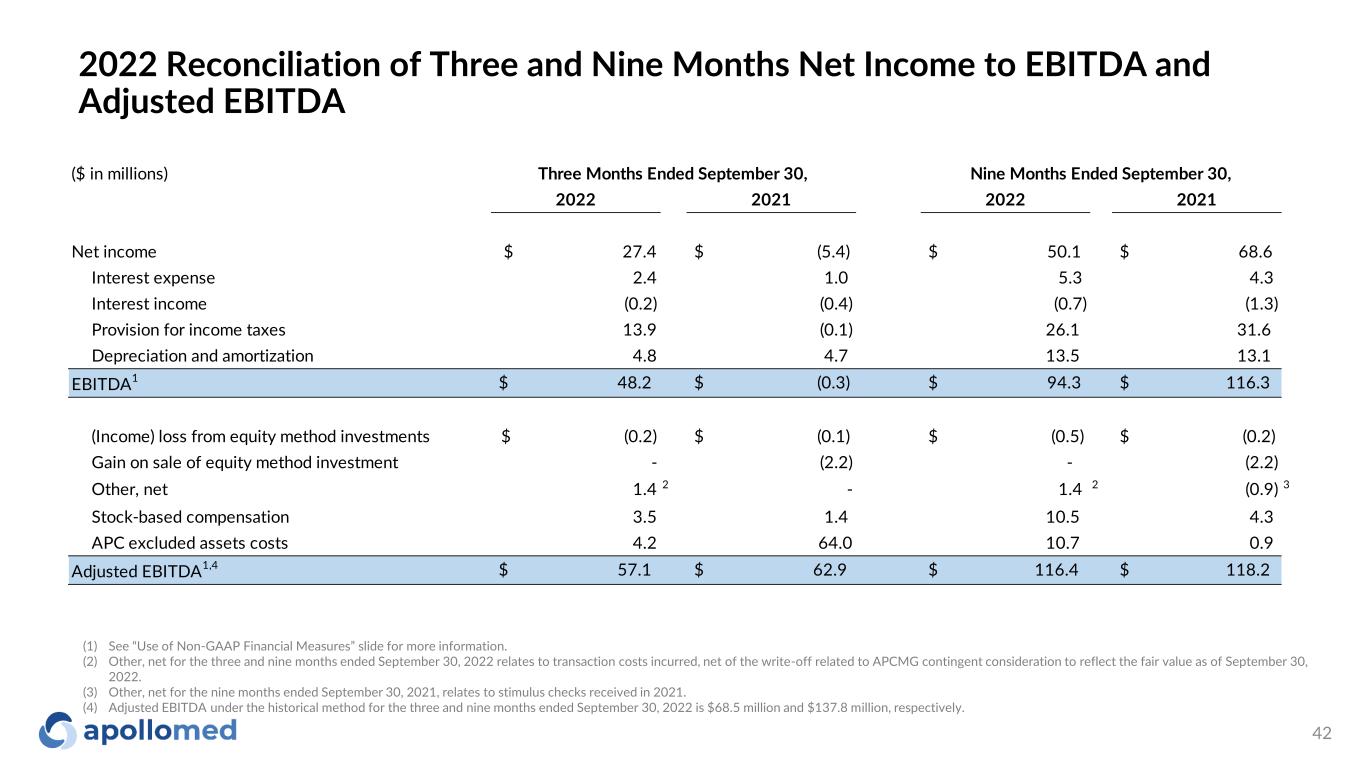
($ in millions) 2022 2021 2022 2021 Net income $ 27.4 $ (5.4) $ 50.1 $ 68.6 Interest expense 2.4 1.0 5.3 4.3 Interest income (0.2) (0.4) (0.7) (1.3) Provision for income taxes 13.9 (0.1) 26.1 31.6 Depreciation and amortization 4.8 4.7 13.5 13.1 EBITDA1 $ 48.2 $ (0.3) $ 94.3 $ 116.3 (Income) loss from equity method investments $ (0.2) $ (0.1) $ (0.5) $ (0.2) Gain on sale of equity method investment - (2.2) - (2.2) Other, net 1.4 2 - 1.4 2 (0.9) 3 Stock-based compensation 3.5 1.4 10.5 4.3 APC excluded assets costs 4.2 64.0 10.7 0.9 Adjusted EBITDA1,4 $ 57.1 $ 62.9 $ 116.4 $ 118.2 Three Months Ended September 30, Nine Months Ended September 30, 42 2022 Reconciliation of Three and Nine Months Net Income to EBITDA and Adjusted EBITDA (1) See “Use of Non-GAAP Financial Measures” slide for more information. (2) Other, net for the three and nine months ended September 30, 2022 relates to transaction costs incurred, net of the write-off related to APCMG contingent consideration to reflect the fair value as of September 30, 2022. (3) Other, net for the nine months ended September 30, 2021, relates to stimulus checks received in 2021. (4) Adjusted EBITDA under the historical method for the three and nine months ended September 30, 2022 is $68.5 million and $137.8 million, respectively.
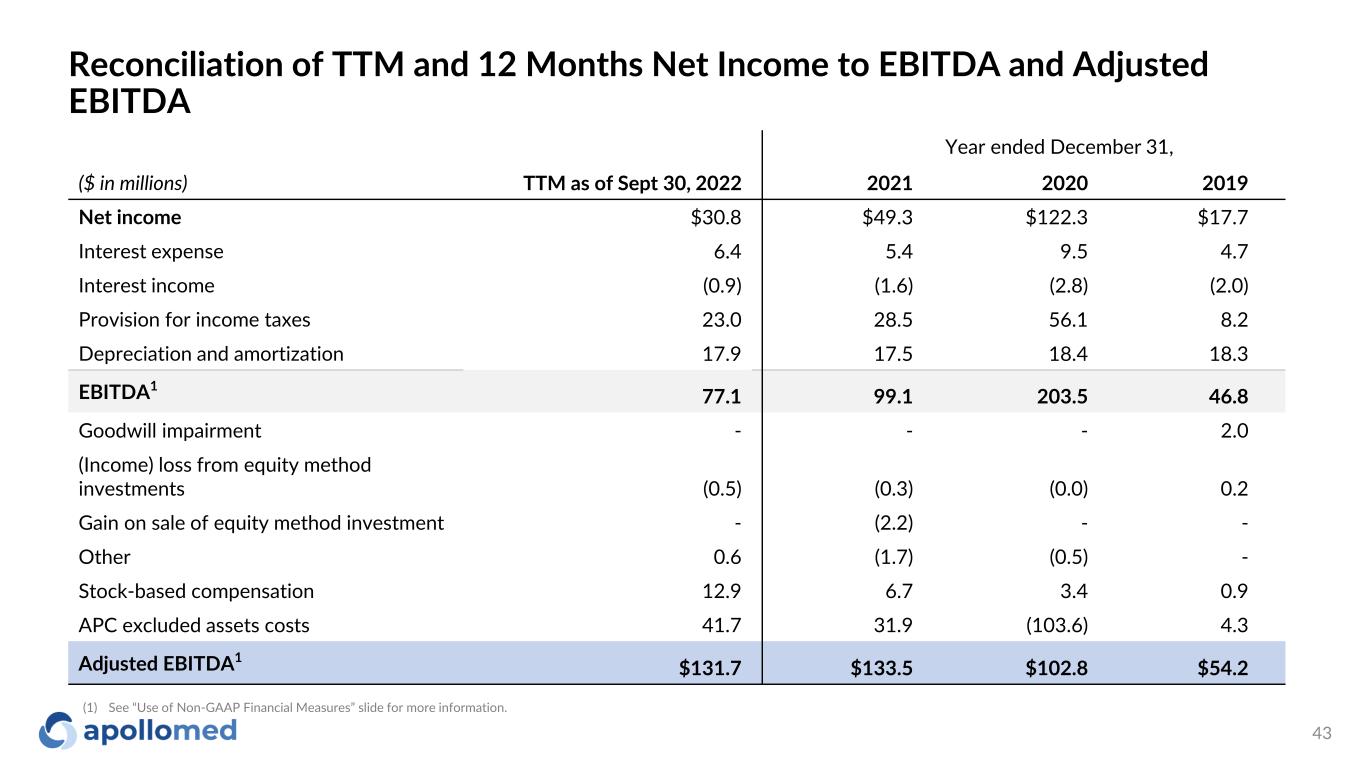
Reconciliation of TTM and 12 Months Net Income to EBITDA and Adjusted EBITDA 43 Year ended December 31, ($ in millions) TTM as of Sept 30, 2022 2021 2020 2019 Net income $30.8 $49.3 $122.3 $17.7 Interest expense 6.4 5.4 9.5 4.7 Interest income (0.9) (1.6) (2.8) (2.0) Provision for income taxes 23.0 28.5 56.1 8.2 Depreciation and amortization 17.9 17.5 18.4 18.3 EBITDA1 77.1 99.1 203.5 46.8 Goodwill impairment - - - 2.0 (Income) loss from equity method investments (0.5) (0.3) (0.0) 0.2 Gain on sale of equity method investment - (2.2) - - Other 0.6 (1.7) (0.5) - Stock-based compensation 12.9 6.7 3.4 0.9 APC excluded assets costs 41.7 31.9 (103.6) 4.3 Adjusted EBITDA1 $131.7 $133.5 $102.8 $54.2 (1) See “Use of Non-GAAP Financial Measures” slide for more information.
Use of Non-GAAP Financial Measures 44 This presentation contains the non-GAAP financial measures EBITDA and adjusted EBITDA, of which the most directly comparable financial measure presented in accordance with U.S. generally accepted accounting principles (“GAAP”) is net (loss) income. These measures are not in accordance with, or an alternative to, GAAP, and may be different from other non-GAAP financial measures used by other companies. The Company uses adjusted EBITDA as a supplemental performance measure of the Company’s operations, for financial and operational decision-making, and as a supplemental means of evaluating period-to-period comparisons on a consistent basis. Adjusted EBITDA is calculated as earnings before interest, taxes, depreciation, and amortization, excluding income from equity method investments, provider bonuses, stock-based compensation, APC excluded assets costs, impairment of intangibles, provision of doubtful accounts, and other income earned that is not related to the Company’s normal operations. Adjusted EBITDA also excludes non-recurring items, including the effect on EBITDA of certain recently acquired IPAs. The Company believes the presentation of these non-GAAP financial measures provides investors with relevant and useful information, as it allows investors to evaluate the operating performance of the business activities without having to account for differences recognized because of non-core or non-recurring financial information. When GAAP financial measures are viewed in conjunction with non-GAAP financial measures, investors are provided with a more meaningful understanding of the Company’s ongoing operating performance. In addition, these non-GAAP financial measures are among those indicators the Company uses as a basis for evaluating operational performance, allocating resources, and planning and forecasting future periods. Non-GAAP financial measures are not intended to be considered in isolation from, or as a substitute for, GAAP financial measures. To the extent this release contains historical or future non-GAAP financial measures, the Company has provided corresponding GAAP financial measures for comparative purposes. The reconciliation between certain GAAP and non-GAAP measures is provided above.

For inquiries, please contact: ApolloMed Investor Relations (626) 943-6491 investors@apollomed.net Carolyne Sohn, The Equity Group (408) 538-4577 csohn@equityny.com